The most important intervention in any urgent or emergent situation is securing the airway and ensuring adequate ventilation. The key points are call for help as soon as possible and always use the simplest possible intervention. By following these guidelines, the average healthcare provider has the potential to make a tremendous impact on the patient's disease or injury and ensure that the patient survives long enough to receive definitive care. The information presented in this course will help anyone address patients' airway problems in an efficient and effective fashion.
This course is designed for dental professionals involved in monitoring and maintaining patients' airways.
Gaining control of the airway in a compromised patient is absolutely crucial. The purpose of this course is to provide dental professionals with the clinical knowledge needed to rapidly and effectively assess the patient's airway and intervene efficiently to begin to ventilate the patient in distress.
Upon completion of this course, you should be able to:
- Outline the pertinent history of airway management.
- Review the anatomy and physiology of the mouth, oropharynx, nose, nasopharynx, and conducting airways of the lung.
- Distinguish between the terms dead space and shunt, and explain how they can be altered.
- Review the gas laws and determine the amount of oxygen being sent to the alveoli when the airway is managed.
- Discuss the assessment of a patient prior to airway management.
- Describe steps to manipulate the airway of a patient in respiratory distress.
- Compare and contrast various devices available for airway management.
Richard E. Haas, BSN, MSN, EdM, PhD, CRNA, LTC US Army Nurse Corps (Retired), is a retired nurse anesthetist and prehospital registered nurse (instructor) who has published extensively in various areas of healthcare research while providing clinical care in arenas ranging from academic medical centers to austere environments in the third world during both wartime and peacetime. He has a bachelor’s degree in nursing from Georgetown University, Master’s degrees in education (Boston University) and nursing specializing in anesthesia (State University of New York in Buffalo and U.S. Army), and a PhD from the University of South Carolina. He is a retired lieutenant colonel in the U.S. Army Nurse Corps. He has taught nursing anesthesia, pharmacology, and physiology; mentored students in doctoral programs; and used advanced patient simulation to train students. Dr. Haas has worked in clinical, administrative, education, and research roles. He continues to work as an independent consultant, while taking more time to enjoy life with his wife of nearly 50 years and their children and grandchildren.
Contributing faculty, Richard E. Haas, BSN, MSN, EdM, PhD, CRNA, LTC US Army Nurse Corps (Retired), has disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
Mark J. Szarejko, DDS, FAGD
The division planner has disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
Sarah Campbell
The Director of Development and Academic Affairs has disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
The purpose of NetCE is to provide challenging curricula to assist healthcare professionals to raise their levels of expertise while fulfilling their continuing education requirements, thereby improving the quality of healthcare.
Our contributing faculty members have taken care to ensure that the information and recommendations are accurate and compatible with the standards generally accepted at the time of publication. The publisher disclaims any liability, loss or damage incurred as a consequence, directly or indirectly, of the use and application of any of the contents. Participants are cautioned about the potential risk of using limited knowledge when integrating new techniques into practice.
It is the policy of NetCE not to accept commercial support. Furthermore, commercial interests are prohibited from distributing or providing access to this activity to learners.
Supported browsers for Windows include Microsoft Internet Explorer 9.0 and up, Mozilla Firefox 3.0 and up, Opera 9.0 and up, and Google Chrome. Supported browsers for Macintosh include Safari, Mozilla Firefox 3.0 and up, Opera 9.0 and up, and Google Chrome. Other operating systems and browsers that include complete implementations of ECMAScript edition 3 and CSS 2.0 may work, but are not supported. Supported browsers must utilize the TLS encryption protocol v1.1 or v1.2 in order to connect to pages that require a secured HTTPS connection. TLS v1.0 is not supported.
The role of implicit biases on healthcare outcomes has become a concern, as there is some evidence that implicit biases contribute to health disparities, professionals' attitudes toward and interactions with patients, quality of care, diagnoses, and treatment decisions. This may produce differences in help-seeking, diagnoses, and ultimately treatments and interventions. Implicit biases may also unwittingly produce professional behaviors, attitudes, and interactions that reduce patients' trust and comfort with their provider, leading to earlier termination of visits and/or reduced adherence and follow-up. Disadvantaged groups are marginalized in the healthcare system and vulnerable on multiple levels; health professionals' implicit biases can further exacerbate these existing disadvantages.
Interventions or strategies designed to reduce implicit bias may be categorized as change-based or control-based. Change-based interventions focus on reducing or changing cognitive associations underlying implicit biases. These interventions might include challenging stereotypes. Conversely, control-based interventions involve reducing the effects of the implicit bias on the individual's behaviors. These strategies include increasing awareness of biased thoughts and responses. The two types of interventions are not mutually exclusive and may be used synergistically.
#50010: Airway Management: Basics for Healthcare Providers
Nearly everyone involved in health care has been exposed to the ABCs of airway, breathing, and circulation during their training; it has been an essential aspect of patient assessment and care. More recently, this has been expanded to include disability and exposure (ABCDE). This course will provide a review of the airway and breathing aspects of the ABCs and describe the simple techniques that can make the difference between life and death for patients. Whether it is something as simple as tilting the chin or as complex as video laryngoscopy, gaining control of the airway in a compromised patient is absolutely crucial. Failing to quickly and easily manage the airway and, when necessary, ventilate the patient, renders all other subsequent interventions futile.
While airway management seems basic, the average practitioner has limited exposure to opening the patient's airway to insure ventilation. In most instruction, there is an emphasis on equipment when, in fact, clinicians should begin with the simplest technique, only moving to more complex interventions when absolutely needed or in the absence of the imminent arrival of a skilled airway provider.
The purpose of this course is to provide practitioners, whether in the clinic, the intensive care unit, the emergency room, or in the community as a prehospital provider, with the clinical knowledge needed to rapidly and effectively assess the patient's airway and intervene efficiently to begin to ventilate the patient in distress. This includes practitioners who are not normally seen as being involved with airway management, such as dental professionals, mental health providers, and allied staff. Further, as practitioners may be called upon to provide ABC assessment and care outside the controlled environment of the hospital or clinic, a significant portion of this course will focus on how to be successful in airway management with a minimum of equipment prior to the arrival of designated advanced care providers.
Airway management is in a constant state of improvement and change. As might be expected, surgical tracheostomy, albeit not under the best conditions, was the first attempt to manipulate the airway in the presence of trauma or obstruction. The first recorded use of an artificial airway was described in 2000 B.C.E. in India, with a description of the healing of a post-tracheostomy wound [1]. Further descriptions came in the period of 400 to 300 B.C.E. from the Greek physician Hippocrates and Greek "first responder" and conqueror Alexander the Great, who reportedly performed a field-expedient tracheostomy with his sword on a fellow soldier who was suffocating on an aspirated bone around 320 B.C.E. [1]. Tracheostomy continued as the technique of choice, though the insertion of a hollow reed in the trachea of a newborn is described as early as 400 C.E. [1]. A lack of understanding that air needed to be pumped through the trachea limited the usefulness of tracheostomy, except in those patients already able to breathe. This limited usefulness is despite the fact that as early as 200 C.E., the Greek physician Galen used bellows attached to the trachea to mechanically move air into and out of the lungs. One author notes that between the years of 1546, when the Italian surgeon Brassavola first published an account of surgical tracheostomy, and 1825, only 28 cases of recovery from the underlying illness or trauma were reported [1,2]. The Renaissance brought new and innovative techniques and ideas relating to patient care, especially in the areas of airway management and ventilatory support. Andreas Vesalius, noted anatomist and physician of the 16th century, described the insertion of a reed into the tracheae of animals he was dissecting to better understand the physiologic interactions between the heart and lungs [3]. Work such as this led the Italian physician Fabricius of Acquapendente to write the following [3]:
Of all the surgical operations which are performed in man . . . the foremost [is] that by which man is recalled from a quick death to a sudden repossession of life . . . the operation is the opening of the aspera arteria ["artery of air" or trachea], by which patients, from a condition of almost suffocating obstruction to respiration, suddenly regain consciousness, and draw that vital ether, the air, so necessary to life, and again resume an existence which had been all but annihilated.
Clearly, physicians of the Renaissance had a greater appreciation for the importance of the airway, and its rapid management, to the sustainment of life. Through the 1600s and 1700s, tracheostomy continued to be performed for various types of pathologic or mechanical obstructions of the trachea. It was not, however, entered into without considerable trepidation and misgivings on the part of the surgeons and physicians performing the procedure, just as interventions with the airways continue to be approached cautiously. In Priest's study on tracheostomy, he quotes the French physician DeGarangeot, who states [3]:
The operation is very dangerous. Few authors say they have performed it, and fewer still that it proved successful. The reason of it seems to be because they perform it too late, and when the patient is dangerously sick.
This statement from 1720 seems to be a prophetic vision of the "golden hour" familiar to practitioners today. From the period of the 1700s through the early 1900s, tracheostomy remained the primary technique for emergency airway management, though some changes in the development of endotracheal intubation were beginning to come into use. In 1871 came the first reported instance of endotracheal intubation, followed by the development of metal endotracheal tubes in 1875 [1]. The increased lethality and deployment of weapons in World War I resulted in increasing numbers of head, face, and neck injuries due to shrapnel or gunshot wounds. Endotracheal intubation was seen as the criterion standard in securing the airway to operate on these patients [4]. Sir Ivan Magill, a British medical officer and anesthetist, pioneered the use of wide bore, uncuffed rubber tubes, and Dr. Arthur Guedel introduced the Guedel laryngoscope [4]. By World War II, field anesthesia machines to provide positive pressure ventilation, delivered via an endotracheal tube, were available but used primarily for chest and lung cases [5]. Mask ventilation and allowing the patient to breathe spontaneously while the anatomic airway was held open by the anesthetist was common. Guedel airways, now known as oropharyngeal airways, were also used to simplify keeping the patient's airway open. In the Korean and, to a greater extent, Vietnam conflicts, the routine use of helicopter evacuation resulted in more patients getting to field surgical units, during which endotracheal intubation could be performed in the operating room, as adequate ventilation was deemed a precursor to all other forms of care [6]. The skills learned during the Vietnam War were rapidly transferred to civilian practices in America as the war ended. The advanced airway skills learned by combat medics impacted the development of paramedics as prehospital providers. Interestingly, it was the 1970s television show Emergency!, an action drama featuring firefighter paramedics in Los Angeles, that has been identified as a driver of improvements in prehospital care [7]. The program at that time was one of the most-watched shows in the United States [8]. One of the characters was a former Army medic who had served in Vietnam. Communities across the United States began to wonder why their emergency responders were different from those on the Emergency! television series [8]. Airway management soon was a pivotal part of prehospital care. The entry of the United States into the Persian Gulf War and wars in Iraq and Afghanistan have further increased the technologic advances in all areas of trauma and health care. It is not uncommon for a wounded soldier to have lifesaving surgery within minutes of being injured, followed by tertiary care stabilization stateside within 24 to 36 hours. These long transports require similar advances in airway and ventilatory management.
As we advance into the 21st century, increases in technology and education of practitioners allow for the treatment of patients receiving complex surgery in the presence of multi-organ dysfunction. Frequently, patients receiving these procedures must be mechanically ventilated. In hospitals, the introduction of more advanced ventilators and complex airway management techniques has increased the number of patients benefiting from airway management.
To manage the airway, healthcare providers require a good working knowledge of the anatomy of the mouth, oropharynx, nose, nasopharynx, and glottic opening. Further, while emergency airway management "opens the door" to saving the patient's life, a knowledge of the conducting and respiratory airways of the lungs, as well as the ability to adequately ventilate the lungs, is a crucial part of saving the patient's life. The following section will work using a "top-to-bottom" approach, beginning with the mouth and nose and ending in the alveoli.
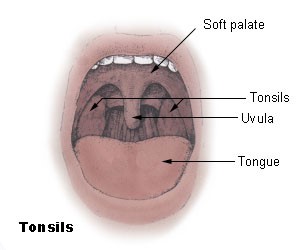
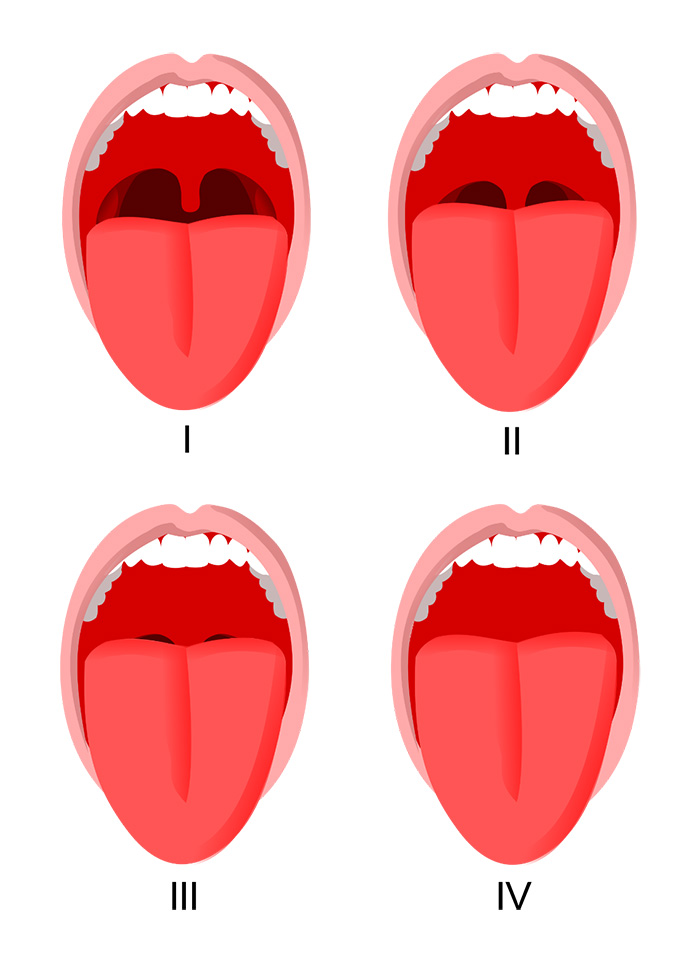
Figure 1 is a representation of the open mouth. This seems basic, yet, in many instances, the basics are overlooked. Note the presence of the tongue, one of the biggest culprits when it comes to obstructing the airways. In many instances, simply displacing the tongue from the posterior of the oral airway is sufficient to allow the patient to breathe. Air enters the mouth and nose first and then descends down the conducting airways to the respiratory airways. One of the primary purposes of the nose and mouth and other upper airway structures is to warm and humidify the air the patient breathes before it enters the trachea and other conducting airways. As this is the case, these upper airway structures are both highly innervated and highly vascular. The mouth is innervated by branches V2 and V3 of cranial nerve (CN) V, the trigeminal nerve [9]. The high degree of innervation means that any manipulation of the upper airway in the mouth, no matter how slight, can precipitate gagging, retching, and in the worst case, vomiting. This is an adaptive mechanism, as objects entering the airway may occlude it, resulting in asphyxiation. The presence of high vascularity means that failure to use care in manipulating the upper airway may result in bleeding, further compromising a patient with airway management problems. One should always engage the minimum amount of intervention needed to open the patient's airway in an effort to decrease the potential for traumatization of the airway. More about the nervous innervation of the airway will be presented later in this course.
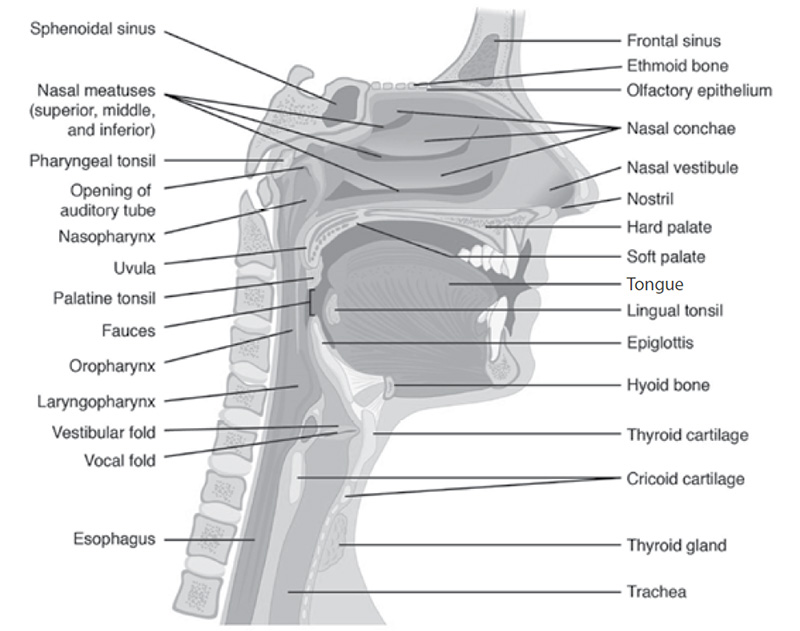
Figure 2 shows a lateral cross-section of the head and tracks the mouth and nose to the oropharynx and nasopharynx. Note the extensive number of structures.
The nasal cavity is quite similar in function to the mouth (warming and humidifying the air) and well innervated by the trigeminal nerve (CN V) through branches V1 and V2, though less likely to promote a gag reflex when stimulated [9]. Rapid or careless insertion of a nasal airway device, particularly in the absence of some form of lubricant, may result in profound bleeding, referred to as epistaxis. Epistaxis ordinarily responds well to direct pressure in the nose; however, some cases are sufficiently serious as to require surgical intervention. Note that the floor of the nasal cavity covers the hard and soft palate and is nearly parallel to the ground when a patient stands upright on a flat surface. This is important to know when attempting to pass any form of nasal airway device. This will be explored further in the section on nasal devices, but for now it is important to remember the flat nature of this structure.
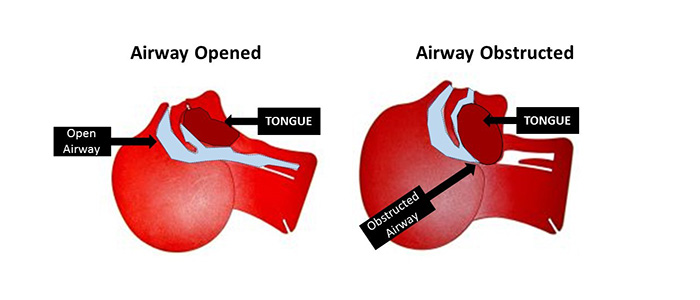
As one traces from the nose and mouth openings toward the back of the head, the oropharynx and nasopharynx are found. This is the first stop in managing supraglottic or pharyngeal obstructions of the airway. As the name implies, supraglottic obstructions appear superior (or above) the epiglottis and glottic opening. The oropharynx and nasopharynx are important when managing the airways for two reasons: this area is ordinarily occluded by the tongue in patients with decreased levels of consciousness, and the two easiest devices for airway management (the oropharyngeal airway and the nasopharyngeal airway) are used here. These areas are innervated by CN IX, the glossopharyngeal nerve [10]. The nasopharynx has less innervation, and this results in nasopharyngeal airways being better tolerated by conscious and semi-conscious patients compared with oropharyngeal airways. Not only is the oropharynx more deeply innervated by CN IX, it is also partially innervated by CN X (vagus nerve), particularly at the base of the tongue [10]. Figure 3 shows a lateral view of the airway in both the open and obstructed condition.
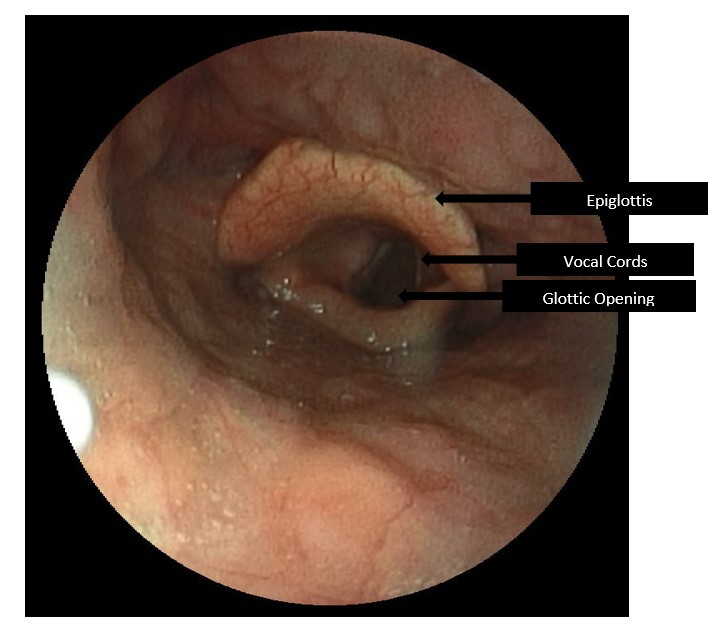
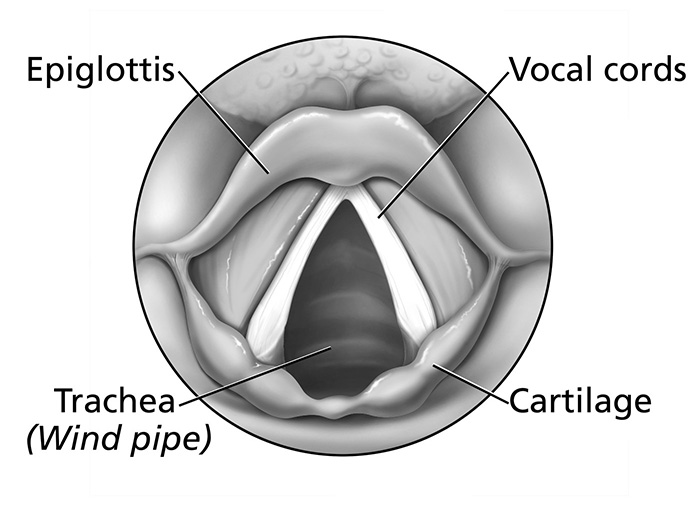
The epiglottis, vocal cords, and glottis are areas of the airway that can only be seen using specialized devices such as laryngoscopes or bronchoscopes. The epiglottis is a large, cartilaginous flap that closes over the glottic opening during times of food and liquid ingestion to preclude the aspiration of these substances into the trachea and lungs. The glottic opening contains the true and false vocal cords and opens a pathway from the upper airways to deeper airways leading into the lungs. Figure 4 shows a view of a normal human epiglottis, as well as the vocal cords (the small white structures) and the glottic opening. Figure 5 is an illustration of the glottic opening and related structures. The epiglottis may swell if repeatedly manipulated during a difficult intubation. Therefore, the first view during laryngoscopy is ordinarily the best view of the glottic opening.
Children may develop an infection of the epiglottis called epiglottitis that results in extreme swelling and partial occlusion of the airway. Children with this disorder typically have fever and lean forward to breathe while drooling heavily. A patient with these symptoms is experiencing a true airway emergency, and endotracheal intubation is ordinarily required. This should not be done except in the presence of an experienced laryngoscopist, usually an anesthetist, and preferably in the operating room with a surgeon present to gain a surgical airway if intubation fails.
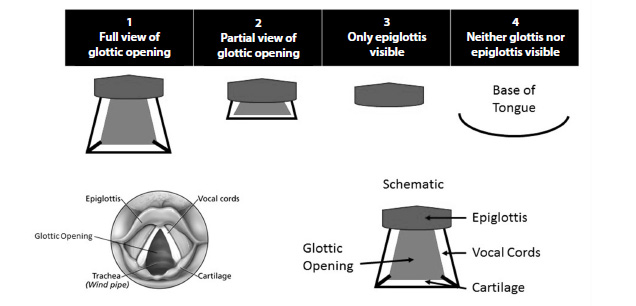
The epiglottis, vocal cords, and trachea are heavily innervated, as might be expected. They are the body's last line of defense to prevent the aspiration of potentially toxic substances into the lungs. Views of the glottic opening are categorized using the Cormack-Lehane system (Figure 6) [11]. Accurately documenting what is visualized when intubating via direct or video-assisted laryngoscopy is an important addition to the patient's medical record. It tells future providers how difficult it was to intubate this patient—the less visualization possible of the glottic opening, the more difficult the intubation. This knowledge may impact future airway management plans.
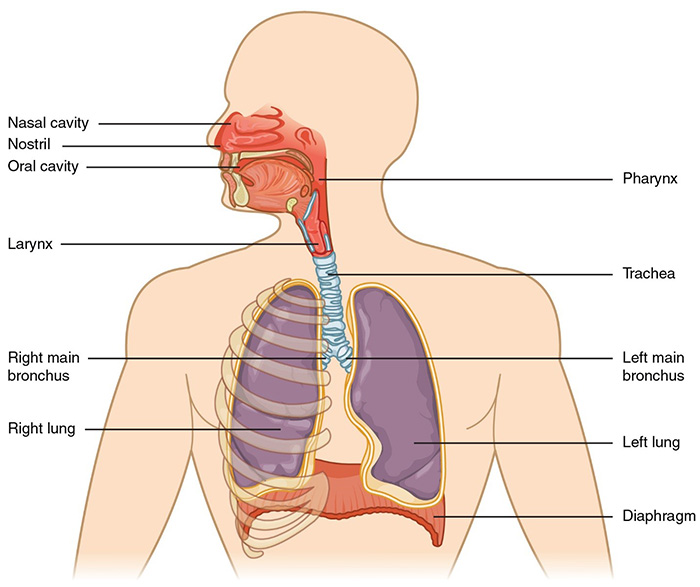
The conducting airways of the lung begin at the trachea, found beneath the glottic opening and midline in the neck. The trachea is a cartilaginous, horseshoe-shaped structure, with the curved part of the horseshoe closest to the skin in the neck. It is quite firm to palpitation. It is firm enough that when subjected to downward pressure (as may be applied during cricoid pressure), the entire laryngeal box will move downward in the intubator's field of vision, which usually simplifies exposure of the glottic opening. The trachea and two mainstem bronchi (Figure 7) are lined with cilia and do not possess gas exchange properties.
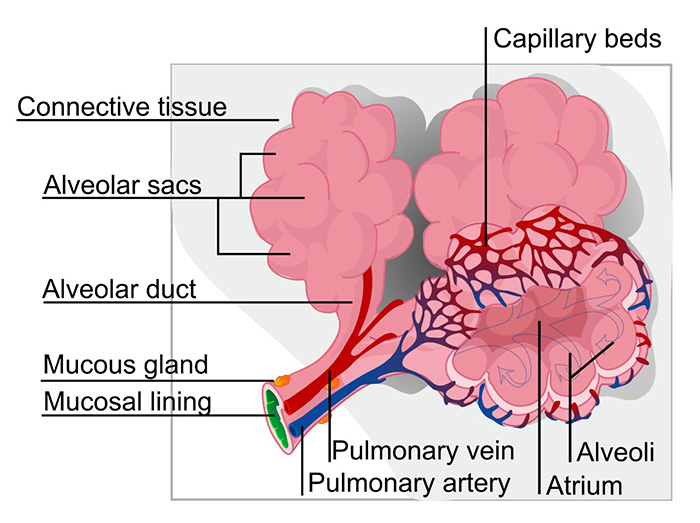
The conducting airways make up the anatomic dead space. While inhaled gases pass through these structures, no exchange of oxygen and carbon dioxide occurs within them. The conducting airways contain various amounts of smooth muscle. The upper airways have the largest amount of smooth muscle, with the amount diminishing as the airways become smaller, until it disappears upon reaching the alveoli. When exposed to a device or toxic substance, smooth muscle rapidly constricts, dramatically limiting the radius of the airway and thus exponentially limiting the flow of inspired gases to lower levels of the lungs. These changes in radius profoundly diminish flow through the airways. The conducting airways divide continuously through 16 generations, at which time the respiratory bronchioles begin to show the development of alveoli, where gas exchange can occur. From the respiratory bronchioles, inhaled gases move through the alveolar ducts and on to the alveoli (Figure 8) [12]. The blood comes from the heart and enters the capillaries surrounding these air sacs. This is the one place in the body where blood flowing from the heart (the right ventricle) and carried in an artery (the pulmonary artery) is deoxygenated and blood returning to the heart (the left atrium) through a vein (the pulmonary vein) is oxygenated [13]. The absorption of oxygen from and the excretion of carbon dioxide into these spaces form the basis of diffusion of gases into the blood, which are subsequently carried to tissue beds, where gas exchange and perfusion occur. The air/blood interface in these pulmonary capillaries is extremely thin, facilitating this gas exchange process in the lung.
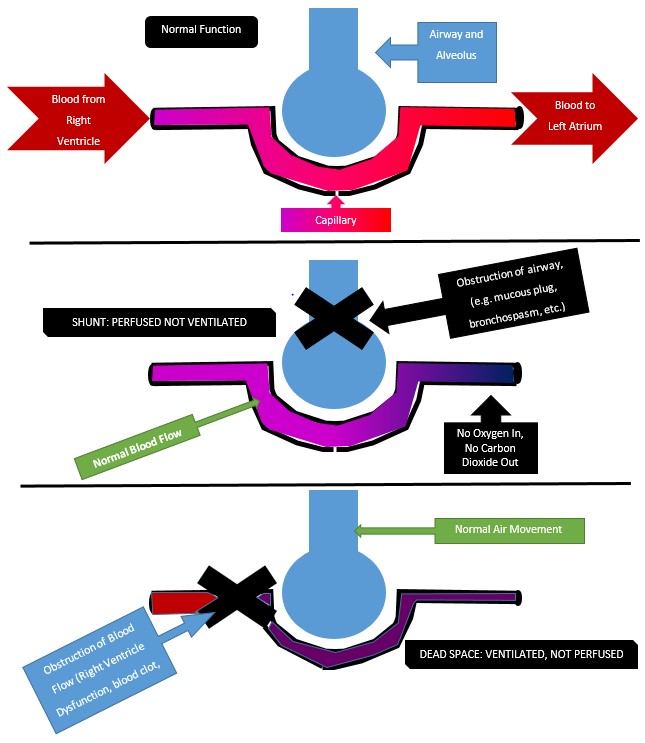
Though frequently confused by novice practitioners and students of health care, dead space and shunt are crucially important concepts when managing a patient's airway and ventilation. In areas of dead space, the tissue is ventilated, but not perfused. The inhaled gases flow over and around these anatomic structures, but due to a lack of specialized capillary bed and the absence of alveoli, no gas exchange occurs. This concept is important, as inadequate amounts of air provided to the patient during artificial or mechanical ventilation will only move air in these dead space areas. Air can rush into and out of the trachea, but if the volume is not sufficient to get to the capillary beds in the lungs, no exchange of gases will take place—the patient will become hypoxic and eventually expire. In areas of shunt, the tissue is perfused, but not ventilated. Once again, inadequate volumes of artificial ventilation or a blockage of an airway will result in ventilatory gases not reaching the capillary beds. This means no oxygen is able to get to the alveoli, so no oxygen will get into the bloodstream. Further, the blood entering these capillaries, filled with carbon dioxide, is not able to unload this gas into fresh alveolar ventilation, resulting in its build up systemically. Carbon dioxide is a volatile acid, and its retention results in respiratory acidosis (Figure 9).
Each patient has both anatomic and physiologic dead space, as well as anatomic and physiologic shunt. Anatomic dead space consists of all anatomic structures that cannot participate in gas exchange. From the mouth and nose to the terminal bronchioles, these structures only conduct gases, they do not directly participate in gas exchange. However, it is also possible to have physiologic dead space. In these instances, even though gases enter the alveolus and are ready for gas exchange, some problem with blood flow to the capillary results in decreased or absent perfusion. For example, patients who have extreme hypotension because of shock may not be able to adequately pump blood to the lungs. This lack of circulation results in alveoli that are ventilated (an adequate volume of air or gas is being placed in the lung) but not perfused (an inadequate amount of blood is present in the capillaries).
Each patient has approximately 8% physiologic shunt, as some of the blood that enters the lungs is not used for gas exchange but rather to oxygenate lung tissues themselves. This small volume of blood is perfused (comes in contact with the tissue to oxygenate the tissue and carry away waste and carbon dioxide) but not ventilated (does not enter the alveolar capillary membrane to load oxygen and unload carbon dioxide). Patients may have illnesses or pathologic conditions that lead to increased shunt levels. For example, a patient with an asthma or bronchitis may occlude an airway, which causes a section of the lung not to be ventilated, due to either severe airway narrowing (asthma) or the creation of a mucous plug (bronchitis). As a result, alveoli distal to the site of occlusion will be perfused but not ventilated. The heart will continue to pump blood to this region of the lung, but no exchange of gases can take place.
In all but the most benign cases, patients with a managed airway and/or ventilation will receive oxygen supplementation. To correctly administer oxygen, practitioners should be familiar with gas laws, particularly Dalton's Law of the Partial Pressure of Gases. This section will demonstrate how knowledge of this concept is important to healthcare providers.
Gases surround all people as they walk through the sea of air that blankets the earth. Air is composed of approximately 21% oxygen and 78% nitrogen, along with numerous trace gases. At sea level, the pressure of the air, measured in millimeters of mercury (sometimes referred to as torr), is the sum of the pressures of all of the gases surrounding us. For example, 21% oxygen times 760 mm Hg of pressure means that almost 160 mm Hg of the pressure is from oxygen. The remaining pressure comes from the nitrogen and other trace gases. When we breathe, oxygen enters conducting airways in the nose and mouth at this pressure of 160 mm Hg but is quickly reduced as the water vapor excreted from our tissues moistens these gases. This water pressure is about 47 mm Hg, so the partial pressure of oxygen is now reduced to 113 mm Hg [13]. Gases are carried in the bloodstream after passing through the alveolar membrane and associated structures into the blood in the capillary. When the 113 mm Hg of oxygen moves through the conducting airways, it is somewhat diluted by gases already present, until the oxygen entering the alveolus has a pressure of approximately 104 mm Hg. Normal arterial blood gas values for oxygen are 80–100 mm Hg, and one can quickly see that in times of normal health, the diffusion of oxygen into the bloodstream has little hindrance.
However, altitude can affect these values significantly. At 15,000 feet above sea level, the pressure is just 429 mm Hg; the composition of the air remains 21% oxygen, 78% nitrogen, and trace gases. Inhaled oxygen is now just 91 mm Hg. This level is saturated with 47 mm Hg of water, and now only 44 mm Hg of oxygen is left, far below the normal partial pressure of 80–100 mm Hg at sea level. The shortness of breath and feeling of exhaustion at even the slightest exertion at this altitude is easily understood, as individuals have less than half the oxygen in their blood as would be present at sea level.
Consider a patient in a high-altitude environment who is administered oxygen at 3 liters per minute from a simple nasal cannula. This would increase the percentage of inhaled oxygen from 21% to 32% [14]. With this intervention, 137 mm Hg of oxygen is delivered to the conducting airways. After mixing with water vapor, 90 mm Hg oxygen pressure remains, nearly the same value as at sea level and once again adequate oxygenation for tissues. Increasing oxygen concentrations, even slightly, results in large increases of oxygen delivery to the alveoli. This key concept will help guide subsequent efforts to manage airway and ventilation in patients.
When time permits, a thorough assessment of the mouth, oral airway, and dentition is important in airway management. If the situation is urgent but not yet an emergency, there are several minutes available to mentally create a plan to manage the patient's airway. This planning period is especially important if the patient is conscious but may become unconscious. One example of such a case is preparing a patient for deep sedation before a procedure or evaluating an ill patient with a worsening condition that indicates airway management may soon be needed. An easy mnemonic to remember is MOUTH [15]:
Mallampati classification
Obesity and opening (oral and nasal)
Upper lip bite test
Teeth
Head and neck movement
These observations will help to determine the difficulty that may be involved in manipulating the airway. To begin, ask conscious patients to look straight at you and open their mouth as widely as possible without sticking out their tongue. This will provide a Mallampati score (Figure 10), which indicates prospective difficulty in airway maintenance and intubation [16]. The ability to see tonsillar pillars, the soft palate, and the uvula indicate an airway that will be comparatively easily manipulated [16]. Conversely, the ability to see only teeth and tongue is prognostic for a difficult intubation, should one be required [16]. Next, patients should be asked to open their mouths. Does the patient have teeth? What is the general condition of the teeth? Missing and carious teeth are indicators of overall health, and poor dentition may be an indicator of poor health overall. How far can the patient open his or her mouth? Patients should be able to open their mouths to provide a space two to three fingerbreadths wide [17]. Is the patient obese? This does not require a body mass index (BMI) calculation, just a simple observation. Obesity correlates positively with airway obstruction and increased difficulty in airway management [18]. The upper lip bite test is a rapid and effective way to determine jaw movement and opening. Ask patients to place their bottom teeth on their upper lip. An inability to do so may portend problems with airway management, especially in mandibular manipulation. Absent teeth result in better intubating conditions, as the mouth opening tends to be wider, but the absence of structure provided by the teeth may result in more difficulty in obtaining a tight seal with a device. Head and neck movement provides the rescuer an idea of how flexible the patient's neck is and may demonstrate that a head-tilt initial technique will be useless and possibly dangerous if there is limited extension of the neck.
In emergent situations, such an advanced assessment will be impossible. However, most emergency medical manuals advise rescuers to at least scan the patient. A patient who is obese, thick-necked, with a full beard, or with a tiny or recessed mandible should signal that airway management may be difficult. In any case, if a patient requires outside assistance in maintaining a patent airway, there is a significant and often life-threatening reason for this problem. In any airway-based intervention, it is important to send for help quickly, as providers may find they need all their skills to maintain the airway in an open position or may be unfamiliar with more advanced techniques.
Even the simplest problem with an airway, if left untreated, can lead down a pathway of severe morbidity and even death. The best treatment is often the simplest, requires the fewest devices, and is most easily monitored.
In many cases, airway management is best accomplished by positioning oneself at the head of the patient. While it can be possible to assist patients by standing beside them, most airway maneuvers on patients who are unconscious and supine are best accomplished from this position.
The purpose of the head-tilt, chin-lift, and jaw-thrust maneuvers is the same: to displace the tongue from the posterior airway. Patients who have decreased levels of consciousness, either from some pathologic state (e.g., syncope) or after receiving sedative or narcotic medications, may relax their head and neck and allow their tongue to slip to the back of the airway. This is usually accompanied by loud, stertorous breathing sounds, such as snoring. A key point to remember is that noisy breathing is obstructed breathing until proven otherwise. The first step is to determine if the patient is truly unconscious or in need of airway manipulation. This can be accomplished by grasping the patient's shoulder firmly and gently agitating the patient, calling his or her name to see if there is any response to these stimuli. Avoid both shouting and whispering; use a conversational tone such as you might employ speaking to a friend in a crowded room—a voice just a bit louder than usual. If the patient fails to respond, the rescuer is free to proceed with noninvasive airway maneuvers.
The head-tilt method is generally preferred and considered the easiest. With this maneuver, the patient is placed supine, and the rescuer places one hand on the patient's forehead and another on the patient's chin. The rescuer then gently tilts the patient's head back until the chin points up. If the rescuer suspects the patient may have a cervical spine injury, this technique is not recommended. The chin-lift technique is also quite simple. The provider moves beside or to the head end of the patient and places her/his thumb beneath the patient's chin and lift upwards (Figure 11). With either technique, one of the following results will be evident:
The patient will awaken, indicating he/she was not as deeply unconscious as may have been thought.
The patient will take a deep breath and continue breathing spontaneously, and may or may not regain consciousness.
The patient will move some air but breathing remains noisy, indicating an inadequate control of the airway.
The patient will remain apneic, requiring further intervention.
Patients who easily awaken when the chin is lifted or head is tilted may require no further intervention. Despite this fact, rescuers are encouraged to err on the side of seeking further treatment; airway obstruction requiring intervention is not a normal event. If the patient does not immediately regain a robust state of consciousness, the provider should send for help, either by dialing 911 if intervening in a nonclinical area or by alerting the institution's rapid response team (e.g. "code blue," "HELP team," or other team designed for emergency intervention in the facility). Altered states of consciousness resulting in airway obstruction may signal more profound pathologic changes that should be evaluated and treated.
The jaw-thrust technique is designed to achieve the same result but requires two hands and is somewhat more demanding. This technique does not require movement of the patient's neck and is a better choice if the patient is unconscious secondary to trauma. Positioning oneself at the patient's head, grasp the patient's lower jaw with both hands, one on either side of the face (Figure 12). Place your fingers behind the angle of the patient's mandible, and lift the mandible straight up. The patient should begin to breath. If performed aggressively, this technique will be painful for the patient, resulting in sympathetic stimulation, which may also prompt resumption of breathing. If the patient is only mildly sedated or in a light state of unconsciousness, he or she may attempt to squirm out of your grasp or show other signs of a response to pain. If the patient has no reaction, it is possible other more advanced techniques may be required. It is difficult to hold the jaw thrust position for a long time without tiring, and if the patient's response is weak (insufficient or absent respiratory effort), it should be seen as a bridge to more definitive care. One advantage of this technique is that it can be used to hold the breathing mask of a bag valve mask (BVM) device in place (Figure 13) [19]. In all of these manipulative techniques, if the patient does not immediately awaken and resume adequate spontaneous respiration, supplemental oxygen should be administered as soon as possible using either a nasal cannula, a standard or non-rebreathing oxygen mask, or, in the case of apnea, a BVM device. Continuous monitoring of respirations should also be maintained until the patient's care can be transferred to another provider (e.g. from a bystander to emergency medical personnel, or from ward staff to a respiratory arrest team).
If head and jaw manipulation techniques are inadequate, the provider should move on to the insertion of pharyngeal devices. These devices are easy to insert when used properly and will greatly increase the ease with which the patient's airway may be maintained. The purpose of these devices is exactly the same as the head and jaw manipulation techniques: to move the tongue away from the posterior pharynx and open the airway. The two primary devices are the oropharyngeal and nasopharyngeal airways.
The oropharyngeal airway (Figure 14) is designed to be used for patients with both airway problems and diminished consciousness. This latter condition is extraordinarily important, as oropharyngeal airways should not be used for patients who have a gag reflex. Their insertion may result in causing the patient to vomit, placing her or him at risk for pulmonary aspiration.
After determining the patient's level of consciousness and after attempting the simpler head and jaw manipulation maneuvers, the rescuer may prepare to insert the oropharyngeal airway. The first step is to determine the correct size of the airway. This is done by placing one end of the oropharyngeal airway on the face, with one end at the corner of the mouth. The other end is placed at the patient's ear; the correct sized airway should end at the opening of the ear. Insertion of the airway has been described in many ways. One technique involves rotating the airway 180 degrees, so the curve (concave surface) is facing away from the tongue and toward the roof of the mouth. The airway is then inserted into the mouth, rotated 180 degrees so the curvature is toward the tongue, and then pushed inward until the flange of the device reaches the teeth or gums. The goal of this technique is to avoid pushing the tongue further into the posterior airway. The rescuer visually observes the airway as it enters the mouth to ensure damage is not created by its insertion; the distal end of the airway can irritate or lacerate the palate prior to its rotation. In the worst case, this can cause bleeding from a very vascular area. The second technique is to rotate the airway 90 degrees, with the curve of the airway facing the lateral teeth (the molars), then rotating it 90 degrees after passing the tongue, once again ensuring the tongue is not pushed distally into the airway. The same advice is proffered for this insertion technique—use care to avoid damaging tissues in the mouth. The final technique may be the easiest and involves using a tongue depressor to gently hold down the tongue. The airway is then inserted following its curvature, so the concave surface faces the tongue. In the absence of a tongue depressor, the rescuer can take a small gauze pad and grasp the tongue and hold it in place while inserting the airway with the other hand. Patients who fight the insertion of the airway are insufficiently obtunded for its use. After the airway is in place, it may be released while continuing to grasp the jaw using the jaw-thrust technique. Ordinarily, the force required to maintain a patent airway decreases dramatically, and a BVM device may be used by a single rescuer using one hand to hold the breathing mask against the face and the other to squeeze the bag reservoir (Figure 13). If the patient is breathing spontaneously, the BVM device with a supplemental oxygen attachment may still be used by simply holding the mask over the patient's face and not squeezing the bag.
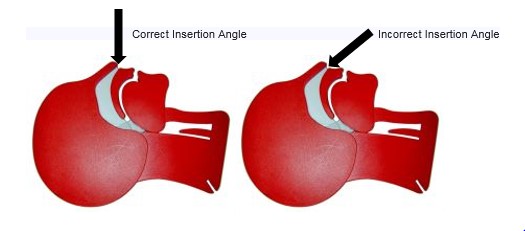
Some patients may be disoriented or have a partial loss of consciousness but are insufficiently obtunded to tolerate the oral airway. If this is the case, a nasopharyngeal airway may be used (Figure 15), as it triggers the patient's gag reflex less than the oral airway. Insertion of the nasopharyngeal airway looks simple, but it is often inserted incorrectly. The angle of entrance into the nose is the key. In the supine patient, the airway should be perpendicular to the floor. The angle of airway entry should be as close as possible to 90 degrees from the plane of the face (Figure 16). If placed at a 45-degree angle, with the tip directed toward the top of the head, the airway will be pushed through the highly vascular turbinates of the nasal cavity, resulting in severe bleeding.
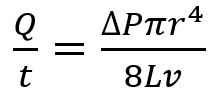
The first step is to measure the diameter of the nasal airway. Note that these airways are designed to be inserted in the right nare, whenever possible. This can be verified by the angular tip of the airway, which should face midline. To determine the correct length, measure from the tip of the nose to the opening of the ear, in the same manner as measuring the oropharyngeal airway. Next, visually inspect the nare and compare the tip of the airway to the diameter of the nare; the airway should be slightly smaller. Apply a water-soluble lubricant to the airway. This use of lubricant is quite important, as even the most flexible nasopharyngeal airways can traumatize the highly vascular area in the nose. If the facility or organization permits its use, local anesthetic ointment application to the airway may be helpful in having the patient tolerate its presence. The administration of a nasal spray vasoconstrictor, such as over-the-counter oxymetazoline (Afrin), can help decrease the chance of bleeding after airway insertion, though some organizations do not permit its use. In some cases, a small, well-lubricated airway is initially inserted, with the smaller airway replaced with airways of increasing size in a sequential fashion to the maximum allowable diameter. As each tube is replaced, the airway is dilated a bit more, easing air flow through the nose and nasopharynx. Using the maximum safe diameter with the nasopharyngeal or any other tube-like airway is extremely important. Flow through the tube increases exponentially as the diameter increases, as demonstrated by the Poiseuille equation [13]:
In this equation, Q/t is air flow, ∆P is the pressure difference, r is the radius of the airway, L is the length of tube, and v is the viscosity of the fluid or gas. The key concept here is that flow is exponentially proportional to the radius of the airway. As such, one can see that small changes in radius equal large changes in flow. For example, doubling the diameter of the airway increases flow 16 times. When the nasopharyngeal airway is inserted all the way into the nose, it passes the nasopharynx and lifts the tongue away from the posterior airway. This airway can be used with patients who are awake but struggling to maintain an open airway. Once inserted, supplemental oxygen should be initiated as quickly as possible via either a nasal cannula or simple mask.
Patients with severe head injury should be carefully evaluated prior to the insertion of a nasopharyngeal airway, and the benefits of its insertion should outweigh the risks. If the nose shows signs of blood or clear fluid (suggesting skull fracture with release of cerebrospinal fluid), these airways should be avoided or used with extreme caution. In these cases, the airway may puncture the cribriform plate on insertion and enter the brain.
Laryngeal devices are somewhat more advanced than pharyngeal airway devices, but they are still characterized by an increased depth of insertion and blind insertion (i.e., no extraneous devices, such as laryngoscopes, are needed for their placement). The two more common devices are the King airway and the laryngeal mask airway, more commonly referred to as an LMA. These are similar to the oropharyngeal airway in that they are indicated for use only when the patient has a significantly decreased level of consciousness that precludes activation of a gag reflex.
The King airway has been described as being both easy to insert (with an 86% first-time success rate) and effective (Figure 17) [20]. The device is inserted in the mouth and passed midline. The device may be slightly rotated before insertion if the tip is getting caught on the tongue. It is important that the tube is first lubricated with the packet of water-soluble lubricant (packaged with the device) and that both the balloons are fully deflated. The use of a tongue depressor or the thumb of the non-insertion hand to hold the tongue away from the back of the airway will facilitate the insertion of this device. The device will pass down the oropharynx into the larynx. Once seated, the balloons are inflated using a provided 30-mL syringe. There is only one port for the syringe, and both balloons will inflate from this single port. If properly inserted, the lower balloon enters the esophagus, partially to fully occluding it and decreasing the likelihood of aspiration of vomitus into the airway. The upper balloon inflates above the glottic opening. The time required for the correct insertion of the airway is quite short, an average of 26 seconds in one study [21]. Using a BVM device, the pressure created by squeezing the bag causes air to exit the openings distal to the bag and enter the respiratory tract. The King airway comes in various sizes, and care should be taken to match the correct size airway for the patient according to manufacturer guidelines (provided with the device).
The forerunner of the King device was the Combitube, which functioned in an analogous fashion but placed the a longer esophageal blocker somewhat further down the esophagus and required two balloons for inflation, as well as a determination by the provider that the esophageal tube had not inadvertently entered the trachea. Its description here is included for the sake of completeness, but its use is diminishing and the device will most likely not be encountered by clinicians.
The LMA was developed in 1981 and is now widely used as to maintain airway patency during anesthesia [22]. The LMA comes in numerous sizes and permutations, but essentially, it is designed to maintain the airway by placing an inflatable cuff around the glottic opening. It differs from the King airway in that no part of the device enters the esophagus. When it first appeared on the market, the LMA was hailed as a breakthrough rescue device when endotracheal intubation failed. Now, these devices are routinely inserted for all types of surgeries. The ability to place the device without visualizing the airway, as with the King, is one of the keys to its popularity. The practitioner first selects the correct size for the patient and then uses the water-soluble lubricant (included with the device) to thoroughly lubricate the cuff. Some practitioners advocate the complete deflation of the LMA cuff for insertion, while others find insertion easier if the cuff is partially inflated. In either event, the device is somewhat wide, and it may easily become caught on the tongue (especially if inadequately lubricated) or on the posterior wall of the oropharynx. Therefore, when inserting the LMA, the patient should be obtunded, as this large airway device will provoke gagging, with his/her head tilted slightly back. The LMA should slide smoothly over the tongue and seat securely in the larynx. At this point, the practitioner can finish inflating the balloon, thus securing the airway. In one study, insertion of this device was successful 98% of the time [23].
Local policies and procedures should be consulted before using this device. In some areas, use of the LMA is restricted to the hospital and surgical suite, while in other places, the LMA is gaining popularity as a prehospital tool and replacement for endotracheal intubation [21]. While the device may stimulate gagging as the patient recovers the use of the airway, the LMA is far less stimulating than an endotracheal tube and, once inserted, is well-tolerated by sedated patients. It is also useful for patients with obtunded central nervous systems but who are still able to breathe spontaneously if their airway is open.
Some LMAs allow the subsequent placement of an orogastric tube through a designated port in the device, permitting the practitioner to decompress the stomach. It is also possible to place an endotracheal tube through the glottic opening by passing a specialized tube through the device and inflating its cuff below the glottic opening. This is a more advanced technique typically attempted by more advanced or experienced practitioners.
Most healthcare professionals think of airway management in terms of endotracheal intubation, for good reason. Endotracheal intubation is the criterion standard for airway management. It is the surest way to secure a patient's airway and provides an avenue for mechanical ventilation. The largest drawbacks are:
It is a psychomotor skill that requires significant training and continued practice.
It frequently requires the administration of potent (and potentially lethal) doses of drugs to adequately sedate the patient or, in the absence of consciousness, temporarily paralyze the patient prior to performing.
It is accompanied by significant potential adverse effects, including aspiration of gastric contents; trauma to the teeth, mouth, and/or airway; and significant damage to the upper airway precluding access.
Whenever possible, if endotracheal intubation is required, it is important to have sufficient manpower, devices, and a backup plan in the event of failure. Endotracheal intubation is a difficult skill to acquire, requiring good instruction and significant practice time with both simulated and actual patients. In one study, an average of 57 attempts at intubation was required to develop a 90% success rate among anesthesia residents [24]. The same study noted that 18% of learners continued to require assistance after 80 attempts [24]. This study was limited to a strictly controlled environment in the operating room.
There are two main methods for endotracheal intubation: direct laryngoscopy with either a straight (Miller) or curved (Macintosh) blade, and video-directed laryngoscopy that uses a fiber-optic image displayed on a screen to visualize the airway prior to tube placement.
Direct laryngoscopy is indicated to obtain airway access and maintenance in patients with severe medical pathology or traumatic injury. It is also performed for routine, urgent, and emergent surgical procedures. Before performing endotracheal intubation, the provider should ensure the following steps have been accomplished:
Send for help. Even the routinely performed endotracheal intubation is more facile with an extra set of hands—or more.
Assemble and assess the necessary equipment. This will include:
Laryngoscope handle and appropriate blade
Bright light for visualization (When the blade is connected to the handle, shining the light in your eyes should cause you to squint.)
Endotracheal tube of the correct size (and at least one size larger and one size smaller than expected)
A stylet to facilitate insertion of the tube
Suction device
Intravenous access if medications are thought to be needed
Medications for intravenous administration (e.g., anesthetic induction and paralytic agents, at a minimum)
Monitoring devices to measure oxygen saturation levels, heart rate, blood pressure, electrocardiogram, and end-tidal carbon dioxide levels
Stethoscope to listen for breath sounds
A functioning BVM device, connected to supplemental oxygen if possible
Have a backup plan if intubation fails. Even masking the patient with an oropharyngeal airway and supplemental oxygen while waiting for help prolongs the duration of time before organ damage secondary to hypoxia begins.
During the preparation phase, patients should be receiving supplemental oxygen in some fashion whenever possible. This is important even if the patient has diminished breathing or appears apneic. In a seminal study, Weingart and Levitan found that with sufficient administration of high-flow oxygen (90% from a well-fitted, non-rebreather mask), patients can absorb as much as 250 mL/minute of oxygen into the bloodstream, thus significantly prolonging the time a compromised patient has until hypoxia occurs [25]. Another substitute is high-flow oxygen via a nasal cannula. In two studies, hypoxia before intubation was alleviated more efficiently by a properly placed nasal cannula than by breathing through the mask portion of the BVM device [26,27]. In the absence of a rebreather mask or nasal cannula, simply holding the mask attached to the BVM device tightly to the patients face while attached to a 10- to 15-liter per minute oxygen flow will improve oxygenation, albeit somewhat less efficiently.
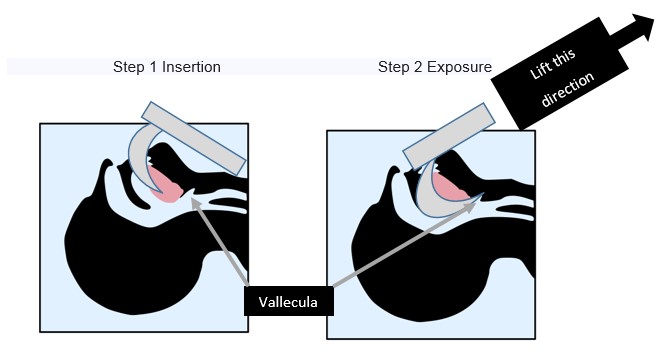
After the preparatory work is complete, it is time to begin the intubation process. Laryngoscopes are comprised of a handle that usually contains a power source (ordinarily batteries of some kind) and a blade that is inserted into the patient's mouth and passed to the larynx, enabling the operator to physically see the glottic opening and watch the tube enter through the vocal cords and into the trachea. The curved or Macintosh (or Mac) blade (Figure 18) comes in many sizes, though the average adult is easily intubated with a Mac 3 blade. A size 4 is useful in large patients, especially those who are obese, provided the patient's mouth opening is sufficient to insert the rather wide flange on the blade. The tip of the blade is designed to be inserted into the vallecula, the small area between the base of the tongue and epiglottis. Raising this area indirectly raises the epiglottis, exposing the vocal cords and glottic opening.
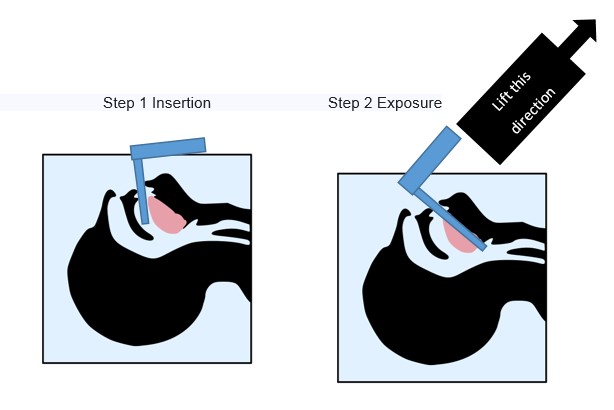
The straight or Miller blade (Figure 19) also comes in various sizes, but a 2 or 3 blade is ordinarily used in the average adult patient. The Miller blade is used to physically raise the epiglottis away from the glottic opening by lifting the epiglottis with the tip of the blade.
The degree to which the patient is conscious will guide the degree of sedation and paralysis needed for intubation. Though intubation can be performed in the absence of induced sedation, only the most obtunded patient will not struggle and attempt to resist during intubation. Discussion of pharmacotherapy to sedate a patient for intubation is outside of the scope of this course; the following discussion assumes adequate sedation to allow safe intubating practice.
The patient should be positioned supine, with the head on a small cushion or flat on the bed, with the practitioner positioned at the head of the bed. For patients with normal body habitus, the bed should be raised or lowered until the level of the patient's head is roughly at the level of the provider's waist. Any large pillows should be removed, though a small, folded towel or "doughnut-type" pillow may be helpful in supporting the patient's extended head. Then, gently tilt the patient's head back so the chin points toward the ceiling. If a curved or Macintosh blade is being used, open the patient's mouth with your right hand, using the scissors technique. Laryngoscopes are designed to be used with the left hand only. The laryngoscope blade should be placed on the center of the tongue. Opening the mouth as wide as possible, begin to insert the blade along the tongue and deep into the oropharynx. This requires a rotating-type movement, tracing the angle of the blade along the tongue, similar to rolling it along a ball (Figure 20). Continue to advance the blade until it enters the vallecula, the small anatomic structure that is the connection point for the base of the epiglottis and the tongue. The tip of the blade is now in the correct position. Be aware of the wide flange of the blade where it is now in the mouth. Pulling back on the handle of the laryngoscope will cause the blade to contact the teeth, which may result in unintentionally chipping or breaking the teeth.
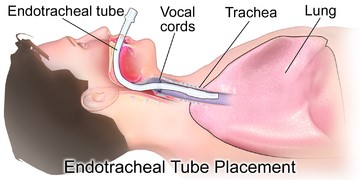
Imagine the patient's toes are pointing toward the ceiling, and imagine a point at which a line drawn straight up from the toes would intersect the plane of the ceiling. Using the left arm, push the handle toward this imaginary point. The arytenoid cartilages and the glottic opening should now be visible. While maintaining visualization, signal for an assistant to place the endotracheal tube (Figure 21) in your right hand. Hold the tube midway down its length as you would hold a pencil, and gently insert the tube into the mouth, guiding it down the oropharynx, into the larynx, and through the glottic opening. When the cuff of the tube passes the glottic opening, while continuing to anchor the endotracheal tube, gently remove the laryngoscope and place it in a "dirty" area of the workspace. The stylet should also be removed from the endotracheal tube. The cuff is then inflated with 3–7 mL of air in a 10-mL syringe. Next, connect the BVM device and ventilate the patient while auscultating over the lung fields to confirm the presence of breath sounds, which should be equal bilaterally. A carbon dioxide monitor or detection device should be connected to confirm the presence of carbon dioxide in exhaled vapors. Finally, secure the tube with tape or a tube-holding device, based on the requirements of the specific intubation. It is best to always recheck breath sounds after securing the tube, as it can move during the process of securing. At this point, one must decide either to continue using the BVM device or to switch the patient to a mechanical ventilator.
The straight or Miller blade is used somewhat differently (Figure 22). After the patient is correctly placed and prepared, inspect the tongue to identify a faint midline. Align the straight blade marginally to the right of this line, so 40% of the blade is on the left side of the line and 60% is on the right side. Advance the blade to the back of the tongue, watching the tip of the blade at all times. When the epiglottis is in view, gently place the tip of the straight blade on the epiglottis itself and, just as with the curved blade, push the handle straight toward the imaginary point on the ceiling, as described in the section on the MacIntosh blade. The patient's glottic opening should be clearly visible. There is a groove in the straight blade that allows the operator to view the glottic opening, not to guide the endotracheal tube. The endotracheal tube should be placed into the oropharynx to the right of the straight blade, while continuing to visualize its entry through the glottic opening and disappearance below the vocal cords. The laryngoscope blade is then gently removed from the patient's mouth, while maintaining a firm grip on the endotracheal tube to ensure it is not inadvertently removed from the trachea. The cuff of the endotracheal tube is inflated with the insertion of 5–7 mL of air; the amount of air placed in the cuff should be just enough to prevent back flow of air into the laryngopharynx. Backflow can be heard by placing a stethoscope over the neck and listening for a leak (air "whooshing" or rustling). When the noise stops, there is sufficient air in the cuff. A BVM device is then attached, with continued monitoring of breath sounds and end-tidal carbon dioxide. The end-tidal carbon dioxide monitor is the criterion standard for monitoring and confirming correct tube placement and will work in all situations unless cardiac output is either absent or so low that the lungs are not being perfused. The final step is securing the endotracheal tube. In a non-operating-room environment (e.g., the emergency department or intensive care unit), it is prudent to obtain a portable chest x-ray as soon as possible after tube insertion to confirm its correct position.
The endotracheal tube has markings indicating the depth of the tube opening. For the average adult patient, the tube is correctly placed at a distance three times the tube diameter. For example, a 7.5-mm tube can be secured in such a fashion that the tube line indicating 22 or 23 centimeters is shown at the level of the patient's teeth. Most modern tubes have markings indicating correct oral and nasal depth.
Video laryngoscopy systems are a modification of the direct laryngoscopy systems discussed. The primary advantage of these systems is that the fiber-optic camera is located near the end of the blade, thus decreasing the force required to bring the glottic opening into view. These systems all use curved blades, which are inserted in a manner similar to the Macintosh blade. The main difference is that this blade need not be maneuvered into the vallecula; indeed, doing so would occlude the user's visual field. The video laryngoscope either has a small video screen mounted on a rolling platform, or a smaller screen connected directly to the handle of the laryngoscope. In the case of the former, the screen should be placed in such a position that the practitioner can see both the screen and the patient, usually somewhere near the patient's left shoulder. In either case, immediately after the insertion of the blade into the patient's mouth, the practitioner should watch the screen and identify the anatomic landmarks of the upper airway. It is not necessary to employ the degree of force needed to expose the glottic opening with direct laryngoscope; merely instead, the practitioner can gently lift the laryngoscope, while being careful not to damage the patient's teeth, until the glottic opening is in view [28]. These devices come with endotracheal tubes with specially designed stylets. The tubes are inserted into the mouth to the right of the device and carefully passed toward the oropharynx until the tip of the tube is also seen on the video screen. The tube can then be advanced through the glottic opening under video observation, confirming its placement. It is likely that these devices will soon replace direct laryngoscopy almost entirely. The technique is easier and associated with greater first-time success rates, particularly in patients with difficult airways [28,29]. Video laryngoscopy has also been suggested as a rescue technique to be used in the case of failed direct laryngoscopy [18]. Other uses include difficult airways in patients with obesity, cervical spine disorders (e.g., arthritis, osteoporosis), or traumatic cervical spine injuries. Perhaps the best reason to use video laryngoscopy is its increased success rate when used by novice practitioners when compared with direct laryngoscopy [30].
Short of being able to provide high-fidelity simulation or actual clinical experiences, this final section will examine postulated examples of times when healthcare providers may be called upon to assist or personally perform airway management. These examples are designed to help further understanding of the airway techniques discussed. In each example, the same precepts apply: approach the patient in a manner that indicates a willingness to act, and be confident in one's abilities and knowledgeable about the resources available. This latter concept requires professionals to have knowledge of the equipment available (and its location) and the policies delineating its use before the airway emergency arises. Such training should be frequent and goal-directed.
In all cases, but especially in staffed medical facilities, the first step is to send for help as you begin to intervene. Outside of medical facilities, this may include calling emergency medical services.
Nurse A is a staff nurse on a general medical-surgical ward in a small hospital answering a call light. On arrival, her patient, an elderly woman who has had a minor surgical procedure, is coughing and snoring loudly and her daughter is concerned about her condition.
Using the bedside call light, Nurse A sends for help. This is an uncommon occurrence in the otherwise stable patient recovering from surgery and may be a precursor of more serious problems.
Nurse A then speaks to her patient and determines her level of consciousness. Some patients may respond appropriately and immediately clear their own airway. However, in this case, the patient does not respond to verbal stimuli.
Next, Nurse A places the head of the bed flat and removes the headboard. She gently places her thumb under the center of the patient's chin and displaces her chin upward, toward the ceiling. The tongue is the most likely anatomic structure to occlude the airway, and displacing it from the oropharynx may result in the return of spontaneous respirations. Nurse A's patient begins to breathe, though her respiratory rate is still somewhat low at 8 to 10 breaths per minute.
By now, the help team has begun to arrive, and they bring the emergency cart containing medications and monitoring devices. In the event further equipment is needed, it is now instantly available. Oxygen is administered via a simple mask, and a pulse oximeter is placed on the patient's finger, revealing a blood oxygen level of 90%, which increases over five minutes to 95%.
A review of the record by one of the assisting staff members reveals the patient received an intramuscular dose of an opioid 15 minutes before the call light was pressed. In order to determine if this is the underlying etiology for the problem, a small dose of naloxone is administered. Almost immediately, the patient begins to respond to verbal stimuli. In this case, the patient had an idiosyncratic response to opioid administration.
The only action necessary to re-establish the patient's airway and ventilation was to displace the patient's tongue from her oropharynx. After help arrived, a more in-depth investigation into the cause of the airway problem could be completed, and definitive therapy (narcotic reversal) applied.
Dr. T is the staff psychologist in a multidisciplinary mental health clinic. His next patient has a 50-minute counseling session scheduled. As she is sitting and discussing her concerns, she becomes increasingly restless, squirming in her chair and unable to become comfortable. Dr. T notices her breathing is becoming labored and invites her to lie down. As the patient stands to move to the recliner, she loses consciousness, falling to the floor.
This is a very unusual emergency for the facility's multidisciplinary team, and the patient's condition appears to be rapidly degrading. Dr. T calls out, and when the door opens, he instructs the receptionist to call 911.
Dr. T rolls the patient over and attempts to awaken her, with no response. Her breathing is noisy and labored, so he places her supine and performs a chin-lift technique. Help is on the way, and Dr. T has few tools available, so opening the airway is the easiest and quickest way to possibly improve the situation.
As Dr. T tilts the patient's head back, he notices a rash around her nose and mouth and on her upper chest, which is exposed by a V-neck shirt. She has a bracelet on her right arm that says "PEANUTS" and has a medical symbol beside it. At the same time, the receptionist brings in a large first-aid kit that includes a BVM device. The patient's breathing is now very noisy, and her chest is barely moving. Dr. T begins to ventilate the patient, holding the mask with two hands while an assistant squeezes the bag. Despite opening the airway, the patient is still breathing inadequately and help has not yet arrived. So, the ventilation Dr. T provides is a bridge to the arrival of paramedics.
Paramedics arrive on the scene with oxygen and advanced drugs and equipment. Dr. T relates his findings while they apply oxygen to the BVM device and insert an intravenous line. This patient may need more advanced interventions, and the drugs are best given intravenously. The paramedics note the patient is wheezing and decide to administer epinephrine for a suspected anaphylactic response. Within minutes, the patient's wheezing stops, and she begins to breathe and responds to verbal stimuli.
Paramedics have relieved Dr. T of the care of this patient and provide supplemental oxygen to prepare for transport. Dr. T's prompt interventions provided the necessary bridge to definitive care.
Mr. N is a staff nurse on the night shift in the emergency department. A woman, 70 years of age, with acute shortness of breath and palpitations stumbles toward the triage desk, collapsing into the chair at the vital signs station and gasping for breath. Her blood pressure is low, and her respiratory rate is 35 breaths per minute. She is unable to complete sentences due to her labored ventilations.
Clearly, this patient is in extremis, and Mr. N requires help simply to move her to an emergency treatment room. It seems clear that this patient will need advanced interventions, so additional help is called for.
Airway and ventilation are the first priorities, and Mr. N applies oxygen in a rebreather mask. This patient is significantly short of breath, and oxygen will immediately begin to alleviate this condition in nearly every circumstance.
Mr. N remains at the head of the bed and continues to monitor the patient's ventilatory status, while ensuring the presence of a BVM device and that suction is readily available. The emergency team is present and working to apply monitors and obtain intravenous access; this allows Mr. N to focus all his attention on the patient's ventilatory status and to ascertain the patient's level of consciousness.
The team continues to work and determines the patient is going into respiratory failure. As such, Mr. N begins to prepare for endotracheal intubation. This patient will require mechanical ventilation to allow time for more definitive care. Anesthesia has been summoned to provide advanced airway management. Mr. N begins to review available tools; monitors are already applied, suction is present, and a BVM device (machine) is ready. Mr. N assembles the necessary laryngoscope with straight and curved blades as well as endotracheal tubes with the preferred size (and one size larger and smaller). Finally, Mr. N assembles the drugs and syringes on top of the cart to complete the necessary preparations. The anesthesia care provider arrives, assesses the patient's airway and condition, and is immediately ready to perform endotracheal intubation. Mr. N's preparations have decreased the time between the decision to intubate and the actual performance of the intubation.
The most important intervention in any urgent or emergent situation is securing the airway and ensuring adequate ventilation. The key points are to call for help as soon as possible and to always use the simplest possible intervention. By following these guidelines, the average healthcare provider has the potential to make a tremendous impact on the patient's disease or injury and ensure that the patient survives long enough to receive definitive care. The information presented in this course will help anyone address patients' airway problems in an efficient and effective fashion.
1. Szmuk P, Ezri T, Evron S, Roth Y, Katz J. A brief history of tracheostomy and tracheal intubation, from the Bronze Age to the Space Age. Intensive Care Med. 2008;34(2):222-228.
2. Priest RE. History of tracheotomy. Annals of Otology, Rhinology & Laryngology. 1952;61(4):1039-1045.
3. Vallejo-Manzur F, Perkins Y, Varon J, Baskett P. The resuscitation greats: Andreas Vesalius, the concept of an artificial airway. Resuscitation. 2003;56(1):3-7.
4. Metcalfe NH. The effect of the First World War (1914–1918) on the development of British anaesthesia. Eur J Anaesthesiol. 2007;24(8):649-657.
5. Waisel DB. The role of World War II and the European Theater of Operations in the development of anesthesiology as a physician specialty in the USA. Anesthesiology. 2001;94:907-914.
8. Bergman P. EMERGENCY! Send a TV show to rescue paramedic services! U Balt L Rev. 2007;36(3):347-369.
9. Dadure C, Sola C, Dalens B, Capdevila X. Regional anesthesia in children. In: Miller RA (ed). Miller's Anesthesia. 8th ed. Vol 2. Philadelphia, PA: Saunders; 2015: 2706-2756.
10. Stackhouse RA, Infosino A. Airway management. In: Miller RD, Pardo M (eds). Basics of Anesthesia. 6th ed. Philadelphia, PA: Saunders; 2015: 219-251.
11. Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia. 1984;39(11):1105-1111.
12. Patwa A, Shah A. Anatomy and physiology of respiratory system relevant to anaesthesia. Indian J Anaesth. 2015;59(9):533-541.
13. Hall JE (ed). Guyton and Hall Textbook of Medical Physiology. 13th ed. Philadelphia, PA: Elsevier; 2016.
14. Tokarcyzk A, Greenberg S, Vender J. Oxygen delivery systems, inhalation therapy, and respiratory therapy. In: Hagburg CA (ed). Benumof and Hagberg's Airway Management. 4th ed. Philadelphia, PA: Elsevier; 2017.
15. Parthasarathy S, Bag SK, Krishnaveni N. Assessment of airway: the MOUTH concept (letter to the editor). J Anaesthesiol Clin Pharmacol. 2012;28(4):539.
16. Mallampati SR, Gatt SP, Gugino LD, et al. A clinical sign to predict difficult tracheal intubation: a prospective study. Can Anaesth Soc J. 1985;32(4):429-434.
17. Gupta S, Sharma R, Jain D. Airway assessment: predictors of difficult airway. Indian J Anaesth. 2005;49(4):257-262.
18. Law JA, Broemling N, Cooper RM, et al. The difficult airway with recommendations for management. Part 2: the anticipated difficult airway. Can J Anaesth. 2013;60(11):1119-1138.
19. Fei M, Blair JL, Rice MJ, et al. Comparison of effectiveness of two commonly used two-handed mask ventilation techniques on unconscious apneic obese patients. Br J Anaesth. 2017;118(4):618-624.
20. Hagberg CA, Bogomolny Y, Gilmore C, Gibson V, Kaitner M, Khurana S. An evaluation of the insertion and function of a new supraglottic airway device, the King LT, during spontaneous ventilation. Anesth Analg. 2006;102(2):621-625.
21. Frascone RJ, Wewerka SS, Burnett AM, Griffith KR, Salzman JG. Supraglottic airway device use as a primary airway during rapid sequence intubation. Air Med J. 2013;32(2):93-97.
22. van Zundert TC, Brimacombe JR, Ferson DZ, Bacon DR, Wilkinson DJ. Archie Brain: celebrating 30 years of development in laryngeal mask airways. Anaesthesia. 2012;67(12):1375-1385.
23. Evans NR, Gardner SV, James MF, et al. The ProSeal laryngeal mask: results of a descriptive trial with experience of 300 cases.Br J Anaesth. 2002;88(4):534-539.
24. Konrad C, Schüpfer G, Wietlisbach M, Gerber H. Learning manual skills in anesthesiology: is there a recommended number of cases for anesthetic procedures? Anesth Analg. 1998;86(3):635-639.
25. Weingart SD, Levitan RM. Preoxygenation and prevention of desaturation during emergency airway management. Ann Emerg Med. 2012;59(3):165-175.
26. Miguel-Montanes R, Hajage D, Messika J, et al. Use of high-flow nasal cannula oxygen therapy to prevent desaturation during tracheal intubation of intensive care patients with mild-to-moderate hypoxemia. Crit Care Med. 2015;43(3):574-583.
27. Simon M, Wachs C, Braune S, de Heer G, Frings D, Kluge S. High-flow nasal cannula versus bag-valve-mask for preoxygenation before intubation in subjects with hypoxemic respiratory failure. Respir Care. 2016;61(9):1160-1167.
28. Zaouter C, Calderon J, Hemmerling TM. Videolaryngoscopy as a new standard of care. Br J Anaesth. 2015;114(2):181-183.
1. Apfelbaum JL, Hagberg CA, Connis RT, et al. 2022 American Society of Anesthesiologists practice guidelines for management of the difficult airway. Anesthesiology. 2021; [Epub ahead of print]. Available at https://pubs.asahq.org/anesthesiology/article/doi/10.1097/ALN.0000000000004002/117915/2022-American-Society-of-Anesthesiologists. Last accessed December 9, 2021.
2. Higgs A, McGrath BA, Goddard C, et al. Guidelines for the management of tracheal intubation in critically ill adults. Br J Anaesth. 2018;120(2):323-352. Available at https://www.bjanaesthesia.org/article/S0007-0912(17)54060-X/fulltext. Last accessed December 9, 2021.
Mention of commercial products does not indicate endorsement.