This course provides an overview of burnout, including the evolution of its definition, its causes, related symptoms, identification, and measurement. The effects of burnout are broad, with consequences not only for the individual personally and professionally but also for patient care and healthcare systems; these implications will be explored. Among the most significant implications is the nursing shortage and a subsequent decrease in the quality of patient care. A review of the literature provides insights into the primary sources of job dissatisfaction, stress, and burnout among healthcare professionals and nurses in particular. Knowledge of the most common risk factors for burnout can help individuals modify their personal and professional lifestyles more effectively. Suggestions are given for ways organizations and nursing leadership can create a healthy work environment in which priority is given to nurses' psychosocial well-being and to fostering supportive relationships. While these strategies are aimed at creating a better work environment for nurses, they also ultimately promote better care and safety of patients.
This course is designed for nurses and nurse practitioners at all levels and in all settings, especially oncology, palliative care, mental health, and critical care.
Given the integral relationship between work-related stress, job dissatisfaction, burnout, and patient care, properly addressing nursing burnout is essential. The purpose of this course is to provide nurses with information to identify burnout and with effective strategies to manage work-related stress and prevent burnout.
Upon completion of this course, you should be able to:
- Define burnout and its relationship to job dissatisfaction and stress.
- Describe the developmental stages of burnout.
- Identify work environment and personal risk factors for burnout.
- Describe the personal and professional consequences of nursing burnout and the nursing shortage.
- Describe tools available to assess for and identify burnout.
- Identify strategies for individuals and institutions/organizations to help prevent and cope with burnout.
Lori L. Alexander, MTPW, ELS, MWC, is President of Editorial Rx, Inc., which provides medical writing and editing services on a wide variety of clinical topics and in a range of media. A medical writer and editor for more than 30 years, Ms. Alexander has written for both professional and lay audiences, with a focus on continuing education materials, medical meeting coverage, and educational resources for patients. She is the Editor Emeritus of the American Medical Writers Association (AMWA) Journal, the peer-review journal representing the largest association of medical communicators in the United States. Ms. Alexander earned a Master’s degree in technical and professional writing, with a concentration in medical writing, at Northeastern University, Boston. She has also earned certification as a life sciences editor and as a medical writer.
Contributing faculty, Lori L. Alexander, MTPW, ELS, MWC, has disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
Mary Franks, MSN, APRN, FNP-C
The division planner has disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
Sarah Campbell
The Director of Development and Academic Affairs has disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
The purpose of NetCE is to provide challenging curricula to assist healthcare professionals to raise their levels of expertise while fulfilling their continuing education requirements, thereby improving the quality of healthcare.
Our contributing faculty members have taken care to ensure that the information and recommendations are accurate and compatible with the standards generally accepted at the time of publication. The publisher disclaims any liability, loss or damage incurred as a consequence, directly or indirectly, of the use and application of any of the contents. Participants are cautioned about the potential risk of using limited knowledge when integrating new techniques into practice.
It is the policy of NetCE not to accept commercial support. Furthermore, commercial interests are prohibited from distributing or providing access to this activity to learners.
Supported browsers for Windows include Microsoft Internet Explorer 9.0 and up, Mozilla Firefox 3.0 and up, Opera 9.0 and up, and Google Chrome. Supported browsers for Macintosh include Safari, Mozilla Firefox 3.0 and up, Opera 9.0 and up, and Google Chrome. Other operating systems and browsers that include complete implementations of ECMAScript edition 3 and CSS 2.0 may work, but are not supported. Supported browsers must utilize the TLS encryption protocol v1.1 or v1.2 in order to connect to pages that require a secured HTTPS connection. TLS v1.0 is not supported.
The role of implicit biases on healthcare outcomes has become a concern, as there is some evidence that implicit biases contribute to health disparities, professionals' attitudes toward and interactions with patients, quality of care, diagnoses, and treatment decisions. This may produce differences in help-seeking, diagnoses, and ultimately treatments and interventions. Implicit biases may also unwittingly produce professional behaviors, attitudes, and interactions that reduce patients' trust and comfort with their provider, leading to earlier termination of visits and/or reduced adherence and follow-up. Disadvantaged groups are marginalized in the healthcare system and vulnerable on multiple levels; health professionals' implicit biases can further exacerbate these existing disadvantages.
Interventions or strategies designed to reduce implicit bias may be categorized as change-based or control-based. Change-based interventions focus on reducing or changing cognitive associations underlying implicit biases. These interventions might include challenging stereotypes. Conversely, control-based interventions involve reducing the effects of the implicit bias on the individual's behaviors. These strategies include increasing awareness of biased thoughts and responses. The two types of interventions are not mutually exclusive and may be used synergistically.
#31434: Burnout: Impact on Nursing and Quality of Care
Work social structure, politics, and interpersonal relationships can all be significant sources of stress, regardless of occupation. According to a 2017 nationwide survey by the American Psychological Association (APA) and the American Institute of Stress (AIS), 61% of employees in the general population reported being affected by work-related stress; in 2023, strongly exacerbated by the coronavirus disease (COVID-19) pandemic, 77% of workers reported having experienced work-related stress in the past month [1,4]. In addition, 57% indicated that negative effects of work-related stress were a precipitating factor of a mental illness and/or workplace burnout [1,4]. With more than 160 million individuals in the U.S. workforce, workplace stress and burnout is a major societal issue [5].
In addition, work-related stress is associated with high direct and indirect costs related to absenteeism, decreased productivity, and employee turnover, as well as a wide variety of physical conditions, from headaches and insomnia to cardiovascular and immune diseases[1,2,4,5]. Work-related stress that is left unaddressed has the potential to develop into burnout. The costs of burnout are even higher than stress and affect not only the well-being of the individual but that of the individual's family, friends, and colleagues. Burnout has been more prevalent in the helping professions, and high levels of burnout have been documented in the healthcare professions, especially among nurses.
This course provides an overview of nursing burnout, addressing the scope of the issue, how burnout develops, and the risk factors that make nurses especially susceptible to burnout. After a discussion of the primary sources of work-related stress, job dissatisfaction, and burnout among nurses, several strategies for preventing burnout at the individual and organizational level are presented.
While nursing burnout is a global issue, this course is built primarily on research in U.S. institutions.
The term "burnout" originated in the 1940s as a word to describe the point at which a jet or rocket engine stops operating [15]. The word was first applied to humans in the 1970s by the psychiatrist Herbert Freudenberger, who used the term to describe the status of overworked volunteers in free mental health clinics [16]. He compared the loss of idealism in these volunteers to a building—once a vital structure—that had burned out, and he defined burnout as the "progressive loss of idealism, energy, and purpose experienced by people in the helping professions as a result of the condition of their work" [17].
Use of the term burnout is now widespread (perhaps overused), and definitions have varied since the time the word was first applied to humans. The term has been used to describe a mild degree of unhappiness caused by stress, as well as any degree of distress, from fatigue to major depression [18]. In the early 1980s, social psychologist Christina Maslach and her colleagues began to explore the loss of emotional feeling and concern for clients among human services professionals. Since then, she has researched burnout extensively, becoming a leading authority on the topic and the author of the criterion standard tool to assess burnout, the Maslach Burnout Inventory (MBI) [19,20,21].
Maslach emphasizes that burnout is not a problem related to an individual [21]. Instead, her research indicates that burnout is a problem of the social environment in which people work and is a function of how people within that environment interact with one another and perform their jobs [21]. She notes that burnout is more likely when there is a "major mismatch between the nature of the job and the nature of the person who does the job" [21]. These mismatches are at the core of the development of burnout. The term burnout is now usually limited to mean burnout as described by Maslach: a syndrome of emotional exhaustion, depersonalization, and reduced personal accomplishment [18].
In the last several decades, a better understanding of burnout and the effects on mental health have evolved. As a result, in 2013, burnout was included in the International Classification of Diseases, 10th edition (ICD-10), in the chapter Factors Influencing Health Status or Contact with Health Services. However, the definition was limited and simply defined as a "state of vital exhaustion," and the definition was not related specifically to an individual's occupation [26].
In January 2022, the 11th edition of the ICD (ICD-11) went into effect, and included an expanded definition and new code. The ICD-11 defines burnout as [34]:
a syndrome conceptualized as resulting from chronic workplace stress that has not been successfully managed. It is characterized by three dimensions: (1) feelings of energy depletion or exhaustion; (2) increased mental distance from one's job, or feelings of negativism or cynicism related to one's job; and (3) reduced professional efficacy.
Burnout refers specifically to phenomena in the occupational context and should not be applied to describe experiences in other areas of life.
It is important to note that burnout, as defined by the ICD-11, is not classified as a medical condition, but rather an occupational phenomenon [34]. Burnout can occur in any occupational setting, although it has been studied most extensively in a wide range of occupations within the human services field, including healthcare professionals to teachers, police, and prison workers [18,22,34]. High levels of burnout among healthcare professionals have been well-documented. This has received increased attention following the COVID-19 pandemic; as a result, several papers and guidelines on the topic have been have been published, including the 2022 Surgeon General's Advisory Addressing Health Worker Burnout [6].
Nurses represent the largest faction of healthcare professionals, with nearly 4.4 million actively licensed RNs and APRNs and another 600,000 LPNs/LVNs in the United States, and they are the frontline for direct patient care in hospitals [3,45]. Burnout in nursing, while always present, has received a long-warranted amount of attention following the extreme conditions and stress related to the COVID-19 pandemic. An estimated 82.3% of nurses who had been employed in the same position for at least one year indicated that they had felt burned out at some point in their career, and 88.8% of those nurses indicated that their feelings of burnout had increased during the pandemic [45].
As mentioned, the major defining component of burnout is that it occurs as a result of factors in the workplace. Job stress can cause or exacerbate physical and mental health issues in nurses and decrease energy and work efficiency. Inadequate nursing staff levels caused by excessive turnover have been significantly associated with nursing errors and poorer patient outcomes, and higher levels of burnout have been associated with lower ratings of the quality of care [7,8]. Researchers estimate that the staffing shortage of RNs will reach nearly 1 million by 2030 [3,10]. Increased efforts to understand shortage dynamics are warranted, as the deficit remains, and further efforts are underway to strengthen the nursing workforce [3,10]. Thus, enhancing job satisfaction and avoiding burnout is crucial to maintaining an adequate population of nurses, and an adequate population of nurses is vital to maintaining high-quality patient care.
Compounding existing issues, frontline healthcare workers working during the COVID-19 pandemic were exposed to threats to physical safety from infection, insufficient resources, continuous changes in roles and responsibilities, high patient acuity and mortality rates, long shifts, inadequate rest, and inadequate personal protective equipment [18]. Each of these factors likely increased perceived job demands and reduced perceived and real resources in ways that exacerbated burnout for healthcare workers.
The economic burden of job-related stress and burnout is difficult to ascertain, although it is estimated that the direct and indirect costs of work-related stress among nurses total $200 million to $300 million annually in the United States. It is also estimated that nearly 90% of employees' physical and/or mental health issues are related to or exacerbated by stress on the job [46].
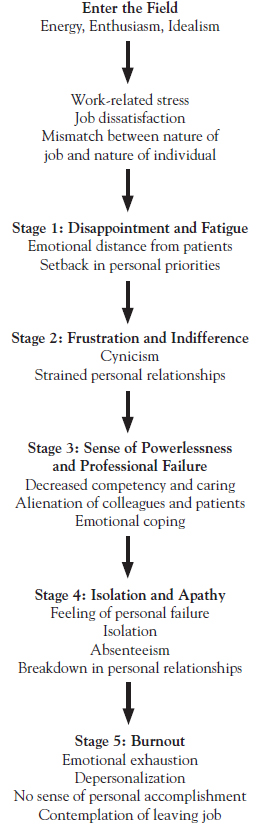
Burnout can develop in any line of work, and while precipitating factors vary by individual and work type, there is a general pattern, or stages, that will eventually lead to burnout if not addressed. There are several differing descriptions of the stages in the development of burnout, and organizations/publications may have a different number of stages based on expanded or condensed information. One of the most common models describes five stages of burnout pertinent to the nursing experience [6,18].
In general, when an individual first enters a chosen career, they are excited and motivated. If the work environment is not supportive of the individual's efforts and concerns, the reality of the job and the individual's expectations begin to diverge and frustration and disappointment can arise [18]. These feelings often lead to job dissatisfaction, resulting in decreased productivity, loss of confidence and enthusiasm, and/or behavior changes. If the situation is not addressed, stress accumulates and causes typical stress-related symptoms. These physical symptoms, when coupled with emotional distance, signify the first stage of burnout: mental and physical exhaustion [18]. If these symptoms are not addressed, they will evolve over four more stages: frustration and indifference, feelings of powerlessness and failure as a professional, isolation and apathy, and true burnout. For nurses, these stages affect not only them and their family and friends, but also their peers and patients (Figure 1) [6,18].
The specific factors within the work environment that lead to stress and burnout vary across occupations and among individuals, but, as the COVID-19 pandemic proved, nurses are especially vulnerable to burnout. While the root of burnout is traditionally thought to be within the work environment, research conducted during and immediately after the COVID-19 pandemic has shown that burnout is highly prevalent, multifaceted, and can be precipitated by any combination of societal pressures, employment conditions, and individual demographics and personality traits (Table 1) [6,13,18].
POTENTIAL RISK FACTORS FOR BURNOUT
| Dimension | Risk Factor | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Societal and cultural |
| ||||||||||||
| Healthcare system |
| ||||||||||||
| Organizational |
| ||||||||||||
| Work environment |
| ||||||||||||
| Demographic variables |
| ||||||||||||
| Individual personality traits |
|
Among nurses, burnout is often directly linked to work-related stress and job dissatisfaction. A systematic review demonstrated that work-related stress is significantly related to job satisfaction, with higher stress levels associated with less job satisfaction [70]. Further, low job satisfaction is associated with burnout [70]. In 2022, a large-scale survey of nearly 18,000 nurses showed that 71% were satisfied with their career choice (the majority reported they were "extremely satisfied"), a 10% decrease in satisfaction from the previous decade. The study found that about half of nurses reported feeling emotionally drained (50.8%), used up (56.4%), fatigued (49.7%), burned out (45.1%), or at the end of the rope (29.4%) a few times per week or every day [37]. Given these facts, an understanding of the prevalence and causes of job dissatisfaction among nurses can help to define the sources of stress and burnout. Studies have indicated that among nurses, factors within the work environment are greater predictors of job dissatisfaction and nurse retention than factors related directly to the care of patients [45].
Societal and cultural factors have been shown to be a major component to the risk of burnout in nursing. In the United States, the COVID-19 pandemic brought with it an increased intrusion of politics into medical care. While society was largely supportive of healthcare workers during the first 12 months of the pandemic, individual opinions became divided due to growing frustration, resentment, and politicization of science and public health; healthcare workers often found themselves on the receiving end of the backlash, increasing stress and moral distress and negatively affecting personal mental health and professional practice.
One post-pandemic survey indicated that nearly 92% of physicians felt stress related to the politization of the pandemic, largely because of conversation surrounding non-approved therapies, mask wearing policies and compliance, and increased work hours. Nurses similarly felt the strain of politics, society, and culture during the pandemic [14].
Healthcare systems' contribution to nursing burnout is usually in the form of policies and procedures that inhibit nurses' ability to complete their jobs to the best of their ability and skill. Other health system-related risk factors are limitations from national and state regulations, misaligned reimbursement policies, burdensome administrative paperwork and documentation requirements, and poor or out-of-touch care coordination. Healthcare system stressors play a role in nursing burnout, which leads to nursing shortages and retention challenges, limited services available, risk of malpractice, increased costs, and decreased patient satisfaction, perpetuating the cycle [6].
Organizational risk factors for nursing burnout include lack of leadership support, lack of clinical autonomy, barriers to mental health and substance use care, and biased and discriminatory practices. In addition, ensuring living and competitive wages, paid sick and family leave, enforced rest breaks, balanced workloads, safe work hours, educational debt support, and family-friendly policies are all important factors to reducing nurse burnout at the organizational level. The Surgeon General's Advisory established a national goal to "transform organizational cultures to prioritize health worker well-being and show all health workers that they are valued. Employers, policymakers, and professional associations can support health workers by identifying and measuring factors contributing to burnout, and co-developing solutions to respond to and prevent it, while advancing worker well-being" [6].
An individuals' work environment is comprised of the setting, social aspects, and physical conditions relating to employment. An increased risk of burnout occurs when an individual's experience (actual or perceived) does not match one or more of these situational factors in a work environment [21].
Among nurses, it has been found that job dissatisfaction varies significantly according to position and setting. In 2017, a survey among RNs indicated that approximately 11% were moderately (8.5%) or extremely (2.5%) dissatisfied with their primary nursing position; in 2021, these rates increased to 14.7% and 5.2%, respectively [23]. In addition, between 2017 and 2021, nurses who indicated that they were extremely satisfied in their primary position fell from 40.2% to 27.6% [44]. In a 2022 nationally representative survey of nurses, burnout was the second most likely reason given for leaving the nursing field completely, following only retirement (Table 2) [45].
REASONS GIVEN FOR LEAVING A NURSING JOB OR POSITION, 2022
| Specific Work-Related Reason | Percentage |
|---|---|
| Leaving for a Different Nursing Job or Position | |
| Burnout | 51.2% |
| Inadequate staffing | 46.1% |
| Stressful work environment | 45.3% |
| Seeking better pay or benefits | 41.1% |
| Lack of good management/leadership | 39.5% |
| Received promotion or career advancement | 23.7% |
| Scheduling issues and inconveniences | 22.7% |
| High-risk working conditions | 19.6% |
| Physical demands of job | 15.0% |
| Lack of advancement opportunities | 14.9% |
| Leaving Nursing Completely | |
| Retirement | 47.2% |
| Burnout | 35.8% |
| Stressful work environment | 28.3% |
| Inadequate staffing | 25.1% |
| Lack of good management/leadership | 23.2% |
| Family caregiving obligations | 18.2% |
| Physical demands of job | 13.5% |
| Scheduling issues and inconveniences | 13.1% |
| High-risk working conditions | 11.5% |
| Lack of collaboration | 9.3% |
Factors contributing to stress and burnout may differ according to specialty. For example, substandard staffing was associated with burnout among oncology nurses, whereas low manager support was a significant predictor of burnout among emergency room nurses [79,83]. In 2021, rates of moderate or extreme job satisfaction were lowest for nurses in orthopedics (71%), general medical/surgical (72%), and pulmonary or respiratory nursing (72%); the highest rates were found for psychiatric and mental health nurses (85%), occupational health nurses (84%), and geriatric nurses (84%) [45]. The change in job satisfaction between 2017 and 2021 (pre- and during-pandemic) in certain specialty areas were especially prominent; there was a 16.1% decrease in satisfaction among nurses in orthopedics, followed by a 16% decrease in infectious and communicable disease nursing, and a 15% decrease in satisfaction in delivery/neonatal care [45].
With regard to setting, the highest rates of job dissatisfaction have been reported among nurses in nursing homes and hospitals, even for nurses who do not provide direct patient care [45]. Job satisfaction in 2021 was highest among nurses employed in outpatient, ambulatory, and other clinical settings. In a survey of more than 95,000 nurses, the most common sources of dissatisfaction for hospital and nursing home nurses were opportunities to advance, professional status, work schedule, and independence at work [68]. Salary/wages and benefits (e.g., health insurance, retirement, tuition reimbursement) have also been common sources of dissatisfaction but have had little influence on burnout [68,69].
Other work environment factors associated with stress and nursing burnout include lack of collaboration and work community; limited time with patients; absence of focus on employee well-being; insufficient professional recognition; and harassment, violence, and discrimination [6,13,21].
These sources of work environment dissatisfaction can be correlated with four of the mismatches identified by Maslach, namely, work overload, lack of control, insufficient reward, and absence of community (Table 3) [18,70]. An additional factor that should be considered is the emotional demands of nursing.
CORRELATION OF SOURCES OF DISSATISFACTION AND AREAS OF MISMATCH
| Area of Mismatch | Dissatisfaction | Specific Factors | ||||||
|---|---|---|---|---|---|---|---|---|
| Work overload |
|
| ||||||
| Lack of control | Role conflict, insufficiency, and/or ambiguity |
| ||||||
| Insufficient reward | Lack of professional recognition or reward |
| ||||||
| Absence of community | Poor relationships with other healthcare professionals |
|
A major source of burnout, work overload is created primarily by inadequate staffing, a prevalent problem in today's hospitals and nursing homes [65,69,72,79]. Studies have shown that the mean patient-to-nurse ratio in U.S. hospitals is approximately 5:1 [69,74]. Nurses have consistently reported that these ratios are inadequate for providing high-quality care. In a study of 534 hospitals (26,005 nurses), staffing was considered to be poor in 25% [69]. In a survey of nearly 11,000 RNs, only 46% said there was enough staff to accomplish the necessary work and 48% said there were not enough RNs on staff to provide high-quality care [67]. A 2022 survey showed that that only 33% of nurses had the time needed to spend with patients [43]. A 2021 study in New York State demonstrated a savings of 4,370 patient lives and a cost savings of $720 million when hospitals were staffed at a 4:1 patient-to-nurse ratio [44]. Increased patient-to-nurse ratios are associated with lower rates of job satisfaction and higher rates of burnout; inadequate staffing was the reason that 46.4% of still-employed nurses gave for changing their position or employer, and the reason that 35.8% of nurses left the profession altogether [7,45,70]. In a study of more than 10,000 nurses, the rate of burnout increased 23% for every additional patient per nurse [7].
Other factors also contribute to increased workload, including a high number of work hours per week, extended shifts, overtime (often mandatory), many consecutive days of work, rotating shifts, weekend work, and on-call requirements. Among more than 235,000 nurses in a 2022 survey, nearly 30% worked more than 40 hours per week, with 19% working 41 to 50 hours per week and 10.6% working more than 50 hours per week [37]. In addition to long work weeks, nurses typically work long workdays. Twelve-hour shifts offer many benefits to nurses and patient care, and as a result, the percentage of nurses who routinely work these shifts has increased to approximately 65% to 80% [94]. However, moderate-to-high levels of acute fatigue and moderate levels of chronic fatigue have been found among nurses working 12-hour shifts [95]. Several studies have indicated a strong relationship between long work hours or 12-hour shifts and adverse nurse outcomes, such as increased fatigue, job dissatisfaction, burnout, and intention to leave the job [94,96].
The increase in working hours for nurses has substantial professional consequences. The odds of job dissatisfaction and burnout are as much as 2.5 times higher for nurses who work longer shifts compared with nurses who worked eight- to nine-hour shifts [94]. Most importantly, fatigue and long hours have been significantly associated with nursing errors [97]. Twelve-hour shifts have been linked to up to three times a higher risk of error [97]. Long shifts (10 hours or more) have also been associated with a greater odds of nurses reporting that the quality of care is fair or poor on their unit compared with shifts of 8 to 9 hours [66].
Shift length has also been associated with patients' perceptions of the quality of care. In a study of 577 hospitals in four states, patients' ratings for 7 of the 10 outcomes on the Hospital Consumer Assessment of Healthcare Providers and Systems survey were significantly adversely affected by the proportion of nurses who worked shifts of 13 hours or more [94]. These lower ratings included the global assessments of overall rating for the hospital and whether the patient would recommend the hospital [94].
Also contributing to fatigue—and its consequences—are rotating shifts and mandatory overtime, which have often been used to solve staffing issues [97].
The amount of medical information available online has raised the levels of patient knowledge but may also increase the number of questions and/or amount of explanation required, in turn contributing to further workload. Advances in treatment have also led to nursing care that can be demanding and challenging. This high level of care, coupled with shorter stays as a result of changes in the healthcare system and reimbursement, result in nursing workloads that are not balanced across various levels of care within the patient population.
Documentation requirements with electronic health records are another source of stress and time. Studies have shown that nurses spend between 15% to 40% of their time at work on electronic health records and documentation requirements [6,80,81].
Many of these sources of dissatisfaction are directly related to nursing turnover, as they have been given as the reason for nurses leaving their job or position. In a 2022 representative survey, a stressful work environment was the reported reason that 45.3% of still-employed nurses left their jobs and the reported reason 28.3% of nurses were no longer employed in nursing [45]. A 2017 survey of 600 RNs conducted by RNnetwork found similar results, with approximately 50% of the nurses having considered leaving nursing due to feeling overworked (27%), not enjoying their job anymore (16%) and spending too much time on paperwork (15%) [65]. The survey also found that more than 50% of the RNs surveyed did not feel respected by their administration, citing that as a reason for considering leaving nursing. In addition, 43% of respondents indicated that their workplace did not support a healthy work/life balance [65].
A sense of control, or autonomy, is important to nurses, and job satisfaction is greater and job stress is lower when nurses feel as if they have some control over how they perform their job. A strong correlation has been identified between job satisfaction and autonomy, empowerment, and control [70,89]. Autonomy in nursing refers to having "the authority to make decisions and freely act in accordance with one's professional knowledge and skills to implement those decisions. It is identified with characteristics including competence, knowledge, decision-making, self-governance, freedom, self-control, responsiveness, and judgment" [89]. Autonomy within the workplace generally falls into two areas: clinical autonomy and practice autonomy. Clinical autonomy is an individual's authority to make independent judgments and decisions about patient care within their scope of practice and ability. Practice autonomy is the individual's influence over their practice setting and includes decisions about organization rules, policies, procedures, structure, and operations. Studies have found that autonomy, empowerment, and decision-making opportunities are strongly related to job satisfaction and retention among nurses [89].
The risk of burnout is increased among nurses who perceive a lack of control in their work environment [82]. A sense of control varies across nursing specialties, which in part explains the range of burnout rates among specialties. For example, in a study of nurse managers, emergency department nurses, and nurse practitioners, the least amount of control was reported by emergency department nurses, who also had the highest rate of burnout; in contrast, nurse practitioners reported having the most control and the lowest rate of burnout [82].
Insufficient reward relates to several aspects, including lack of recognition of contributions, inadequate compensation (salary), and few opportunities for advancement. Being fairly rewarded and recognized for contributions is important to nurses, and nurses who perceive respect and recognition are more likely to be satisfied with their job and to have a lower likelihood of burnout [6,60]. In multiple studies, a culture that supports the nursing profession was the factor most strongly associated with job satisfaction [45,58]. Another study found that approximately 34% of nurses feel that their employers do not treat them with respect, do not make good use of their skills and abilities, and the lack of recognition in the work environment does not motivate them to go above and beyond [59]. Lack of professional recognition and professional uncertainty have also both been significantly associated with all three subscales on the MBI [70].
Although wage has been associated with job dissatisfaction and intent to leave, it is thought to have little effect on burnout, and nurses have fairly consistently ranked other work environment factors as being of more concern than money [69]. It is important to note, however, that a 2019 survey of nearly 20,000 registered nurses found that nearly one in five nurses work a second nursing job and nearly one in ten work a second full-time job, potentially impacting both quality of care and the quality of life for nurses [49].
The nurse's community consists of peers, nursing leaders, and physicians. Positive, supportive relationships with all these constituencies have been related to job satisfaction and a decreased likelihood of stress and burnout. In contrast, lack of peer cohesion, inadequate administrative and supervisor support, and difficulties with nurse-physician interactions, have all been factors in high rates of burnout, especially on the emotional exhaustion and depersonalization subscales [6,18].
Nurse-Peer Relationships
In one survey of 76,000 registered nurses, the highest level of satisfaction was given to relationships with other nurses. Still, the survey showed that one-third of nurses were dissatisfied with interactions with their peers [112]. A 2017 survey of 600 nurses found that 45% had been verbally harassed by other nurses [65]. Interpersonal conflict with other nurses is a stress factor in and of itself, but a lack of close working relationships deprives nurses of their colleagues as a source of support. This lack of support is important, as nurses have ranked their peers as providing the most support within the hospital community, and higher levels of support from co-workers have been related to lower levels of emotional exhaustion on the MBI. Similarly, lack of peer cohesion has correlated with high levels of emotional exhaustion and depersonalization, or cynicism [6].
Although resolving conflicts can mitigate stress, the style of conflict resolution has also been a significant predictor of burnout. A study of three conflict resolution styles—avoidance, confrontational, and cooperative—showed that the avoidance and confrontational styles were associated with a higher rate of burnout, while the cooperative style was associated with a lower rate [113,114].
Nurse-Nurse Leader Relationships
Support from nursing leaders and administration is essential for nurses' job satisfaction. Studies have indicated, however, that most nurses do not have or perceive supportive leadership. Approximately 45% to 70% of nurses are dissatisfied with nursing management and administration because they do not listen to or address nurses' concerns or deal with nurses truthfully about decisions affecting their jobs [67,71,112]. One study found that 41% of nurses reported having been verbally harassed by managers or administrators [65,71]. Approximately 53% to 62% of nurses think they have a nurse manager who is a good manager and leader or have a head nurse who backs nursing staff in decision-making [67,71]. Another survey found that 82% of respondents believed that more nurse leaders are needed in health care; however, 61% of also indicated that they were not interested in moving into a leadership position [71] Leadership style and lack of administrator and supervisor support has been related to both job satisfaction and burnout. Among emergency department nurses, a low level of manager support was a significant predictor of burnout [83].
Nurse-Physician Relationships
Nurse-physician relationships and their effect on nurses have an extensive history. Daily interactions between nurses and physicians strongly influence nurses' morale, and difficulties in nurse-physician relationships are perceived by most nurses, physicians, and hospital executives as having negative or worsening effects on stress, frustration, concentration, communication, collaboration, and information transfer between nurses and physicians [47]. One study showed that nurses value collaborative relationships with physicians, and place more importance on the collaboration than do physicians [116]. The findings of surveys have varied with regard to nurses' perceptions of nurse-physician relationships at their facility. In a statewide survey, 72% of nurses said collaboration existed between nurses and physicians and 80% said nurses and physicians had good working relationships [67]. In addition, studies have shown that better nurse-physician collaboration and communication lead to faster patient throughput, shorter hospital stays, increased patient satisfaction, fewer adverse events, and improved patient outcomes [47].
Studies have indicated that positive nurse-physician relationships significantly correlate with lower emotional exhaustion and depersonalization and higher personal accomplishment [64]. Similarly, a low score on organizational climate (of which nurse-physician collaboration is a factor) has correlated with high rates of burnout.
The emotional demands of the nursing profession are well recognized, and human suffering has been noted to be a stressor for nurses. In a 2022 American Nurses Foundation survey, 33% of nurses said they were "not emotionally healthy" or "not at all emotionally healthy," and 75% reported feeling stressed, frustrated, and exhausted [48]. In addition to the stressful nature of nursing, the COVID-19 pandemic and associated loss of more than 1 million lives affected nurses emotionally and collectively unlike anything in recent history. Often being on the frontline of care, with limited knowledge of the virus in the first weeks, limited available protection equipment and resources, and mass patient influx, nurses were put in a unique and stressful situation that continues in the post-pandemic healthcare environment [48].
Emotional demands are greater in settings such as oncology, palliative care, and critical care, where grief and loss have been identified as a source for stress among nurses and other healthcare professionals. The sense of loss extends beyond the loss of the relationship with the patient to identifying with the pain of the family, past unresolved loss and anticipated future loss, and loss of one's goals and expectations. Nurses in these settings may experience stress when they cannot provide adequate care at the end of life or help a patient die a "good death" [118].
Demographic variables have been studied in relation to burnout, and several have been found to influence the risk of burnout, alone or in combination, including [18]:
Age (younger than 25 years of age)
Race/ethnicity
Family status
Educational status
Gender
Personality traits
In the 2022 American Nurses Foundation study, among the 30% of all nurses who reported being "not emotionally healthy" or "not at all emotionally healthy," 46% were younger than 25 years of age (compared with 19% for those 55 years of age and older) [48]. In terms of burnout, studies have shown that burnout levels are high among nurses (high scores on the MBI), and age was a factor [40]. In one study, researchers found that levels of burnout were higher among nurses younger than 30 years of age than among nurses older than 30 years of age [40].
Burnout is less prevalent among older individuals because they tend to have a more balanced perspective on life [18,14]. Research from Maslach indicated that the increased rate of burnout among younger individuals is a function of a "survival of the fittest" concept. Burnout usually occurs early in one's career (in the first one to five years), and many young, burned out individuals leave the profession; as a result, the remaining individuals in an occupation are the "survivors" [18]. Research has supported this, with one study finding a correlation between younger age (and less than 10 years in nursing field) and lack of problem-solving/life skills that are essential in the extreme situations often encountered in nursing. Furthermore, increased age has correlated with more positive coping skills (e.g., receiving emotional support from others, spirituality) and younger age with more negative coping skills (e.g., alcohol and drug use). Although both groups showed similar rates of emotional exhaustion, the younger group had higher rates of cynicism and depersonalization and lower rates of job satisfaction [14].
Comparing burnout across racial/ethnic groups is difficult, but more information is becoming available. While no statistical significance has been found directly linking race/ethnicity to burnout, job dissatisfaction and emotional distress have been seen in greater numbers in non-White nurses. For example, Black nurses (92%) experienced the highest numbers of workplace racial microaggressions from leaders, patients, and/or peers, followed by Asian nurses (73%), Hispanic nurses (69%), and White nurses (28%). An analysis of the 2022 survey of RNs showed that the risk for job dissatisfaction was greater for Black, American Indian/Alaska Native, and multiracial nurses than for White nurses [43]. No clear difference in job satisfaction could be found among Hispanic, Native Hawaiian/Pacific Islander, and White nurses [43]. In a 2017 survey of physicians, similar rates of burnout were seen among all racial/ethnic groups in the United States, with Chinese physicians experiencing a slightly greater prevalence than the national average (56% vs. 52%), and Hispanic/Latino and Black physicians experiencing slightly less burnout (51% and 48% vs. 52%, respectively). Asian Indian physicians were least likely to experience burnout (46%) [76]. Non-White nurses tend to leave their nursing position at a rate of nearly twice that of White nurses [29]. A nationwide survey by the National Commission to End Racism in Nursing found that 63% of nurses have experienced racism in the workplace, and 56% report that it has negatively affected their professional well-being. Among the 57% of respondents who reported having challenged racism in the workplace, 64% indicated that their effort did not result in a change [30]. Efforts to confront systemic racism in the nursing profession are paramount to the mental health of nurses and the outcomes of their patients.
Family status also seems to play an important role in burnout; rates of burnout are higher among single workers and workers with no children than among married workers and those with children [18]. The emotional resources provided by a family are thought to be the reason for this difference.
Educational status seems to have an effect, with higher levels of burnout among workers with higher levels of education [18]. This difference could be the result of the expectations associated with advanced education and job choices [18].
Differences in job satisfaction, stress, and burnout according to gender are not well known because of the predominance of women in nursing (approximately 90%) [45]. Across most work settings, levels of burnout have been somewhat consistent among men and women. One meta-analysis demonstrated similar overall rates of burnout among men and women, but there were gender differences in burnout components, with slightly higher levels of emotional exhaustion among women and somewhat higher levels of depersonalization among men [24]. Limited data have indicated that the rates of job satisfaction do not differ between male and female nurses [77]. No studies were found in which rates of burnout were compared for male and female nurses working in the United States. However, one meta-analysis demonstrated that the rates of emotional exhaustion were higher for women than men in female-typed occupations [29]. Gender differences have also been found with respect to other demographic variables [18]. For example, a survey of 3,424 employees in a Finnish study indicated that a low educational level and low social status increased the risk of burnout for women, whereas marital status (single, divorced, or widowed) increased the risk for men [25].
Studies have also been completed to explore relationships between personality traits and the risk of burnout. Maslach noted that characteristics such as low self-esteem or lack of confidence, failure to recognize personal limits, need for approval, drive to overachieve, need for autonomy, impatience, intolerance, and empathy increased susceptibility to burnout [18]. Others have postulated that extreme conscientiousness, perfectionism, and self-giving (selflessness) also increase susceptibility, as does a type D personality (a joint tendency for negative emotions and social inhibition) [6,18].
Many of the personal risk factors described here are common among nurses and other healthcare professionals; in fact, several are essential for success in the healthcare field. This may explain, in part, the high levels of burnout among nurses.
Nurses are susceptible to the same physical, psychological, and interpersonal/social effects of stress and burnout as the general workforce. However, the stakes are higher for nurses, as the consequences of nurse burnout have serious implications not only for nurses but also for patients.
Studies have indicated that nurses' physical and mental health are negatively affected by many work-related stressors, including lack of social support from peers, work overload, high job demands, low job control, and nurse-physician conflict [70]. It has been shown that health can be adversely affected by stress and burnout, with a range of physical symptoms from headaches to chronic pain to gastrointestinal distress. Mental health symptoms often include anxiety and depression. In addition, burnout can result in chronic feelings of guilt and inadequacy, affecting self-worth and need for purpose [57,61].
A variety of professional consequences are related to prolonged stress and burnout, and poor work performance is the ultimate result. Emotional exhaustion leads to absenteeism and decreased productivity, both of which affect work overload for other nurses [6,18]. As a result, burned out individuals create distance between themselves and patients as well as colleagues (referred to as depersonalization). Maslach described the detrimental change in a burned-out individual's work performance [18]:
Motivation is down, frustration is up, and an unsympathetic, don't-give-a damn attitude predominates. They don't take care in making their judgments, and they don't care as much about the outcome. They 'go by the book' and are stale rather than innovative and fresh. They give the bare minimum rather than giving their all, and sometimes they give nothing at all.
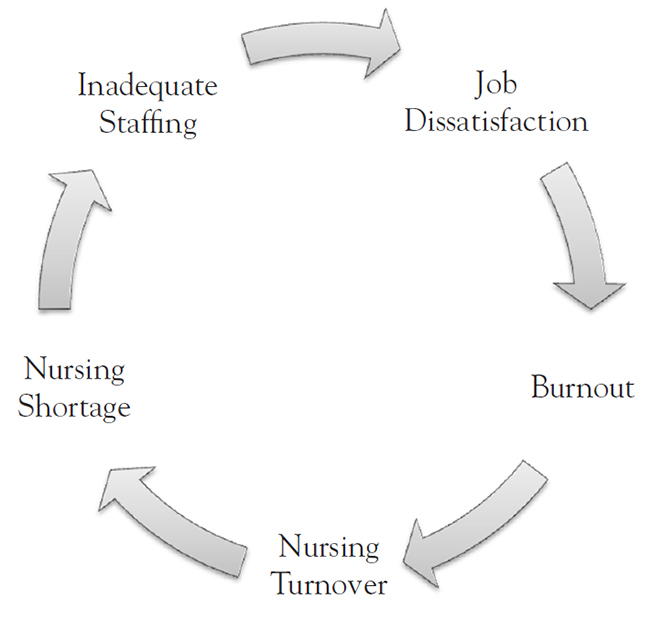
Perhaps the greatest professional consequence of nurse burnout is the nursing shortage. High turnover among nurses as a result of job dissatisfaction and burnout is a driving contributor to the nursing shortage [9,65,71]. Other factors are an aging nursing workforce and increased health demands in the general population [10]. The supply of nurses has been declining since the late 1990s, while the demand for nurses has been increasing. The downturn in the U.S. economy in the early 2000s eased the nursing shortage in the short term, but the shortage is still projected to grow to nearly 1 million by 2030 [10]. The problems of burnout and the nursing shortage escalate in a cyclical manner: job dissatisfaction leads to burnout, nursing turnover, and inadequate staffing, which further increases job dissatisfaction (Figure 2) [70].
The nursing shortage has far-reaching effects on the quality of care and patient safety. A multitude of studies have demonstrated that factors caused by the shortage—primarily, inadequate staffing and hours worked—significantly affect nurses' perceived quality of care, patient satisfaction, the potential for nursing errors, adverse events for patients, and patient mortality.
Perceived Quality of Care and Patient Satisfaction
As already mentioned, high proportions of nurses have noted that there are not enough registered nurses on staff to provide high-quality patient care [10,37,65,75]. Nurses report the feeling that, in general, the quality of patient care is declining, and this feeling increases with age; 37% of nurses 19 to 39 years of age agreed that the quality of care is declining, compared with 56% of nurses 40 to 54 years of age and 66% for nurses 55 years and older [73].
Some studies have addressed nurses' perceptions about the quality of care in relation to burnout. In a study of nurses at 198 hospitals, all three subscales of the MBI were significant predictors of nurses' fair/poor quality ratings of care [13]. The findings of other studies have similarly shown a relationship between rates of burnout and nurses' ratings of fair or poor quality of care [72].
Higher levels of burnout and job dissatisfaction are also associated with lower patient satisfaction. In one study, rates of patient satisfaction were lower in hospitals with higher rates of nurses who were dissatisfied or burned out [68].
Nursing Errors
Several surveys have indicated that nursing errors are, in many cases, perceived by nurses to be a result of the nursing shortage [8,63,68]. For example, in one study, 78% of surveyed nurses said they had not given a prescribed medication or had given it at the wrong time, and 69% of these nurses believed the error was somewhat or strongly related to the nursing shortage. In addition to the harm to patients, medication and treatment errors caused moral distress for 73% and 61% of the nurses involved, respectively [8]. In the other study, 36% of hospital nurses and 47% of nursing home nurses said that their workload caused them to miss important changes in their patients' condition [68]. A different study found that 46.8% of nurses had committed a medication error within the past year, with incorrect infusion rates (33.3%) and administering two doses of medicine instead of one (23.8%) being the most common errors. Almost two-thirds of these errors were not reported by the nurse. The foremost reason cited for these errors was a shortage of nurses (47.6%) [63]. As noted earlier, long work hours and nurse fatigue have also contributed substantially to nursing errors [6,63,68,97].
Adverse Events
The findings of studies have consistently demonstrated a relationship between inadequate staffing and higher rates of patient adverse events. A review of 28 studies on the relationship between nurse-to-patient ratios and outcomes demonstrated that an increase of one registered nurse per patient per day was associated with decreased odds of hospital-acquired pneumonia, unplanned extubation, respiratory failure, and cardiac arrest in intensive care units; of failure to rescue among postoperative patients; and of shorter stays in the intensive care unit and hospital [11]. A later literature review on adverse outcomes in adult intensive care units showed that decreased staffing was associated with adverse outcomes (infection, postoperative complications, unplanned extubation) [122].
The relationship between inadequate staffing and nosocomial infection has received widespread attention, primarily because of the high rate of infection despite its preventability. In a study in neonatal intensive care units, inadequate staffing was associated with an increased risk of nosocomial infection in very-low-birth-weight infants [123]. In a study of adults, the rates of urinary tract and surgical site infections increased when a nurse's workload was increased by one patient [12]. Furthermore, the authors found a specific and significant association between nurse burnout and the rates of these infections. It was theorized that the cognitive detachment associated with burnout led to lapses in proper infection control procedures and estimated that if burnout was reduced by 30%, the annual cost savings would be nearly $28 million to more than $69 million from preventing these infections [12].
Mortality
Mortality is also influenced by nurses' patient volume and thus is linked to burnout. Several studies have shown that lower nurse workloads are associated with lower hospital mortality. In a landmark study, it was found that the addition of one patient per nurse was associated with a 7% increase in the likelihood of the patient dying within 30 days after admission [7]. Analysis of pooled data has indicated that, if a causal relationship exists between patient-nurse ratios and patient outcomes, decreasing the ratio from more than six patients per nurse to one or two patients per nurse would save an estimated 25 lives per 1,000 hospitalized patients and 15 lives per 1,000 surgical patients [11].
In addition, mortality rates can be improved in intensive care units, as shown by a 2017 retrospective analysis of nearly 900 patients in two separate units. In this study, the researchers focused on workload rather than number of patients. Workload was calculated using the Therapeutic Intervention Scoring System (TISS-76), which assigns points based on therapeutic, diagnostic, and nursing activities. Workloads scored as less than 40 per nurse produced a 95% probability that survival to hospital discharge was more likely to occur. Conversely, scores of more than 52 per nurse produced a more than 95% chance that death was more likely to occur [62].
In summary, increasing the availability of nurses by reducing the frequency of burnout can have a substantial effect on patient safety and the quality of care.
Identifying the signs of stress and burnout is important to preserve the overall health and well-being of nurses and their patients. For accurate identification, care should be taken to distinguish burnout from other conditions, such as stress, prolonged fatigue, compassion fatigue, and depression (Table 4)[6,18,27,28,36,38,41].
DIFFERENCES BETWEEN BURNOUT AND CLINICAL ENTITIES WITH SIMILAR PRESENTATION
| Other Clinical Entity | Burnout | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||
|
| ||||||||
|
| ||||||||
|
| ||||||||
|
|
Stress is a precursor to burnout, making it important to identify the signs and symptoms and address the issue. These signs and symptoms are multidimensional, with physical, psychological/psychiatric, and interpersonal/social manifestations [1,2,20]. As such, a multidisciplinary approach should be taken not only to confirm the presence of stress and/or burnout but also to rule out other illnesses or conditions. In addition to the traditional medical history and physical examination, a social and occupational history should be obtained in an effort to identify potential stress factors and possible social consequences [20]. An evaluation of the type, course, and frequency of symptoms can help distinguish them as signs of stress or burnout, and a drug history can help to identify potential substance abuse problems. The signs and symptoms of stress discussed here are similar across work settings, although, as mentioned, these symptoms may be exaggerated among healthcare workers due to the nature of their work [6,31].
Stress has been linked to many somatic conditions of varying degrees of severity. A 2022 report by the American Psychological Association showed that 76% of the American population reported stress-related physical symptoms. Headache was the leading physical symptom, reported by more than half of the respondents, and fatigue, upset stomach, and muscle tension were other top stress-related physical symptoms (Table 5) [2,32].
MOST COMMON PHYSICAL AND PSYCHOLOGICAL SYMPTOMS RELATED TO STRESS
| Symptoms | Frequency |
|---|---|
| Physical | |
| Headache | 59% |
| Fatigue | 57% |
| Change in sleep habits | 53% |
| Upset stomach | 34% |
| Muscle tension | 30% |
| Change in appetite | 33% |
| Psychological | |
| Feeling overwhelmed | 57% |
| Feeling depressed or sad | 57% |
| Nervousness/anxiety | 56% |
| Constant worrying | 53% |
| Difficulty making decisions | 31% |
| Forgetfulness | 21% |
Stress has also been found to contribute to poor health and coping behaviors, such as [42]:
Smoking
Overeating or eating an unhealthy diet
Not getting physical activity
Not taking medications as prescribed
Being overweight
Alcohol or drug misuse
Metabolic syndrome
These behaviors have been shown to increase the risk of developing chronic physical conditions such as hypertension, high cholesterol, uncontrolled glucose levels, inflammation, and arthritic conditions. Additionally, the risk of heart disease and stroke is raised, making it important to address factors causing stress [42].
Stress is also associated with a range of psychological symptoms. In the 2022 American Psychological Association survey, between 53% to 60% of respondents indicated that they felt overwhelmed, depressed, sad, nervous, anxious, and/or a constant state of worry during the past month. Other symptoms included difficulty making decisions and forgetfulness [2,32].
Interpersonal and social relationships may also be compromised by stress. Individuals experiencing acute stress and burnout may have a difficult time communicating with others in the work environment as well as with friends and family and may create emotional distance [18]. The cynicism that is characteristic of the syndrome may lead individuals to treat co-workers with suspicion and to have critical attitudes toward them [18]. Other effects include marital conflict and divorce, neglect of family and social obligations, and questioning of previously held spiritual beliefs [18].
Stress can cause many of the same physical, psychological, and interpersonal/social symptoms as burnout. However, stress is distinct from burnout in that it is usually precipitated by isolated or situational instances, whereas burnout is the result of chronic workplace stress [18,27].
Prolonged fatigue (also known as chronic fatigue) often overlaps with burnout, but the precipitating factor differs for each; fatigue is usually associated with health-related causes, whereas burnout is caused by job-related factors. In general, overall health and psychological distress are worse for individuals who have concurrent prolonged fatigue and burnout [28].
Compassion fatigue (also called vicarious or secondary trauma) occurs when an individual is exposed to the trauma or suffering of others, leading to emotional strain [38]. Compassion fatigue may be the result of one or multiple instances of witnessing (directly or indirectly) suffering or trauma. An individual with compassion fatigue is often able to still care and be involved, although emotional distress can vary from mild to severe; an individual with burnout may become indifferent, cynical, disengaged, and distant. The major difference between compassion fatigue and burnout is the involvement of trauma; burnout is not trauma-related, but instead is the result of chronic workplace stress [38].
Moral fatigue or moral injury is a relatively new term used to describe a feeling of powerlessness and deep moral injury that occurs when a person faces a moral dilemma and must act, witness, or consider violating their deeply held moral beliefs due to circumstances outside the individual's control. This term was used frequently during the COVID-19 pandemic to describe the challenges that healthcare workers faced when knowing what patients needed but being unable to provide optimal care due to systemic, societal, and organizational constraints beyond the healthcare workers' control. Moral injury is often caused by unforeseen and extreme circumstances and can lead to depression and contribute to burnout [36].
Depression and burnout may have a similar clinical presentation, and signs of depression can be associated with burnout. However, depression is related to factors within every domain of an individual's life and is not limited to specific factors in the work setting [27,41]. Depression is more likely among individuals who have had a recent loss or a personal or family history of depression, but burnout is more likely if symptoms are worse in the work environment and if the individual works long hours and has no time for outside interests.
The most important distinction between burnout and all of these entities is that only burnout is characterized by the collective features of emotional exhaustion, depersonalization, and lack of accomplishment, as measured on the MBI [6,19,27].
As noted, the criterion standard for measuring burnout is the Maslach Burnout Inventory, or MBI, a self-assessment tool first published in 1981 by Maslach and Jackson [19]. The MBI was originally developed for the human services industry (MBI-HSS), and since then, additional versions have been developed, including a general survey, an educator-specific survey, a medical personnel survey, and a survey for students [20,39]. In addition, the tool has been shown to be reliable, valid, and easy to administer and has been translated into several languages for use around the world. The MBI measures burnout as defined by the World Health Organization and the ICD-11 and is often used in conjunction with other assessments to evaluate the relationship between burnout and organizational policies, productivity, and social support [19,39].
The MBI addresses the three defining aspects of burnout syndrome with 22 statements in three subscales [18]:
Emotional exhaustion: Nine statements to measure feelings of being emotionally overextended and exhausted by one's work
Depersonalization: Five statements to measure an unfeeling and impersonal response to the recipients of one's services, care treatment, or instruction
Personal accomplishment: Eight statements to measure feelings of competence and successful achievement in one's work
Each statement in the MBI expresses a particular feeling or attitude; for example, one statement in the depersonalization subscale is "I've become more callous toward people since I took this job" [18]. For each statement, the respondent indicates how frequently he or she experiences that feeling by using a fully anchored scale ranging from 0 (never) to 6 (every day). Higher scores on the emotional exhaustion and depersonalization subscales indicate higher degrees of burnout. A lower score on the personal accomplishment subscale corresponds to a lower degree of burnout. A separate score is determined for each subscale, and a scoring key provides threshold scores to indicate a low, average, or high degree of burnout on each subscale.
The Areas of Worklife Survey (AWS) is an assessment tool that is designed to be used in conjunction with the MBI, and measures the likely cause of burnout in the workplace based on six key areas: workload, control, reward, community, fairness, and values [39]. The AWS uses individual assessment to assist in determining strengths and weaknesses in an organization or work environment in order to determine areas of improvement or adjustment. It should be noted, however, that the MBI and AWS were not meant to be used as an isolated diagnostic tool. Rather, Maslach notes, "When the MBI is used correctly, and in strategic combination with other relevant information, the findings can help leaders design effective ways to build engagement and establish healthier workplaces in which employees will thrive" [56].
Because the length of the MBI/AWS may limit its usefulness, researchers have explored the use of single-item measures from the instrument. Studies of healthcare professionals have shown that responses to one question in the emotional exhaustion subscale ("I feel burned out from my work") and one statement in the depersonalization subscale ("I have become more callous toward people since I took this job") correlate well with the results of the full MBI [50,51]. More recently, a nonproprietary single-item measure has been shown to be a reliable substitute for the single-item measure on the emotional exhaustion subscale of the MBI [52].
The use of psychological assessment tools in conjunction with the MBI can help professionals gain a better understanding of the sources of stress for individuals. The General Health Questionnaire, developed by Goldberg, is designed to measure common mental health problems (domains of depression, anxiety, somatic symptoms, and social withdrawal) and was developed as a measure to identify individuals who are likely to have or be at risk for the development of psychiatric disorders [53]. The General Health Questionnaire is frequently used in conjunction with the MBI to evaluate psychological morbidity and burnout, as the pathways to both are related [54].
The General Health Questionnaire has been translated into several languages and is available in a variety of versions, with a range of 12 to 60 items; the version with 28 items (GHQ-28) has been used most often in workplace settings [54]. A score of 0 to 3 is assigned to four possible responses ("not at all," "no more than usual," "rather more than usual," and "much more than usual") to such questions as:
Have you found everything getting on top of you?
Have you been getting scared or panicky for no good reason?
Have you been getting edgy and bad tempered?
Another exercise, the Burnout Risk Survey, was developed by Pfifferling, the director of the Center for Professional Well-Being, who has extensively studied stress in healthcare professionals (Table 6)[55]. This tool is designed to demonstrate the probability of mismatches between an individual and his or her work environment. A "yes" response to three or more of these items indicates a risk of burnout and a "yes" response to four or more items indicates a high risk.
BURNOUT RISK SURVEY
|
There are two primary approaches to preventing and/or coping with work-related stress and burnout. Given that the most significant factors in stress and burnout are related to the work environment, modifying the environment to eliminate the factors has the potential for the most success. However, it is often difficult to change organizational structure, which means individuals must make changes themselves.
The primary goal in any setting is to stop the burnout cycle early by preventing the accumulation of stress. When implemented appropriately, preventing burnout is easier and more cost-effective than resolving it once it has occurred; burnout that is addressed in later stages may take months or years to resolve fully [18,21]. Thus, stress management techniques and other interventions to ensure psychosocial well-being should be a priority for both individuals and institutions/organizations, with a goal of preventing stress and managing it during its early stages.
Attention to personal and professional lifestyle habits is essential for individuals to prevent and manage stress effectively. Self-care, time management, and strong interpersonal relationships are key elements for maintaining physical and psychosocial well-being (Table 7). In addition, care must be taken to protect an individual's professional lifestyle. Institutions and organizations have an obligation to maintain a healthy work environment for nurses and other healthcare professionals, not only to minimize the risk of burnout but also to ensure patient safety and high-quality patient care.
STRATEGIES FOR MANAGING STRESS AND AVOIDING BURNOUT
| Strategy Classification | Specific Strategies | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Personal lifestyle |
| |||||||||||||
| Professional lifestyle |
| |||||||||||||
| Organizational level |
|
The concept of self-care is one that is emphasized in every book or article on preventing job stress and burnout across occupations. Self-care warrants particular emphasis for nurses, as they have been trained to put the care of others ahead of themselves. It is important for nurses to recognize that self-care is not equivalent to selfishness; rather, self-care is essential for energizing, restoring, and maintaining the physical and emotional stamina to reduce fatigue and manage stress Research has shown that self-care strategies are associated with lower levels of burnout among nurses [18,119,124,125]. Self-care involves several universal lifestyle habits, such as proper diet, exercise, sleep, and regular health care. Maintaining a healthy lifestyle through these habits is vital to avoiding the physical effects of stress [2]. The need for appropriate sleep hygiene is the most essential element for nurses, as fatigue can have serious outcomes for both the nurse and patient. One study showed that 49% of nurses at an academic medical center averaged less than the recommended 7 hours of sleep per night, and the overall average nightly sleep time was only 6.6 hours. In addition, 27% used medication to help them sleep, and 13% used medications to stay awake. Symptoms consistent with chronic insomnia were identified in 31% of nurses sampled [33]. In 2020, the Well-Being Initiative, a collaborative effort by multiple nursing associations, published the Guide to Sleeping Better and Restoring Energy for nurses, after finding that 72.8% of nurses are suffering with sleep challenges (either excessive sleep or sleeplessness) [34]. There is widespread documentation that sleep disturbances are associated with a high risk of fatigue, which is linked to job satisfaction and burnout [117,119,124,125]. The following are recommended for proper sleep, nutrition, and exercise needed to alleviate stress and prevent burnout [34,119,125]:
Prioritize sleep
Maintain a regular sleep schedule on duty and off-duty days.
Try to get 7 to 9 hours in a 24-hour period.
Create a comfortable, cool, dark sleeping environment.
Wind down with gentle stretches, meditation, or progressive relaxation exercises.
Track sleep with wearable fitness tracker, phone, or sleep diary.
Restore energy
Use light to prompt wakefulness (open a window or turn on a light).
Take mental breaks to walk or practice mindfulness.
Eat healthy foods and do not skip meals.
Monitor caffeine (limit intake to 400 mg per day, avoid six hours prior to sleep, do not use as a substitute for sleep).
Take a 20-minute nap to restore energy or longer if needed to catch up on sleep.
If necessary, "bank" sleep ahead of time to prepare for longer periods of no sleep.
Participate in regular exercise—find activities that fit into your daily routine
Do not rely on medications to enhance alertness
Nurses should also seek outside activities that will help them disengage from their professional routine and provide enjoyment, such as yoga, music, art, reading, journaling, sports, meditation, hobbies, and volunteerism. Spirituality may help some individuals derive a sense of purpose or meaning in life and enhance coping skills, especially for nurses who care for dying patients [104].
Cognitive behavior training, physical relaxation (e.g., massage), and mental relaxation (e.g., mediation) may have limited benefit, according to a meta-analysis of interventions to reduce work-related stress in healthcare workers. The study demonstrated low-quality evidence that cognitive behavior training, with or without relaxation, reduced stress compared with no intervention, but only after more than one month of follow-up [104,106]. Similarly, physical relaxation was most effective one to six months after the intervention [106]. Little evidence supported mental relaxation as a way to reduce work-related stress after up to six months [106].
Managing stress requires a high level of self-awareness, which can also help prevent burnout [1,104]. An individual should recognize the specific factors that cause stress and how he or she deals with it. Many informal self-assessment exercises are available to help individuals determine their own level of work-related stress. For example, a simple exercise in the book Controlling Stress and Tension asks individuals to describe how frequently (almost always, often, seldom, or almost never) they experience the following signs or symptoms associated with burnout [107]:
Find yourself with insufficient time to do things you really enjoy?
Wish you had more support/assistance?
Lack sufficient time to complete your work most effectively?
Have difficulty falling asleep because you have too much on your mind?
Feel people simply expect too much of you?
Feel overwhelmed?
Find yourself becoming forgetful or indecisive because you have too much on your mind?
Consider yourself in a high-pressure situation?
Feel you have too much responsibility for one person?
Feel exhausted at the end of the day?
A score for the exercise is calculated by assigning 1 to 4 points for each answer (with 4 representing the "almost always" response); a total of 25 to 40 points indicates a high level of stress that could be psychologically or physically debilitating [107].
Staying in tune with the signs and symptoms of stress overload and burnout is a continuous process, and individuals should remain alert to their use of unhealthy and ineffective coping mechanisms, such as excessive use of caffeine, alcohol, or prescription medication; overeating or undereating; smoking; inactivity; or social withdrawal [6]. Such habits can be difficult to change, and individuals should focus on changing one behavior at a time and seek help from professional counseling if necessary [1].
Work/life satisfaction is a challenge for workers in all occupations and may be particularly difficult for nurses because of their work schedules. One way to help create better work/life satisfaction is to quantify the amount of time currently spent in each primary aspect of life—work, home, leisure, and vacation—and then determine priorities and assign preferred amounts of time for each aspect [108]. Creating such a time budget can help to prevent work life from overshadowing all other aspects of life, which can be harmful to self-esteem, self-identity, and overall well-being [22].
In a year-long study of the work/personal priorities of executive men and women from 10 multinational companies, 62% of the subjects were found to be work-centric (more apt to put work above personal life) and 32% were found to be dual-centric (more apt to set work and personal life as equal priorities) [105]. Dual-centric subjects reported stress less often than work-centric subjects (26% vs. 42%) [105]. In addition, dual-centric individuals felt more successful at work and had achieved higher professional levels. The dual-centric subjects used several strategies to maintain their priorities [105]:
Set strict boundaries between work and nonwork (did not bring work home)
Remained emotionally present in each aspect of life
Took time to "recover" after a particularly difficult time at work
Engaged in personal activities that require focus (such as sports, hobbies, or community volunteering)
Remained clear about priorities
Other ways to enhance work/life satisfaction is to maintain a balance of friends and colleagues, set boundaries with family and friends to avoid excess expectations, limit nonessential or nonproductive activities (e.g., checking personal email or social media, playing online games), communicate personal needs, and remember that you cannot please everyone—know how much you can handle [108].
Remaining "connected" to people is important in managing stress and preventing burnout. Nurses should strengthen relationships with family and friends and seek support from them as needed. Expanding the social network to involve community and volunteer activities can help increase self-esteem and provide focus and fulfillment outside of the profession [104,105].
Persistent symptoms of unresolved stress or burnout, such as sadness, anger, worthlessness, hopelessness, anxiety, sleep disturbances, or exhaustion, should prompt an individual to seek counseling, especially if these feelings interfere with interpersonal relationships or affect job performance [1]. Substance misuse or addictive behaviors also indicate the need for professional counseling. Nurses should be alert to the signs of burnout in not only themselves but also in their colleagues and should talk openly with those who exhibit severe symptoms [109].
Social support has been found to have a beneficial effect on workers' psychological well-being and professional productivity. Colleagues are in a unique position to understand each other's professional needs and stressors, and a supportive work environment protects against burnout [108,110]. Social support from colleagues is especially important during times of change and uncertainty in the work environment and can provide comfort, insight, rewards, humor, help, and escape [18,110]. In particularly stressful settings, informal social support gatherings can help nurses and other healthcare professionals deal with emotionally demanding events (such as the loss of a patient) [6,111].
Maslach defined working smarter as setting realistic goals, doing things differently (when possible), not taking things personally, and taking time away [18]. Setting realistic goals involves moving from abstract, idealistic goals to well-defined specific goals, which can help individuals gain a better sense of accomplishment. Varying work routines can help avoid feelings of being in a rut and provide a sense of better control. Taking things less personally involves objectifying negative interactions and situations to help decrease emotional involvement, thereby reducing stress.
Working smarter also means taking time away and organizing time more effectively. A typical response to work overload is to work longer or harder to help make the situation "get better" [18]. However, this approach will only exacerbate stress and burnout, not relieve it. The need to take some time away from work must be especially emphasized to nurses, most of whom do not routinely take breaks or do not take effective breaks. One study showed that appropriate breaks were least likely among nurses working the longest hours, and that approximately 60% of nurses are usually not completely free of patient care responsibilities during breaks for rest or meals [93]. Rest breaks are particularly important for nurses working the night shift, to relieve symptoms of fatigue, which can be detrimental to both nurses' well-being and patient safety [6,97]. Taking some time away from work—even if only a few minutes at a time—to stretch, take a walk, make a personal phone call, read, meditate, or just sit and relax can help nurses "recharge" and will improve performance and increase productivity more effectively than working continuously [1]. Facilities must help ensure that nurses take breaks and meals appropriately, as will be discussed later. Other time management techniques include scheduling a block of unplugged, uninterrupted time (no phones, pagers, or e-mails) to complete paperwork more efficiently, creating "to do" lists to maintain control over tasks, and increasing organizational skills [1,104].
Engaging in lifelong learning is another way to help combat burnout. Continuing education can help infuse energy into nurses and help them renew their passion for the profession. Studies have found that continuing career development through high-quality education was correlated with greater job satisfaction and job retention among nurses [35,92]. The COVID-19 Impact Assessment Survey, which included more than 22,000 responses from nurses, asked what would better prepare nurses for future health crises and/or pandemics, and nurses indicated that continuing education in disaster preparedness (50%) and in emergency and critical care (44%) would be helpful [115]. Becoming better educated can also help nurses advance in their career and become involved in decision making that affects nurses' job satisfaction.
Advocating for changes in the work environment or in the healthcare profession overall can help nurses increase a sense of control [18]. Assessing the potential for burnout and taking steps toward prevention is a process that can begin with one person who assumes a leadership role in a group effort [18]. The individual leader engages a group of colleagues to work with organizational leaders to heighten awareness of common stress factors within the organization and to address issues that compromise patient safety and quality of care.
Becoming an advocate means becoming familiar with policies, laws, and regulations related to nursing practice. Yet, many nurses are not aware of their facility's policies regarding breaks or limits for work hours or overtime [78]. Nurses should gain a better understanding of these policies, as well as federal and state regulations and professional statements. For example, the ANA has developed a position statement on nurse fatigue and resources on staffing plans and mandatory overtime [84,85,124]. Nurse specialty organizations have also developed recommendations to address fatigue [86,87,125]. The Emergency Nurses Association lists several evidence-based recommendations concerning fatigue for staff nurses; among these recommendations are the following [125]:
Speak up when fatigue is a concern, before patient safety is compromised
Evaluate the decision to work if you have had enough rest
Tell your nurse managers when you have worked extended shifts
Limit the number of hours you agree to work overtime
Identify and work the shift that fits your circadian rhythm the best
Establish support networks
Exchange solutions with colleagues on ways to cope with the problems of shift work
Help co-workers by watching for signs of drowsiness
Integrate innovative strategies that support adequate rest and time away from the workplace between worked shifts
In addition to helping manage fatigue, these recommendations can help nurses serve as a role model for others, as well as feel empowered and in control of their practice, two other factors that help to prevent burnout.
Nurses learn to control their emotions to maintain a professional demeanor, but they are not immune to grief. A healthy response to the stresses associated with loss is important for avoiding burnout. As noted, burnout levels were higher among nurses who masked their emotions [75]. Instead of masking emotions, nurses must learn how to grieve well [111]. Grieving well involves accepting the reality of the loss, experiencing the pain of grief, adjusting to the absence, and moving on with life. Nurses can draw strength from colleagues and others by communicating sadness, frustration, and grief and can find solace in discussing what they were able to achieve with their dying patients, such as the ability to help manage pain and other symptoms [111].
Maintaining positive relationships with colleagues, physicians, and patients is often challenging and requires strong communication skills. Skilled communication is an essential standard in nursing and is an integral aspect of a healthy work environment. Nurses can decrease their vulnerability to stress by taking advantage of programs that strengthen their communication skills and help them to become more adept at handling difficult situations.
Nurses should also learn how to better communicate with their patients across language and culture. They should ask their patients what language they prefer for their medical care information and should seek the use of professional interpreters as much as possible [98]. The use of professional interpreters has been associated with improvements in communication (errors and comprehension), clinical outcomes, and patient satisfaction with care [99,100]. In addition, a systematic review of the literature has shown that the use of professional interpreters provides better clinical care than the use of ad hoc interpreters (untrained staff members, family members, friends, strangers in the hospital), with the former improving the quality of care for patients with limited English language skills to a level equal to that for patients with no language barriers [100].
Among the best ways for an institution to prevent burnout is to promote engagement by implementing strategies that enhance energy, involvement, and efficacy. Promoting engagement involves increasing positive aspects as well as reducing negative ones. As a first step, Maslach suggests transforming the six mismatches to fit a sense of engagement [21,39,45]:
Sustainable workload
Feelings of choice and control
Recognition and reward
A sense of community
Fairness, respect, and justice
Meaningful and valued work
Another integral step in preventing burnout is to survey staff about important aspects of the organizational culture. As noted, Maslach developed a staff survey that incorporates the MBI with questions related to the six mismatches that lead to burnout (work overload, lack of control, insufficient reward, absence of community, lack of fairness, and conflict in values) and questions about management structures and processes (such as direct supervision and distant management), communication networks, health and safety concerns, and performance appraisal. Questions customized for a specific setting may also be helpful. The AWS can also be used in conjunction with the MBI to measure the likely cause of burnout in the workplace. After the survey data have been collected, the responses are analyzed to identify the issues that should be addressed [21,39].
Organizations and institutions can help protect nurses from burnout by creating an organizational culture of trust, support, and open communication and fostering a healthy work environment [6,18]. Creating a healthy work environment has become a priority for enhancing nurse job satisfaction and retention and improving patient safety and satisfaction. The American Association of Critical-Care Nurses (AACN) developed standards for a healthy work environment, noting that such an environment is necessary for clinical excellence and good patient outcomes. Six components were noted to be essential for establishing and sustaining a healthy work environment [101]:
Appropriate staffing
Meaningful recognition
True collaboration
Skilled communication
Effective decision making
Authentic leadership
The AACN has also developed an assessment tool that institutions can use to evaluate their environment against the AACN standards.
Evidence that a healthy work environment helps improve job satisfaction is emerging. Reports from hospitals that have implemented changes to create a healthy work environment have shown that the changes led to a more engaged nursing staff, greater job satisfaction, low turnover, and high retention. The changes have included the following [6,102,103]:
Creating a culture of uninterrupted meal breaks
Developing strategies to manage patient volumes
Reorganizing schedules to reduce stress
Creating a serenity area
Enhancing nurse-physician relationships
Establishing a hospital wellness program
Offering regular fun activities
Implementing training and education initiatives
Developing reward and recognition programs
Implementing a zero-tolerance policy for discriminatory behavior
Normalizing help-seeking for mental health issues and/or substance use care
Implementing strategies to reduce administrative burdens
Nurses' work schedules and appropriate staffing should be the highest priority for reducing burnout. Defining "appropriate staffing" has been subject to debate, however. Some have argued for specific patient-nurse ratios, while others have advocated for hospitals to establish staffing committees, with nurses as members, charged with creating staffing plans that reflect the specific needs of the institution [84]. The ANA has identified enforceable ratios as an essential approach to achieving appropriate nurse staffing through their support of theNurse Staffing Standards for Hospital Patient Safety and Quality Care Act of 2023. This act calls for establishing minimum nurse-to-patient staffing requirements at the national level and will help examine best practices for nurse staffing and provide whistleblower protections for nurses who choose to advocate for the safety of their patients [84,91]. This bill has been introduced in Congress several times since 2007, but no action has been taken; however, the need to protect nurses and patients is greater than ever [91]. As of 2022, 14 states have passed laws or regulations addressing nurse staffing: California, Connecticut, Illinois, Massachusetts, Minnesota, Nevada, New Jersey, New York, Ohio, Oregon, Rhode Island, Texas, Vermont, and Washington [46,84]. Of these, seven states have laws or regulations requiring staffing policies that are developed by committees. Only California stipulates in law and regulations a required minimum nurse-to-patient ratio be maintained at all times, with that ratio being dependent on the unit of care. Massachusetts is the only other state to have a specific staff ratio legislation enacted; however, that law applies to the intensive care unit only [84]. Hospital administrators and nursing leaders should be familiar with staffing ratios mandated in their state.
With the unexpected surge of hospitalized patients due to COVID-19, the nurse-to-patient ratio soared in most states. During the height of the pandemic, California hospitals were able to apply for waivers to bypass safe staffing ratios, placing nurse staff at higher risk for burnout and creating an increasingly unsafe environment. All waivers granted in California expired in February 2021, but the uncertainty surrounding the pandemic calls for a renewed discussion of The Nurse Staffing Standards for Hospital Patient Safety and Quality Care Act and other legislation [60,84]. In addition, in the One-Year COVID-19 Impact Assessment Survey, released in 2021, the leading response (74% of participants) when asked what would help prepare for future crises and/or pandemics was consistent and better executive national health policies and public intervention plans, followed by effective leadership communication (67%), and increased staffing (66%) [115].
Institutions should also implement staffing policies that address nurse fatigue. The ANA position statement on nurse fatigue notes the following evidence-based recommendations [124]:
Employers should include nurse input when designing work schedules and implement a "regular and predictable schedule" that allows nurses to plan for work and personal obligations.
Nurses should work no more than 40 hours in a seven-day period and limit work shifts to 12 hours in a 24-hour period, including on-call hours worked.
Employers should stop using mandatory overtime as a "staffing solution."
Employers should encourage "frequent, uninterrupted rest breaks during work shifts."
Employers should adopt official policy that gives RNs the "right to accept or reject a work assignment" to prevent risks from fatigue. The policy should be clear that rejecting an assignment under these conditions is not patient abandonment and that RNs will not be retaliated against or face negative consequences for rejecting such an assignment.
Employers should encourage nurses to be proactive about managing their health and rest, including getting seven to nine hours of sleep per day; managing stress effectively; developing healthy nutrition and exercise habits; and using naps according to employer policy.
These recommendations echo those developed by the Joint Commission and specialty nurse associations [85,86,87,125,117]. As of March 2024, 18 states had enacted laws or regulations restricting mandatory overtime for nurses [85].
Institutions should also consider implementing innovative measures to ensure that nurses take breaks and meal periods. Some interventions that have been successful are encouraging going outside for breaks, setting longer meal periods, adding shorter shifts to cover meal periods, a buddy system for breaks, tuning off cell phones and pagers during breaks, nurse managers' coverage of breaks, and monitoring and documentation of breaks to ensure they are taken [88,102].
Administration and nursing managers can help increase job satisfaction and nurse retention by implementing strategies to enhance nurse autonomy and control. These strategies should be based on setting clear expectations and supporting measures to increase the knowledge and expertise of nurses [89]. Nurses should be involved in participative decision making, especially as it relates to their practice. Fostering independence and autonomy can be accomplished through clear and open communication, collaboration, seeking opinions from a nursing team, providing decision-making opportunities, and encouraging professional development through education and training [89].
Given the link between ineffective management and leadership and job dissatisfaction and burnout, institutions should ensure that nursing leadership is strong and supportive.
Nurse managers should be accessible to staff, provide a supportive environment, and work to foster better relationships among nurse peers and between nurses and physicians. Nurse leaders should also empower nurses by providing them with information, resources, and opportunities. These factors have been shown to reduce work-related stress and burnout among nurses [89].
One challenge for nurse managers is that they themselves are often burned out or fatigued. Nurse managers should ensure that they practice self-care, set realistic goals, be clear about boundaries, and schedule time off [71,104,125].
The importance of positive interpersonal relationships with peers and physicians to both nurses' job satisfaction and patient outcomes requires a commitment from administrators and nursing leadership to foster better collaboration and communication within the working environment. Enhancing peer support systems and group cohesion has been identified as an important aspect of a healthy work environment [90]. And, as noted earlier, enhancing communication and collaboration between nurses and physicians is an essential element of a healthy work environment [65,101,102]. Thus, institutions should offer training programs that focus on effective communication between nurses and physicians and forums that allow healthcare professionals to interact outside of the patient's bedside [126]. Simulation training in decision making, interdisciplinary rounds, patient care seminars, continuing education lectures, and hospital committees can provide opportunities for nurses and physicians to collaborate on projects and gain a better understanding and respect for each other. Developing mutual respect early in the career may be of value; medical students who were required (as part of their curriculum) to shadow a nurse for one day gained a better appreciation of the nurse's role [6,47].
Nurses should be encouraged to participate in workshops that address challenges such as overcoming cultural and language barriers, responding to emotions, and dealing with angry patients and their families. Training has been advocated primarily for nurses in oncology and has been shown to improve some areas of communication skills, to help alleviate stress, and to improve the coping skills of patients with cancer [6,121].
Another priority is to make available programs designed to help nurses manage the emotional demands of the job and enhance their psychosocial well-being. However, developing effective programs can be a challenge. A meta-analysis of staff-support interventions showed that stress management training offers some benefit in reducing work-related stress and increasing job satisfaction among health workers, but the benefit is not maintained over the long term. High-intensity stress management training interventions did have a beneficial effect in terms of reducing burnout. More research is needed to determine if longer term interventions or refresher sessions will help improve the effectiveness of these programs [120]. Nurses in all settings can benefit from programs designed to enhance coping techniques, to facilitate work-related grief and bereavement [72].
Nurse C and Nurse M had been best friends growing up, and they shared a lifelong dream of becoming nurses. Various family and other commitments separated them after college, and they began their nursing careers at different hospitals in different states. As new graduates on medical-surgical units, both were energetic and enthusiastic nurses, committed to excellence in caring for their patients.
Over the course of the first year, the hospital where Nurse C worked dealt with budget cuts and resources began to decline. Staffing on Nurse C's unit decreased, and daily patient load went from four patients to seven patients. She struggled to keep up with the increasing workload and found herself unable to spend as much time as she wanted with her patients. The hospital instituted mandatory overtime to help overcome the staffing shortage, and Nurse C soon began working a few hours beyond her usual 12-hour shifts and often worked six or seven days in a row. She was tired all the time and frequently found it difficult to focus, especially near the end of her shift. Her personal life was affected; she called her family less often and never seemed to have time for her friends.
Nurse C has many of the personal risk factors for burnout: she is young, early in her career, single, and highly educated. Her unsupportive work environment, however, is the key, with work overload leading her to become frustrated and disappointed with her job. Nurse C is among the approximately 65% to 80% of nurses who work 12 hours or more per day. As a result, she is experiencing the first stage of burnout, characterized by mental and physical exhaustion. Unless she addresses her stress and job dissatisfaction, the subsequent stages of burnout will evolve.
Nurse C did make time for a phone call from her friend Nurse M and couldn't believe how happy Nurse M was in her job. Nurse M listened as Nurse C described all her dissatisfactions with her work. Nurse M sympathized with her situation and talked enthusiastically about her own recent transfer to the medical intensive care unit. She urged Nurse C to transfer to the intensive care unit at her hospital because of the professional challenges and lower patient load. "You'll really feel like you're making a difference," Nurse M told her. Encouraged, Nurse C submitted a request for a transfer to the medical intensive care unit.
Nurse C gained renewed interest and energy during her orientation and training in the intensive care unit. She enjoyed the technical challenges of the more complex patient care, and she again looked forward to work. However, after she was fully oriented to the unit, her patient load increased and she again found herself working long hours and overtime. She went home every day with a headache and backache, she never felt fully rested, and she experienced extreme mood swings. She again withdrew from family and friends and found herself frequently overeating. She also began to have a glass or two of wine every night as a way to cope with her stress. The "last straw" for Nurse C was a medication error she made. No substantial harm came to the patient, but the patient's physician yelled at Nurse C and several other nurses in the unit. As a result, Nurse C felt like a professional failure and questioned her decision to become a nurse. She distanced herself even further from her colleagues, her family, and her friends.
Changing the work setting is a frequent response to job dissatisfaction. However, different environments can have the same inherent stress factors, which means that the potential for burnout can continue. Within nursing environments, work overload brought on by inadequate staffing is the most common source of stress and burnout. High levels of fatigue brought on by work schedule factors have been associated with an increased risk of errors, and these errors frequently cause moral distress for nurses. In addition, difficulties in nurse-physician relationships also affect nurses' morale, and job satisfaction decreases when nurse-physician collaboration is poor. Nurse C is moving through the next stages of burnout, marked by indifference and feelings of failure as a professional.
Nurse M surprised Nurse C with a visit and was distressed about what had happened to Nurse C. Her friend had dark circles under her eyes, was overweight, and lacked her usual passion for life. Nurse M convinced Nurse C to tell her about her situation at work. When Nurse M heard about Nurse C's work schedule and patient load, she became angry at the situation and told Nurse C that she needed to take better care of herself and become an advocate for change at her hospital. Nurse M explained that not all hospitals are the same, and she described her own positive work environment. In her unit, the nurses have a weekly get-together during which they talk about their most challenging patients and how they cope with loss. The Human Resources department sends out flyers about stress management programs, and the supervisors rearrange schedules to allow nurses to attend. Although there can be heavy workloads, the head nurse works with the staff as she develops the schedule so nurses have some say in the shifts and the number of days they work. The head nurse also anticipates needs and requests per diem nurses to help keep the patient load low.
Nurse C was surprised at the differences between her hospital and Nurse M's hospital, but she expressed doubt that she could change how her hospital functioned. Nurse M acknowledged that it is difficult to change organizations but she encouraged her to talk with other nurses about the situation and to band together to approach administration and request changes in scheduling and to emphasize the detrimental effect of heavy patient load on patient outcomes and quality of care. Nurse M noted that, equally as important as working for change in her hospital, Nurse C must make changes in her personal and professional lifestyles to help her better manage stress and avoid burning out completely. Nurse M told her about the importance of finding healthier ways to cope with stress, evaluating her work/life satisfaction, seeking support from friends and family, working "smarter," and engaging in nonwork activities. Nurse M also reminded Nurse C about how excited the two of them had always been about becoming nurses.
Because it is difficult to change organizational structure, individuals must make changes in themselves to avoid stress and burnout. Attention to personal and professional lifestyle habits are integral steps in preventing and managing stress effectively. Self-care, time management, and strong interpersonal relationships are key elements for maintaining physical and psychosocial well-being.
Maintaining a healthy lifestyle, with proper diet, exercise, and sleep, is vital to avoiding the physical effects of stress, as is seeking activities that help to disengage individuals from their professional routine and provide enjoyment. Self-reflection as a way to remind oneself why he or she entered the healthcare profession and remaining "connected" to people are also important in managing stress and preventing burnout. Adequate time away from work is essential for maintaining positive work/life satisfaction and has been the most common suggestion about how to avoid stress and burnout.
Working smarter refers to taking frequent "mini-breaks" to escape work stresses, varying daily work routines, and setting realistic goals. Nurses can also increase their sense of control by advocating for changes in the work environment and for adherence to institution policies, state and federal laws and regulations, and nursing association statements and principles.
Over the next few months, Nurse C starts to pay better attention to her health by eating a balanced diet and finding time for regular exercise, including a twice-weekly yoga class. She starts an informal support group with her peers on her unit, and the number of participants increases as the sessions become more popular. She also visits with the Human Resources staff to ask about workshops in stress management techniques. In addition, Nurse C leads a small group of her peers in approaching their nursing supervisor to discuss their concerns about the quality of patient care and staffing. With time, Nurse C has a renewed sense of purpose at work and has become involved in a multidisciplinary committee that is addressing quality of care. She also has become more active in her personal life, spending more time with friends and family and volunteering as a coach for a youth soccer team. She has scheduled her first vacation in two years, planning a 10-day cruise with her best friend, Nurse M.
Burnout is a syndrome of emotional exhaustion, depersonalization, and reduced personal accomplishment. Levels of burnout are high among healthcare professionals, and the effects of burnout have serious consequences in the nursing profession. Combined with the unique experiences of the COVID-19 pandemic, nurses are at an unprecedented risk of psychological and physical effects that could lead to burnout. In addition to the detrimental physical, psychological, and interpersonal/social effects, high levels of burnout among nurses have led to an ongoing nursing shortage that poses a threat to patient safety and quality of patient care.
At the root of burnout is job dissatisfaction. If left unaddressed, this dissatisfaction can lead to prolonged stress and subsequent burnout. Several sources of job dissatisfaction among nurses have been identified, including staffing inadequacy, work schedule, lack of involvement in decision making, lack of support from nursing leadership and administration, interpersonal conflict (interactions with physicians and peers), and inadequate pay. These sources of dissatisfaction can be correlated with four of the mismatches (work overload, lack of control, insufficient reward, and absence of community) identified by Maslach, the foremost authority on burnout. One of the most often cited sources of dissatisfaction is inadequate staffing, which creates a cycle of increased job dissatisfaction, burnout, and turnover. The rate of burnout has been found to increase 23% for every additional patient per nurse, and patient-nurse volumes have also been related to an increased frequency of adverse events, nursing errors, and higher patient mortality.
Because studies have shown that factors within the work environment are the greatest predictors of job dissatisfaction and stress, it is incumbent on nursing management and administration, as well as individual nurses themselves, to address issues of job dissatisfaction to prevent burnout early in the cycle. Nurses must maintain personal and professional lifestyle habits that will keep them healthy, engaged in pursuits other than their profession, and connected with family, friends, and colleagues. In addition, nurses should seek supportive relationships with colleagues and ensure a work/life balance that fits their overall priorities.
Institutions and organizations should focus on creating a healthy work environment in which nurses feel supported by their peers, their supervisors, and physicians. In addition, organizations should make available stress management workshops and other educational programs that target nurses' psychosocial well-being and interpersonal skills. Above all, organizations must ensure that safe nurse staffing patterns are in place.
1. American Psychological Association. Coping with Stress at Work. Available at https://www.apa.org/topics/healthy-workplaces/work-stress. Last accessed March 1, 2024.
2. American Institute of Stress. What is Stress? Available at https://www.stress.org/daily-life. Last accessed March 1, 2024.
3. Bureau of Labor Statistics, U.S. Department of Labor. Occupational Outlook Handbook, Registered Nurses. Available at https://www.bls.gov/ooh/healthcare/registered-nurses.htm. Last accessed March 1, 2024.
4. American Psychological Association. 2023 Work in America Study: Workplaces as Engines of Psychological Health and Well-Being. Available at https://www.apa.org/pubs/reports/work-in-america/2023-workplace-health-well-being. Last accessed March 1, 2024.
5. U.S. Department of Health and Human Services. The U.S. Surgeon General's Framework for Workplace Mental Health and Well-Being. Available at https://www.hhs.gov/sites/default/files/workplace-mental-health-well-being.pdf. Last accessed March 1, 2024.
6. U.S. Department of Health and Human Services. Addressing Health Worker Burnout: The U.S. Surgeon General's Advisory on Building a Thriving Health Workforce. Available at https://www.hhs.gov/sites/default/files/health-worker-wellbeing-advisory.pdf. Last accessed March 1, 2024.
7. Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288(16):1987-1993.
9. Kelly LA, Gee PM, Butler RJ. Impact of nurse burnout on organizational and position turnover. Nursing Outlook. 2021;69(1):96-102.
10. Juraschek SP, Zhang X, Ranganathan V, Lin VW. Republished: United States registered nurse workforce report card and shortage forecast. Am J Med Qual. 2019;34(5):473-481.
11. Kane RL, Shamliyan T, Mueller C, Duval S, Wilt TJ. Nursing Staffing and Quality of Patient Care. Evidence Report/Technology Assessment No. 151. Rockville, MD: Agency for Healthcare Research and Quality; 2007.
12. Cimiotti JP, Aiken LH, Sloane DM, Wu ES. Nurse staffing, burnout, and health care-associated infection. Am J Infect Control. 2012;40(6):486-490.
13. Mayo Clinic. Job Burnout: How to Spot it and Take Action. Available at https://www.mayoclinic.org/healthy-lifestyle/adult-health/ in-depth/burnout/art-20046642. Last accessed March 1, 2024.
14. Sinsky CA, Trockel M, Carlasare LE, et al. Politicization of medical care, burnout, and professionally conflicting emotions among physicians during COVID-19. Mayo Clin Proc. 2023;98(11):1613-1628.
15. Felton JS. Burnout as a clinical entity: its importance in health care workers. Occup Med (Lond). 1998;48(4):237-250.
17. Edelwich J, Brodsky A. Burn-out: Stages of Disillusionment in the Helping Professions. New York, NY: Springer; 1980.
19. Maslach C, Jackson SE. Maslach Burnout Inventory. Palo Alto, CA: Consulting Psychologists Press; 1981.
20. Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory. 3rd ed. Palo Alto, CA: Consulting Psychologists Press; 1996.
21. Maslach C, Leiter MP. The Truth about Burnout: How Organizations Cause Personal Stress and What to Do About it. San Francisco, CA: Jossey-Bass; 1997.
22. Weber A, Jaekel-Reinhard A. Burnout syndrome: a disease of modern societies? Occup Med (Lond). 2000;50(7):512-517.
23. U.S. Department of Health and Human Services. Job Satisfaction Among Registered Nurses: Pre-COVID. Available at https://bhw.hrsa.gov/data-research/review-health-workforce-research/national-sample-survey-registered-nurses. Last accessed March 1, 2024.
24. Purvanova RK, Muros JP. Gender differences in burnout: a meta-analysis. J Vocat Behav. 2010;77(2):168-185.
25. Ahola K, Honkonen T, Isometsä E, et al. Burnout in the general population: results from the Finnish Health 2000 Study. Soc Psychiatry Psychiatr Epidemiol. 2006;41(1):11-17.
26. Centers for Medicare and Medicaid Services. ICD-10 Resources. Available at https://www.cms.gov/medicare/coding-billing/icd-10-codes/icd-10-resources. Last accessed March 1, 2024.
27. World Health Organization. Burn-out an "Occupational Phenomenon:" International Classification of Diseases. Available at https://www.who.int/news/item/28-05-2019-burn-out-an-occupational-phenomenon-international-classification-of-diseases. Last accessed March 1, 2024.
28. Ross A, Geiger-Brown J, Yang L, et al. Acute and chronic fatigue in nurses providing direct patient care and in non-direct care roles: a cross-sectional analysis. Nurs Health Sci. 2021;23(3):628-638.
29. Thomas-Hawkins C, Flynn L, Zha P, Ando. The effects of race and workplace racism on nurses' intent to leave the job: the mediating roles of job dissatisfaction and emotional distress. Nurs Outlook. 2022;70(4):590-600.
30. American Nursing Association. Survey Shows Substantial Racism in Nursing. Available at https://www.nursingworld.org/practice-policy/workforce/racism-in-nursing/national-commission-to-address-racism-in-nursing/survey-shows-substantial-racism-in-nursing. Last accessed March 1, 2024.
31. American Psychological Association. Stress in America 2023: A Nation Recovering from Collective Trauma. Available at https:// www.apa.org/news/press/releases/stress/2023/collective-trauma-recovery. Last accessed March 1, 2024.
32. American Psychological Association. Stress in America 2022: Concerned for the Future, Beset by Inflation. Available at https:// www.apa.org/news/press/releases/stress/2022/concerned-future-inflation. Last accessed March 1, 2024.
33. American Academy of Sleep Science. Nurses Have an Increased Risk of Sleep Disorders and Sleep Deprivation. Available at https://aasm.org/sleep-deprivation-disorders-nurses. Last accessed March 1, 2024.
34. American Psychiatric Nurses Association. Guide to Sleeping Better and Restoring Energy. Available at https://www.apna.org/resources/well-being-initiative/. Last accessed March 1, 2024.
35. Shiri R, El-Metwally A, Sallinen M, et al. The role of continuing professional training or development in maintaining current employment: a systematic review. Healthcare (Basel). 2023;11(21):2900.
36. Vaughn N. Nursing Compassion Fatigue and Burnout vs. Moral Injury. Available at https://www.nurse.com/blog/nursing-compassion-fatigue-and-burnout-vs-moral-injury. Last accessed March 1, 2024.
37. AMN Healthcare. 2023 AMN Healthcare Survey of Registered Nurses: The Pandemic's Consequences. Available at https://www.amnhealthcare.com/amn-insights/nursing/surveys/2023. Last accessed March 1, 2024.
38. The American Institute of Stress. Definitions. Available at https://www.stress.org/military/for-practitionersleaders/compassion-fatigue. Last accessed March 1, 2024.
39. Maslach C, Jackson SE, Leiter MP, Schaufeli WB, Schwab RL. Maslach Burnout Inventory (MBI). Available at https://www.mindgarden.com/117-maslach-burnout-inventory-mbi. Last accessed March 1, 2024.
40. Gómez-Urquiza JL, Vargas C, De la Fuente EI, et al. Age as a risk factor for burnout syndrome in nursing professionals: a meta-analytic study. Res Nurs Health. 2017;40(2):99-110.
41. Ahola K, Hakanen J, Perhoniemi R, Mutanen P. Relationship between burnout and depressive symptoms: a study using the person-centered approach. Burnout Res. 2014;1(1):29-37.
42. American Heart Association. Stress and Heart Health. Available at https://www.heart.org/en/healthy-living/healthy-lifestyle/stress-management/stress-and-heart-health. Last accessed March 1, 2024.
43. Smiley RA, Allgeyer RL, Shobo Y, et al. The 2022 National Nursing Workforce Survey. J Nurs Reg. 2023;14(1 Suppl 2):S1-S90.
44. Hassard J, Teoh KR, Visockaite G, Dewe P, Cox T. The cost of work-related stress to society: a systematic review. J Occup Health Psychol. 2018;23(1):1.
45. U.S. Department of Health and Human Services. 2022 National Sample Survey of Registered Nurses. Available at https://bhw.hrsa.gov/data-research/access-data-tools/national-sample-survey-registered-nurses. Last accessed March 1, 2024.
46. Trusted Nurse Staffing. 2024 Nursing Ratios: Which States Have Nurse-Patient Ratios and Why They're Important. Available at https://www.trustednursestaffing.com/nurse-patient-ratios-by-state. Last accessed March 1, 2024.
47. Alder S. The HIPAA Journal: Communication between Doctors and Nurses. Available at https://www.hipaajournal.com/communication-between-doctors-and-nurses. Last accessed March 1, 2024.
48. American Nurses Foundation. Pulse on the Nation's Nurses Survey Series: COVID-19 Two-Year Impact Assessment Survey Younger Nurses Disproportionally Impacted by Pandemic Compared to Older Nurses; Intent to Leave and Staff Shortages Reach Critical Levels. Available at https://www.nursingworld.org/practice-policy/work-environment/health-safety/disaster-preparedness/coronavirus/what-you-need-to-know/covid-19-impact-assessment-survey---the-second-year. Last accessed March 1, 2024.
49. AMN Healthcare. 2019 Survey of Registered Nurses. Available at https://www.njccn.org/wp-content/uploads/2020/04/AMN-2019-RN-Survey-Report.pdf. Last accessed March 1, 2024.
50. West CP, Dyrbye LN, Sloane JA, Shanafelt TD. Single item measures of emotional exhaustion and depersonalization are useful for assessing burnout in medical professionals. J Gen Intern Med. 2009;24(12):1318-1321.
51. West CP, Dyrbye LN, Satele DV, Sloan JA, Shanafelt TD. Concurrent validity of single-item measures of emotional exhaustion and depersonalization in burnout assessment. J Gen Intern Med. 2012;27(11):1445-1452.
52. Dolan ED, Mohr D, Lempa M, et al. Using a single item to measure burnout in primary care setting: a psychometric evaluation.J Gen Intern Med. 2015;30(5):582-587.
55. Pfifferling JH. Burnout Risk Appraisal. Available at http://www.vhcf.org/wp-content/uploads/2010/11/Burnout-Risk-Survey.doc. Last accessed March 1, 2024.
56. Maslach C, Leiter MP. How to Measure Burnout Accurately and Ethically. Available at https://hbr.org/2021/03/how-to-measure-burnout-accurately-and-ethically. Last accessed March 1, 2024.
57. American Nurses Foundation. The American Nurses Foundation Says Action is Still Needed to Address Serious Nursing Workforce Challenges. Available at https://www.nursingworld.org/news/news-releases/2023/the-american-nurses-foundation-says-action-is-still-needed-to-address-serious-nursing-workforce-challenges. Last accessed March 1, 2024.
58. Oshodi TO, Bruneau B, Crockett R, et al. The nursing work environment and quality of care: content analysis of comments made by registered nurses responding to the Essentials of Magnetism II scale. Nurs Open. 2019;6(3):878-888.
59. Dempsey C, Reilly BA. Nurse Engagement: What Are the Contributing Factors for Success? Available at https://ojin.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/OJIN/TableofContents/Vol-21-2016/No1-Jan-2016/Nurse-Engagement-Contributing-Factors-for-Success.html. Last accessed March 1, 2024.
60. Dembosky A. California is Overriding its Limits on Nurse Workloads as COVID Surges. Available at https://www.healthleadersmedia.com/nursing/california-overriding-its-limits-nurse-workloads-covid-surges. Last accessed March 1, 2024.
61. Jun J, Ojemeni MM, Kalamani R, et al. Relationship between nurse burnout, patient and organizational outcomes: systematic review. Int J Nur Stud. 2021;119:103933.
62. Lee A, Cheung YSL, Joynt GM, Leung CCH, Wong W-T, Gomersall CD. Are high nurse workload/staffing ratios associated with decreased survival in critically ill patients? A cohort study. Ann Intensive Care. 2017;7:46.
63. Ehsani SR, Cheraghi MA, Nejati A, Salari A, Esmaeilpoor AH, Nejad EM. Medication errors of nurses in the emergency department.J Med Ethics Hist Med. 2013;6:11.
64. Bogaert PV, Clarke S, Roelant E, et al. Impacts of unit-level nurse practice environment and burnout on nurse-reported outcomes: a multilevel modelling approach. J Clin Nurs. 2010;19:1664-1674.
65. Sutherland S. Survey Finds Nearly Half of Nurses Considering Leaving the Profession. Available at https://www.rnnetwork.com/blog/in-the-news/rnnetwork-nurse-survey. Last accessed March 1, 2024.
66. Stimpfel AW, Aiken LH. Hospital staff nurses' shift length associated with safety and quality of care. J Nurs Care Qual. 2013;28(2):122-129.
67. Neff DF, Cimiotti JP, Heusinger AS, Aiken LH. Nurse reports from the frontlines: analysis of a statewide nurse survey. Nurs Forum. 2011;46(1):4-10.
68. McHugh MD, Kutney-Lee A, Cimiotti JP, Sloane DM, Aiken LH. Nurses' widespread job dissatisfaction, burnout, and frustration with health benefits signal problems for patient care. Health Aff (Millwood). 2011;30(2):202-210.
69. McHugh MD, Ma C. Wage, work environment, and staffing: effects on nurse outcomes. Policy Polit Nurs Pract. 2014;15(0):72-80.
70. Khamisa N, Peltzer K, Oldenburg B. Burnout in relation to specific contributing factors and health outcomes among nurses: a systematic review. Int J Environ Res Public Health. 2013;10:2214-2240.
71. AMN Healthcare. 2017 Survey of Registered Nurses. Available at https://www.amnhealthcare.com/amn-insights/nursing/surveys/survey-of-registered-nurses-2017. Last accessed March 1, 2024.
72. Wakim N. Occupational stressors, stress perception levels, and coping styles of medical surgical RNs: a generational perspective.J Nurs Adm. 2014;44(12):632-639.
73. AMN Healthcare. 2013 Survey of Registered Nurses. Available at https://www.amnhealthcare.com/amn-insights/nursing/surveys/2013-survey-of-registered-nurses. Last accessed March 1, 2024.
74. Aiken LH, Sermeus W, Van den Heede K, et al. Patient safety, satisfaction, and quality of hospital care: cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ. 2012;344:e1717.
75. Erickson RJ, Grove WJC. Why emotions matter: age, agitation, and burnout among registered nurses. Online J Issues Nursing. 2007;13.
76. Peckham C. Medscape Lifestyle Report 2017: Race and Ethnicity, Bias and Burnout. Available at https://www.medscape.com/features/slideshow/lifestyle/2017/overview. Last accessed March 1, 2024.
77. Moore GA, Dienemann JA. Job satisfaction and career development of men in nursing. J Nurs Ed Pract. 2014;4(3):86-93.
78. Stutting HL. The relationship between rest breaks and professional burnout among nurses. Crit Care Nurse. 2023;43(6):48-56.
79. Toh SG, Ang E, Devi MK. Systematic review on the relationship between the nursing shortage and job satisfaction, stress and burnout levels among nurses in oncology/hematology settings. Int J Evid Based Healthc. 2012;10(2):126-141.
80. Pinevich Y, Clark KJ, Harrison AM, Pickering BW, Herasevich V. Interaction time with electronic health records: a systematic review. Appl Clin Inform. 2021;12(4):788-799.
81. Khan AR, Rosenthal CD, Ternes K, et al. Time spent by intensive care unit nurses on the electronic health record. Crit Care Nurse. 2022;42(5):44-50.
82. Browning L, Ryan C, Thomas S, Greenberg M, Rolniak S. Nursing specialty and burnout. Psychol Health Med. 2007;12(2):148-154.
83. Hunsaker S, Chen HC, Maughan D, Heaston S. Factors that influence the development of compassion fatigue, burnout, and compassion satisfaction in emergency department nurses. J Nurs Scholarsh. 2015;47(2):186-194.
84. American Nurses Association. Nurse Staffing. Available at https://www.nursingworld.org/practice-policy/nurse-staffing. Last accessed March 15, 2021.
85. American Nurses Association. Safe Staffing. Available at http://ana.aristotle.com/SitePages/safestaffing.aspx. Last accessed March 15, 2021.
86. American Association of Nurse Anesthesiology. Patient Safety: Fatigue, Sleep, and Work Schedule Effects. Available at https://www.aana.com/wp-content/uploads/2023/01/patient-safety-fatigue-sleep-and-work-schedule-effects-011523.pdf. Last accessed March 1, 2024.
87. National Association of Neonatal Nurses. The Impact of Advanced Practice Nurses' Shift Length and Fatigue on Patient Safety: Position Statement #3064. Available at http://nann.org/uploads/Membership/NANNP_Pubs/APNs_Shift_Length_and_Fatigue-FINAL_04-16-15.pdf. Last accessed March 1, 2024.
88. Lesniak J. The Case for Taking a Break. Available at https://engage.healthynursehealthynation.org/blogs/9/38. Last accessed March 1, 2024.
89. Faubion D. 25 Common Examples of Autonomy in Nursing and How to Get More. Available at https://www.nursingprocess.org/autonomy-in-nursing.html. Last accessed March 1, 2024.
90. Doran D, Clarke S, Hayes L, Nincic V. Nurses' expert opinions of workplace interventions for a healthy working environment: a Delphi survey. Nurs Leadersh (Tor Ont). 2014;27(3):40-50.
91. U.S. Congress. S.1113 (118th): The Nurse Staffing Standards for Hospital Patient Safety and Quality Care Act of 2023. Available at https://www.congress.gov/bill/118th-congress/senate-bill/1113. Last accessed March 14, 2021.
92. Yarbrough S, Martin P, Alfred D, McNeill C. Professional values, job satisfaction, career development, and intent to stay. Nurs Ethics. 2017;24(6):675-685.
93. Sagherian K, McNeely C, Cho H, Steege LM. Nurses' rest breaks and fatigue: the roles of psychological detachment and workload.West J Nur Res. 2023;45(10):885-893.
94. Stimpfel AW, Sloane DM, Aiken LH. The longer the shifts for hospital nurses, the higher the levels of burnout and patient dissatisfaction. Health Aff (Millwood). 2012;31(11):2501-2509.
95. Chen J, Davis KG, Daraiseh NM, Pan W, Davis LS. Fatigue and recovery in 12-hour dayshift hospital nurses. J Nurs Manag. 2014;22(5):593-603.
96. Bae SH, Yoon J. Impact of states' nurse work hour regulations on overtime practices and work hours among registered nurses. Health Serv Res. 2014;49(5):1638-1658.
97. Rogers AE. The effects of fatigue and sleepiness on nurse performance and patient safety. In: Hughes RG (ed). Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville, MD: Agency for Healthcare Research and Quality; 2008.
98. Karliner LS, Napoles-Springer AM, Schillinger D, Bibbins-Domingo K, Pérez-Stable EJ. Identification of limited English proficient patients in clinical care. J Gen Intern Med. 2008;23(10):1555-1560.
99. Flores G. The impact of medical interpreter services on the quality of health care: a systematic review. Med Care Res Rev. 2005;62(3):255-299.
100. Karliner LS, Jacobs EA, Chen AH, Mutha S. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv Res. 2007;42(2):727-754.
101. American Association of Critical-Care Nurses. AACN Standards for Establishing and Sustaining Healthy Work Environments. Available at https://www.aacn.org/wd/hwe/docs/hwestandards.pdf. Last accessed March 1, 2023.
102. Wei H, Sewell KA, Woody G, Rose MA. The state of the science of nurse work environments in the United States: a systematic review. Int J Nurs Sci. 2018;5(3):287-300.
103. Groff-Paris L, Terhaar M. Using Maslow's pyramid and the National Database of Nursing Quality Indicators to attain a healthier work environment. Online J Issues Nurs. 2010;16(1):6.
104. American Psychiatric Nurses Association. Self Care Tip Sheet for Nurses. Available at https://www.apna.org/wp-content/uploads/2021/03/APNASelfCareTipSheet.pdf. Last accessed March 1, 2024.
105. Galinsky E, Bond JT, Kim S, et al. Overwork in America: When the Way We Work Becomes Too Much. Available at https://cdn.sanity.io/files/ow8usu72/production/adba773f25d46c0b714d577bd3ab61fea450a069.pdf. Last accessed March 1, 2024.
106. Ruotsalainen JH, Verbeek JH, Marine A, Serra C. Preventing occupational stress in healthcare workers. Cochrane Database Syst Rev. 2014;12:CD002892.
107. Girdano DA, Everly GS, Dusek DE. Controlling Stress and Tension. Needham Heights MA: Allyn & Bacon; 1996.
108. Indeed.com. Career Development: 11 Tips to Help Balance Work and Family Life. Available at https://www.indeed.com/career-advice/career-development/balance-work-and-family. Last accessed March 1, 2024.
109. National Council of State Boards of Nursing. Substance Use Disorder in Nursing. Available at https://wwwncsbn.org/nursing-regulation/practice/substance-use-disorder/substance-use-in-nursing.page. Last accessed March 1, 2024.
110. Velando-Soriano A, Ortega-Campos E, Gómez-Urquiza JL, et al. Impact of social support in preventing burnout syndrome in nurses: a systematic review. Jpn J Nurs Sci. 2020;17(1):e12269.
111. Worden JW. Grief Counseling and Grief Therapy: A Handbook for the Mental Health Practitioner. 5th ed. New York, NY: Springer; 2018.
112. American Nurses Association. Survey of 76,000 Nurses Probes Elements of Job Satisfaction. Available at https://pubmed.ncbi.nlm.nih.gov/16927745. Last accessed March 1, 2024.
113. Montoro-Rodriguez J, Small JA. The role of conflict resolution styles on nursing staff morale, burnout, and job satisfaction in long-term care. J Aging Health. 2006;18(3):385-406.
114. Soriano-Vázquez I, Cajachagua Castro M, Morales-García WC. Emotional intelligence as a predictor of job satisfaction: the mediating role of conflict management in nurses. Front Pub Health. 2023;11:1249020.
115. American Nurses Association. Year One COVID-19 Impact Assessment Survey. Available at https://www.nursingworld.org/practice-policy/work-environment/health-safety/disaster-preparedness/coronavirus/what-you-need-to-know/year-one-covid-19-impact-assessment-survey. Last accessed March 1, 2024.
116. Tang CJ, Chan SW, Zhou WT, Liaw SY. Collaboration between hospital physicians and nurses: an integrated literature review. Int Nurs Rev. 2013;60(3):291-302.
117. The Joint Commission. Health care worker fatigue and patient safety. Sentinel Event Alert (Addendum 2018). 2011;(48). Available at https://www.jointcommission.org/-/media/tjc/documents/resources/patient-safety-topics/sentinel-event/sea_48_hcw_fatigue_final_w_2018_addendum.pdf. Last accessed March 1, 2024.
118. Piers RD, Van den Eynde M, Steeman E, et al. End-of-life care of the geriatric patient and nurses' moral distress. J Am Med Dir Assoc. 2012;13:e7-e13.
119. American Nurses Association. What is Nurse Burnout? How to Prevent It. Available at https://www.nursingworld.org/content-hub/resources/workplace/what-is-nurse-burnout-how-to-prevent-it. Last accessed March 1, 2024.
120. Van Wyk BE, Pillay-Van Wyk V. Preventive staff-support interventions for health workers. Cochrane Database Syst Rev. 2014;4:CD003541.
121. Wilkinson S, Perry R, Blanchard K, Linsell L. Effectiveness of a three-day communication skills course in changing nurses' communication skills with cancer/palliative care patients: a randomised controlled trial. Palliat Med. 2008;22(4):365-375.
122. Penoyer DA. Nurse staffing and patient outcomes in critical care: a concise review. Crit Care Med. 2010;38(7):1521-1529.
123. Rogowski JA, Staiger D, Patrick T, Horbar J, Kenny M, Lake ET. Nurse staffing and NICU infection rates. JAMA Pediatr. 2013;167(5):444-450.
124. American Nurses Association. ANA Position Statement: Addressing Nurse Fatigue to Promote Safety and Health: Joint Responsibilities of Registered Nurses and Employers to Reduce Risks. Available at https://www.nursingworld.org/~4afdfc/globalassets/practiceandpolicy/health-and-safety/nurse-fatigue-position-statement-final.pdf. Last accessed March 1, 2024.
125. Walsh R. Emergency Nurses Association White Paper: Nurse Fatigue. Available at https://enau.ena.org/Listing/Nurse%20Fatigue%20White%20Paper. Last accessed March 1, 2024.
Mention of commercial products does not indicate endorsement.