Atrial fibrillation is one of the most common arrhythmias encountered in clinical practice today. Current treatment options for atrial fibrillation include pharmacological cardioversion, direct current electric cardioversion, radiofrequency ablation, and long-term rate control with a wide variety of oral antiarrhythmic medications. The specific treatment(s) selected to manage atrial fibrillation in adult patients must be tailored to each individual's needs, clinical symptoms, and response to any previous treatment. The efficacy, safety, and cost of the treatment option must also be evaluated. This course will review current treatment options for the clinical management of atrial fibrillation, including indications for use, risks, and criteria for evaluating the treatment's efficacy. Recommendations from the American Heart Association and Agency for Healthcare Research and Practice will be reviewed. Finally, the clinical management of a patient with acute onset atrial fibrillation and a patient with chronic atrial fibrillation will be explored in depth through the use of simulated case studies.
- INTRODUCTION
- A BRIEF REVIEW OF NORMAL ELECTRICAL CONDUCTION
- A REVIEW OF ELECTROCARDIOGRAM WAVEFORM
- ATRIAL FIBRILLATION
- ASSESSMENT OF THE PATIENT WITH ATRIAL FIBRILLATION
- ESTABLISHING THE MEDICAL PLAN OF CARE
- PHARMACOLOGIC THERAPY
- PHARMACOLOGIC THERAPY FOR RATE CONTROL
- PHARMACOLOGIC CARDIOVERSION
- ELECTRICAL CARDIOVERSION
- PHARMACOLOGIC THERAPY FOR MAINTENANCE OF NORMAL SINUS RHYTHM
- PREVENTION OF THROMBOEMBOLIC COMPLICATIONS
- RADIOFREQUENCY ABLATION AND CRYOABLATION IN THE MANAGEMENT OF ATRIAL FIBRILLATION
- MANAGEMENT OF ATRIAL FIBRILLATION FOLLOWING CORONARY ARTERY BYPASS GRAFT SURGERY
- ATRIAL FIBRILLATION IN WOLFF-PARKINSON-WHITE SYNDROME
- SIMULATED CASE STUDY: THE PATIENT WITH ACUTE-ONSET ATRIAL FIBRILLATION
- SIMULATED CASE STUDY: CLINICAL MANAGEMENT OF THE PATIENT WITH PERSISTENT ATRIAL FIBRILLATION
- CONCLUSION
- RESOURCES
- Works Cited
- Evidence-Based Practice Recommendations Citations
This course is designed for physicians, physician assistants, nurses, and other healthcare professionals working in an adult healthcare setting, where they are likely to encounter patients who are (or should be) receiving medical intervention for control of atrial fibrillation.
The purpose of this course is to provide a basic review of current treatment options for the management of atrial fibrillation and indications for use, risks, and criteria for evaluating the treatment's efficacy.
Upon completion of this course, you should be able to:
- Describe cardiac conduction and the components of an ECG waveform.
- Use your knowledge of the pathophysiology of atrial fibrillation, including key defining characteristics, to differentiate it from other arrhythmias and predict impact on normal functioning.
- Outline common cardiac and noncardiac causes of atrial fibrillation.
- List key clinical data, including subjective symptoms, past medical history, physical assessment findings, and diagnostic/laboratory tests, important to obtain when assessing a patient with atrial fibrillation.
- Identify key components that should be considered in the development of the medical plan of care, including the issue of generic drug substitution.
- Compare and contrast antiarrhythmic medications appropriate to use for acute and chronic rate control for patients with atrial fibrillation.
- Outline the use of pharmacologic therapy in the restoration of normal sinus rhythm, including indications for use and procedure for administration.
- Describe electrical cardioversion, including indications and pre- and postprocedure care.
- Discuss antiarrhythmic medications that may be used to maintain normal sinus rhythm in a patient following successful spontaneous, electrical, or pharmacologic cardioversion.
- Select appropriate pharmacologic measures that may be used to reduce risk of thromboembolic events in persons with atrial fibrillation.
- Discuss the use of radiofrequency ablation of the atrioventricular (AV) node in the clinical management of atrial fibrillation.
- Describe the causes and recommended management of atrial fibrillation in adult patients following coronary artery bypass graft surgery and in patients with Wolff-Parkinson-White syndrome.
- Using simulated case study data, develop a best practice strategy for the clinical management of atrial fibrillation.
Karen Majorowicz, RN, is currently employed in the Cardiac Intermediate Care Unit at Shands Healthcare at the University of Florida, Gainesville. She received her Master's in Medical-Surgical Nursing in 1978 from the University of Maryland. Karen has created numerous instructional manuals on Medicare and has conducted educational programs on cardiovascular assessment.
Contributing faculty, Karen Majorowicz, RN, has disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
John M. Leonard, MD
Mary Franks, MSN, APRN, FNP-C
The division planners have disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
Sarah Campbell
The Director of Development and Academic Affairs has disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
The purpose of NetCE is to provide challenging curricula to assist healthcare professionals to raise their levels of expertise while fulfilling their continuing education requirements, thereby improving the quality of healthcare.
Our contributing faculty members have taken care to ensure that the information and recommendations are accurate and compatible with the standards generally accepted at the time of publication. The publisher disclaims any liability, loss or damage incurred as a consequence, directly or indirectly, of the use and application of any of the contents. Participants are cautioned about the potential risk of using limited knowledge when integrating new techniques into practice.
It is the policy of NetCE not to accept commercial support. Furthermore, commercial interests are prohibited from distributing or providing access to this activity to learners.
Supported browsers for Windows include Microsoft Internet Explorer 9.0 and up, Mozilla Firefox 3.0 and up, Opera 9.0 and up, and Google Chrome. Supported browsers for Macintosh include Safari, Mozilla Firefox 3.0 and up, Opera 9.0 and up, and Google Chrome. Other operating systems and browsers that include complete implementations of ECMAScript edition 3 and CSS 2.0 may work, but are not supported. Supported browsers must utilize the TLS encryption protocol v1.1 or v1.2 in order to connect to pages that require a secured HTTPS connection. TLS v1.0 is not supported.
The role of implicit biases on healthcare outcomes has become a concern, as there is some evidence that implicit biases contribute to health disparities, professionals' attitudes toward and interactions with patients, quality of care, diagnoses, and treatment decisions. This may produce differences in help-seeking, diagnoses, and ultimately treatments and interventions. Implicit biases may also unwittingly produce professional behaviors, attitudes, and interactions that reduce patients' trust and comfort with their provider, leading to earlier termination of visits and/or reduced adherence and follow-up. Disadvantaged groups are marginalized in the healthcare system and vulnerable on multiple levels; health professionals' implicit biases can further exacerbate these existing disadvantages.
Interventions or strategies designed to reduce implicit bias may be categorized as change-based or control-based. Change-based interventions focus on reducing or changing cognitive associations underlying implicit biases. These interventions might include challenging stereotypes. Conversely, control-based interventions involve reducing the effects of the implicit bias on the individual's behaviors. These strategies include increasing awareness of biased thoughts and responses. The two types of interventions are not mutually exclusive and may be used synergistically.
#90824: Clinical Management of Atrial Fibrillation
Atrial fibrillation is one of the most commonly sustained arrhythmias seen in medical practice. It is estimated that 12.1 million people in the United States will have atrial fibrillation in 2030 [1,2]. Consider the following statistics [3,4,5,6,7,8]:
Increasing age is a major risk factor for the development of atrial fibrillation. As the American population continues to age, increasing numbers of elderly individuals will require medical care for the management of atrial fibrillation.
Atrial fibrillation is associated with increased morbidity and mortality, especially in the elderly population.
Elderly individuals who develop atrial fibrillation and also have a history of congestive heart failure, myocardial infarction, and/or left ventricular dysfunction are at increased risk for poor outcomes and complications.
Atrial fibrillation is a major independent risk factor for thromboembolic cerebrovascular accidents (CVAs). CVAs may result in death or serious disability.
Hospital stays for management of atrial fibrillation are longer than hospital stays for the treatment of other arrhythmias.
The clinical management of atrial fibrillation presents a complex challenge to the clinician. A wide variety of pharmacologic and nonpharmacologic therapies is available for the treatment of atrial fibrillation. Therapy should be individualized to each specific patient. Carefully assess the patient's status and past medical history with an emphasis on the patient's specific pattern of atrial fibrillation, including its onset, duration, and precipitating factors, the symptoms experienced during atrial fibrillation, the impact of the arrhythmia on the patient's activities of daily living, risk factors for atrial fibrillation, findings from laboratory and diagnostic tests, and history of cardiovascular disease.
It is important to match patient assessment data with an appropriate medical management plan. Common goals seen in the management of atrial fibrillation include rate control, restoration of normal sinus rhythm, maintenance of normal sinus rhythm, and prevention of thromboembolic complications.
The selection of appropriate pharmacologic and nonpharmacologic therapies for the patient should be based on the identified goal(s) and patient assessment data. A wide range of antiarrhythmic medications is available with varying effects on the electrical conduction system in the heart. Some are contraindicated in the presence of concurrent illnesses, such as hypertension and asthma. Nonpharmacologic therapies include direct current (electrical) cardioversion, radiofrequency ablation, and atrial or dual chamber pacemakers.
Regular follow-up is required to monitor the effectiveness of the therapy in meeting the identified medical goals. Evaluation criteria include a rate that is controlled within desired parameters, increased ability to perform activities of daily living, reduction in severity of attacks of atrial fibrillation, absence of undesired side effects of prescribed antiarrhythmic medications, and absence of any thromboembolic complications.
In the normal heart, the heartbeat is initiated by the sinoatrial (SA) node. From the SA node, the electrical impulse travels through both the right and left atria, causing depolarization of the atria. Atrial depolarization is followed by atrial contraction and atrial repolarization. The electrical impulse travels from the atria to the atrioventricular (AV) node located in the inferior wall of the right atrium. The speed of conduction slows in the AV node to allow time for the atria to depolarize, contract, and complete ventricular filling. From the AV node, the electrical impulse travels through the bundle of His located in the septum of the heart. The bundle of His divides into the right and left bundle branches. These branches divide further into the smaller fibers of the Purkinje system. Electrical conduction through the His-Purkinje system is rapid, causing rapid depolarization of both the right and left ventricles. Depolarization of the ventricular cells spreads from the apex of each ventricle to the base and moves from the endocardium to the epicardium. Ventricular depolarization is followed by ventricular contraction and ventricular repolarization [9,10,11].
When an electrical impulse stimulates a cardiac cell, a series of events is initiated that causes the cell to depolarize and repolarize. This generates an action potential that allows the electrical impulse to propagate, ultimately resulting in the contraction of the cells of the myocardium. The basic events that occur during the formation of the action potential are as follows:
When an electrical impulse stimulates a cardiac cell, the cell depolarizes. Positively charged sodium ions from the extracellular space flood rapidly into the intracellular space. This increases the total number of positively charged ions in the intracellular space, and the charge in the intracellular space becomes less negative. The potential or voltage in the cell increases. This is phase 0 of the development of the action potential.
The flood of sodium ions into the intracellular space stops very quickly. It is followed by a brief and incomplete period of repolarization. This period is mediated by a temporary movement of potassium ions from the intracellular to the extracellular space. This brief period of repolarization is referred to as phase 1 of the action potential.
Phase 2 of the action potential is characterized by a balance of inward and outward movement of ions. Calcium ions move slowly through select channels into the intracellular space while potassium ions move out through multiple channels into the extracellular space. This initiates a slow repolarization and creates a plateau in the action potential. Cardiac contraction is mediated by phase 2.
In phase 3, the calcium channels close. The process of repolarization is accelerated.
In phase 4, electrical diastole occurs. Except for the SA node, the heart rests. The SA node begins the process of initiating the next electrical impulse.
After the myocardial cell has depolarized, there is a period of time during which the cell cannot generate an action potential in response to another electrical impulse; this is referred to as the "absolute refractory period." As the cell continues to repolarize, an "effective refractory period" occurs in which the cell can transiently depolarize in response to an electrical impulse but generally will not develop enough of an action potential to propagate the impulse to surrounding cells. As repolarization nears completion, the cell is said to be in a "relative refractory period." In this period, a strong electrical stimulus can trigger the cell to depolarize and create another action potential [12,13,14].
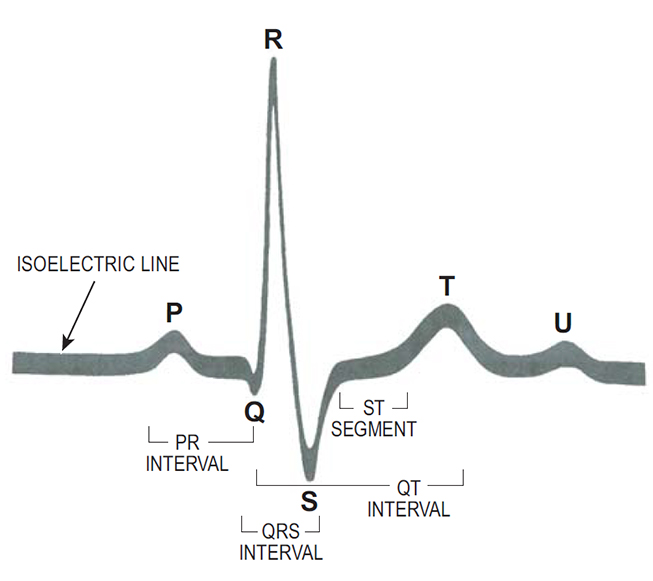
The electrical events that occur in the heart are reflected in the electrocardiogram (ECG) waveform. The components of a normal beat are (Figure 1):
The P wave represents atrial depolarization.
The PR interval represents the amount of time the electrical impulse takes to travel from the SA node through the AV node. The normal PR interval is 0.12 to 0.20 seconds.
The QRS interval represents the amount of time it takes the ventricles to depolarize. In normal conduction, ventricular depolarization occurs rapidly. This rapid conduction is reflected in a narrow QRS interval. The normal duration of a QRS interval is <0.10 seconds.
The T wave represents ventricular repolar-ization.
The QT interval represents the amount of time that it takes the ventricles to depolarize and repolarize; it is measured from the beginning of ventricular depolar-ization (i.e., the start of the QRS interval) to the end of repolarization (i.e., the end of the T wave). During the early part of the QT interval, the ventricles are completely refractory and unable to respond to another electrical impulse. During the latter part of the interval, the ventricles are only partially refractory and may respond to some impulses but not to others. The normal QT interval is <0.44 seconds.
When changes occur in the normal cardiac cycle, the normal ECG waveform is altered to reflect them. For example, prolonged repolarization is reflected in a prolonged QT interval. A slowing of conduction from the SA node through the AV node may be reflected in a prolonged PR interval. Abnormal conduction of the electrical impulse through the ventricles results in a QRS interval that is wider than usual or bizarre in shape. Careful analysis of the changes in a patient's ECG can provide valuable information in the diagnosis and treatment of the arrhythmia [6,15].
Antiarrhythmic medications interrupt or prevent arrhythmias by altering electrical conduction in the heart. Some antiarrhythmic medications have a single mechanism of action, but many have multiple mechanisms. In general, antiarrhythmic medications may act by:
Prolonging the normal development of the action potential
Inhibiting or slowing the movement of sodium or calcium ions into the intracellular space
Altering the movement of potassium ions out of the intracellular space
Altering the speed at which the impulse is conducted through the AV node
Prolonging ventricular repolarization and the refractory period
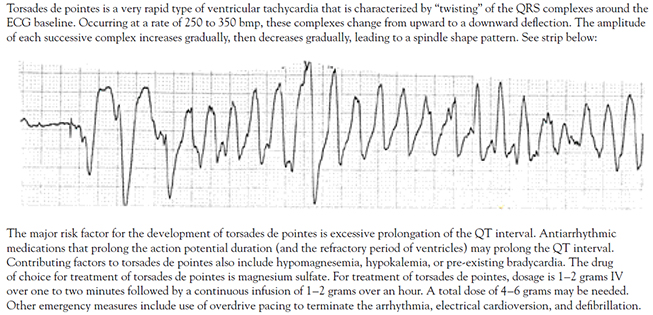
Because antiarrhythmic medications impact specific events in cardiac conduction, they run the risk of creating new arrhythmias or worsening existing arrhythmias. Arrhythmias caused by the administration of an antiarrhythmic medication are referred to as proarrhythmias. Proarrhythmias can range from mild to severe. Serious proarrhythmias include ventricular tachycardia, torsades de pointes, and ventricular fibrillation. We will look at the actions and properties of specific antiarrhythmic agents in more detail in later sections.
Atrial fibrillation is an arrhythmia characterized by rapid, disorganized electrical activity in the atria. Instead of the SA node depolarizing to initiate a heartbeat, ectopic (or abnormal) areas in the atria depolarize rapidly and irregularly, resulting in chaotic atrial activity. Because of the chaotic electrical activity, normal atrial depolarization does not occur. Patchy areas of the atria may attempt to contract, giving the atria a "quivering" appearance, but the unified contraction of both the right and left atria (needed to complete active filling of the ventricles) cannot occur. One theory suggests that the mechanism underlying atrial fibrillation is the development of multiple impulses or "wavelets" in the atria. These impulses wander around and through the atria, getting caught in a cycle that continuously circulates in the atria, triggering small, erratic areas of depolarization. In atrial fibrillation, atrial impulses may be generated at a rate as high as 300 impulses per minute. Atrial impulses bombard the AV node. However, because of its inherent characteristics, the AV node tends to limit ventricular response to the atrial stimulation. Because the AV node is less excitable than the nearby atrial or ventricular cells, it conducts impulses more slowly, and its refractory period (when it cannot respond to another electrical stimulus) is relatively prolonged. Recently, there has been a re-assessment of the multiple wavelet hypothesis, demonstrating that the substrates of atrial fibrillation at the clinical level are focal trigger sites of action potentials rather than multiple micro re-entry sites [16].
Conduction in the AV node is also "decremental." This means that, as the impulse is conducted through the AV node, the action potentials that are generated have less and less ability to stimulate new action potentials. In atrial fibrillation, some atrial impulses are "blocked" or lost in the AV node because the action potentials that are generated are insufficient to stimulate further electrical activity.
Finally, the AV node has the property of concealed conduction. An atrial impulse may enter the AV node, stimulate depolarization of initial cells in the node, and be blocked from further conduction. Although the impulse is not sufficient to generate ventricular depolarization, it depolarizes enough cells in the AV node to create a refractory period. Subsequent impulses entering the AV node immediately following that impulse will be blocked. The AV node will be unable to accept or respond to them until repolarization has occurred. Due to the combination of slowed, decremental, and concealed conduction, the AV node can limit ventricular rate in atrial fibrillation to less than 200 beats per minute (bpm). It is important to note that these properties of the AV node create a relationship between atrial and ventricular rates in atrial fibrillation: when the atrial rate increases, the ventricular rate decreases. However, when the atrial rate slows, the ventricular rate may actually increase. At a slower rate, more atrial impulses are likely to stimulate the AV node at a time when the impulse can be conducted through the AV node to the ventricles [17,18,19].
Clinicians who work with patients who have atrial fibrillation are aware that the longer atrial fibrillation persists, the harder it becomes to terminate the arrhythmia and maintain normal sinus rhythm. Research suggests that atrial fibrillation triggers a process known as "atrial remodeling." In atrial remodeling, electrical, histologic, anatomic, and autonomic nervous system changes occur in the atria that facilitate the continuation of atrial fibrillation and impair the heart's ability to return to normal sinus rhythm [20,21,22]. Changes that have been hypothesized include:
Gradual enlargement of the atria through dilation and stretching. Atrial hypertrophy may increase the vulnerability of the atria to abnormal electrical impulses and may shorten the atrial refractory period. A shortened refractory period facilitates development of the continuous loop or cycle of impulses (also called a re-entry mechanism) that sustains atrial fibrillation.
Alteration in the normal flow of one or more ions (especially calcium ions) across the cardiac cell membrane, leading to generation of a cellular substrate that facilitates the onset of arrhythmia.
Progressive shortening of the effective refractory period in the atria.
Adrenergic activation may contribute to the initiation of ectopic activity
Additional factors have emerged to complement the arrhythmogenic substrate that shed light on the perpetuation of arrhythmia. These include inflammation, fibrosis, altered gap junctions, and genetic predisposition, which are yet to be fully characterized across the different stages of atrial fibrillation [23,24,25,26,27].
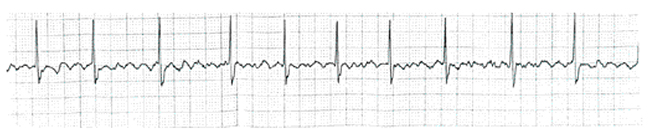
The two key defining characteristics of atrial fibrillation are (Figure 2) [5,17,19]:
Total absence of normal sinus P waves. The absence of P waves indicates that the heartbeat was not initiated in the SA node, or normal pacemaker, of the heart. The P waves are replaced by fibrillatory (fib) waves. These fib waves may be so fine that they are indiscernible or barely discernible; or, they may be very coarse and more clearly seen on the ECG tracing.
An irregularly irregular ventricular response when conduction through the AV node is normal.
Additional characteristics associated with atrial fibrillation include:
A variable ventricular rate. The rate may range from less than 60 bpm to as high as 160 bpm.
A QRS interval that is usually (but not always) normal in configuration and duration.
The types of atrial fibrillation may be described in terms of onset or duration of rate. Descriptions based on rate include the following [17]:
Rapid ventricular response: atrial fibrillation with a ventricular rate greater than 120 bpm.
Controlled ventricular response: atrial fibrillation with a ventricular rate between 60 bpm and 110 bpm.
Slow ventricular response: atrial fibrillation with a ventricular rate of less than 60 bpm.
Descriptions based on onset and duration have not been standardized throughout medical literature. Terms such as acute onset, chronic, and others have been used. In its published practice guidelines, the American College of Cardiology, the American Heart Association, and the European Society for Cardiology (ACC/AHA/ESC) Task Force recommends the following simplified terminology for episodes of atrial fibrillation that last more than 30 seconds and are not caused by another, reversible medical cause [28]:
First-detected: the first diagnosed or known episode of atrial fibrillation that a patient experiences. A first-detected episode may be symptomatic or asymptomatic; it may or may not be self-limited. It may or may not actually be the patient's first episode of atrial fibrillation; however, it is the first episode that is formally identified as atrial fibrillation.
Paroxysmal: recurrent atrial fibrillation that spontaneously terminates or terminates with intervention within seven days of onset, and episodes may recur with variable frequency.
Persistent: recurrent atrial fibrillation that is sustained beyond seven days; it may include atrial fibrillation that is terminated by electrical cardioversion or pharmacologic therapy. This category also includes cases of long-standing atrial fibrillation (e.g., longer than one year) that usually lead to permanent atrial fibrillation.
Permanent: paroxysmal or persistent atrial fibrillation in which pharmacologic and/or electrical cardioversion is not attempted or is not successful.
Nonvalvular: atrial fibrillation in the absence of rheumatic mitral stenosis, a mechanical or bioprosthetic heart valve, or mitral valve repair.
Atrial fibrillation is one of several arrhythmias in which the electrical impulse is initiated at or above the AV node. These arrhythmias are usually referred to using the umbrella term, supraventricular tachycardias (SVT). Other common SVTs include atrial flutter and AV nodal re-entrant tachycardia.
In atrial flutter, the heartbeat originates in the atria somewhere outside the SA node. More organized than fib waves, atrial flutter (F) waves have a characteristic sawtooth appearance. Early studies designated atrial flutter with rates between 240 and 340 bpm as "type I flutter," and this term has commonly been applied to typical atrial flutter. An electrocardiographic appearance of atrial flutter with a rate faster than 340 bpm was designated as "type II flutter;" the mechanisms for type II flutter remain undefined [28]. The atrial rate is typically 240 to 300 bpm, but conduction delays in the atrial circuit due to scars from prior ablation, surgery, or antiarrhythmic drugs can slow the rate to less than 150 bpm in some patients [28]. One or more flutter waves may be present before each QRS interval. Conduction through the AV node is often regular (i.e., every second or third or fourth flutter wave is conducted). The most common pattern is 2:1 conduction, which results in a ventricular rate of 150 bpm. Flutter waves do not result in organized contraction of the atria, but they may increase atrial oxygen demands by triggering "near contractions." Atrial flutter is generally differentiated from atrial fibrillation by the presence of flutter waves that are more defined than fib waves and occur at regular intervals and regular ventricular rhythm [29]. The relationship between atrial fibrillation and atrial flutter may explain why 80% of patients who undergo radiofrequency catheter ablation of typical atrial flutter will have atrial fibrillation within the following five years [28].
In AV nodal re-entrant tachycardia, the ventricular rate falls between 150 and 250 bpm. Because of the abrupt onset and termination of the re-entrant SVT, the nonspecific term paroxysmal supraventricular tachycardia has been used to refer to these tachyarrhythmias. With improved knowledge of the electrophysiology of re-entrant SVT, greater specificity in nomenclature, based on the mechanisms of re-entry, has been possible [30]. With AV nodal re-entrant tachycardia, no evidence of atrial activity is present. The ventricular rhythm is regular. The arrhythmia has an abrupt onset and termination, with episodes lasting from seconds or minutes to days, and may occur in persons with no history of heart disease as well as in elderly persons with chronic heart disease. The arrhythmia may be differentiated from sinus tachycardia by rate; sinus tachycardia rarely exceeds a rate of 150 to 160 bpm in an adult at rest. It may also be differentiated from atrial fibrillation because the rhythm is regular. It may be differentiated from atrial flutter by rate; the usual rates associated with AV nodal re-entrant tachycardia are too slow for 1:1 (atrial to ventricular) conduction in atrial flutter and too fast for 2:1 conduction [17,30].
Differential diagnosis of atrial fibrillation is based on ECG analysis combined with patient history, description of symptoms, current medications, and past medical history [31]. At a controlled rate, atrial fibrillation is usually readily recognizable because of the absence of sinus P waves and the irregularly irregular rhythm. However, at higher rates, identification of these key characteristics may become more difficult. The physician may choose to facilitate diagnosis through the use of intravenous adenosine. Adenosine is a medication that may be administered intravenously to aid in the differential diagnosis of a narrow complex SVT [32]. Adenosine should not be administered in the presence of a wide QRS complex tachyarrhythmia, nor should it be administered if the arrhythmia's underlying mechanism has already been identified [31]. Adenosine has an immediate onset of action and an extremely short half-life (i.e., <10 seconds) [33]. Care should be taken to administer the medication rapidly enough to ensure that the medication reaches the systemic circulation before its half-life expires. Due to its extremely short half-life, adenosine is not effective for pharmacologic cardioversion; as soon as the effects wear off, the original arrhythmia resumes. Adenosine acts by interrupting re-entry pathways and slowing conduction through the AV node; it slows the ventricular rate to permit analysis and identification of the exact arrhythmia. Side effects include bradycardia, a brief period of asystole that does not exceed 15 seconds, and a sense of flushing and lightheadedness. It is a potent vasodilator and may cause hypotension. The side effects may be uncomfortable for the patient but are usually short and self-limiting [12,14,19,34]. In 2013, the U.S. Food and Drug Administration (FDA) issued a warning of a rare but serious risk of myocardial infarction and death with the use of adenosine [35]. Adenosine should be avoided in patients with unstable angina or cardiovascular instability. When administering adenosine, follow these tips [12,14,19,33,36]:
Make sure that the patient has a good IV access.
Administer adenosine undiluted through a proximal IV access.
Administer an initial dose of 6 mg over one to two seconds. Follow the medication quickly with a rapid normal saline flush to make sure that the entire dose reaches systemic circulation. Remember that the rapid administration rate is vital for effectiveness. If adenosine is administered too slowly, it may have the adverse effect of further increasing heart rate.
Continuously monitor ECG and heart rate before, during, and after administration. Record a continuous strip during administration to assess the arrhythmia when the rate slows or the arrhythmia breaks and resumes.
After one to two minutes, if the initial dose is ineffective, a second dose of 12 mg may be given as a rapid one- to two-second bolus. The second dose should also be followed with a rapid saline flush.
Note that a single dose should not exceed 12 mg.
If the second dose is ineffective, another 12 mg dose may be given after several minutes, to a maximum of 18–24 mg.
Atrial fibrillation causes a drop in cardiac output. Atrial contraction does not occur, thereby reducing ventricular filling during mechanical diastole. Loss of atrial contraction (or "atrial kick") may reduce cardiac output from 5% to 40%. Symptoms of decreased cardiac output may develop; how severe these symptoms are depends on multiple factors, including the person's age, overall health, and presence of structural heart disease. If atrial fibrillation occurs at a rapid ventricular rate, cardiac output is reduced further. Any tachycardia reduces ventricular filling time. When ventricular filling is already reduced due to the loss of atrial kick, further reduction in filling time from a rapid heart rate may greatly exacerbate signs of reduced cardiac output. Over time, atrial fibrillation with a rapid ventricular response may cause a tachycardia-induced cardiomyopathy. This cardiomyopathy may be reversible when the heart rate is controlled [17,19]. Loss of atrial contraction also causes stasis of blood in the atria. Stasis of blood increases the risk of thrombus formation and can lead to the development of thromboembolic complications such as CVAs [17,29].
The causes of atrial fibrillation may be grouped into three major categories [5,37]:
Primary arrhythmia in the absence of structural heart disease or other precipitating causes
Secondary arrhythmia associated with a range of cardiovascular diseases
Secondary arrhythmia in the absence of heart disease but in the presence of a systemic problem that precipitates the arrhythmia
Historically, atrial fibrillation, as a primary arrhythmia, was thought to develop in isolation, with no known precipitating cause. Called "lone atrial fibrillation," this type of atrial fibrillation was defined as occurring in the presence of documented normal left ventricular function, typically in people 60 years of age or younger. It was characterized by a paroxysmal onset and termination and frequent recurrence. However, a Working Group of the American College of Cardiology suggests that the category of lone (idiopathic) atrial fibrillation is no longer mechanistically or clinically useful [2]. The Working Group posits several reasons for avoiding use of the term "lone atrial fibrillation," including [2]:
Outdated terminology, as the term "lone atrial fibrillation" predates current understanding of the many disorders that may contribute to the initiation of atrial fibrillation
Broad definition of and variation in what investigators have termed "lone atrial fibrillation," leading to confusion and diminished usefulness of the term
Wide variation in the reported prevalence (0.2% to 68%) of lone atrial fibrillation
No specificity in requirement for extensiveness and interval of baseline imaging to exclude heart disease
Well-established heritability of atrial fibrillation not taken into account when classifying an individual as having lone atrial fibrillation
Lack of unique pathophysiologic mechanisms attributed to lone atrial fibrillation
Instead, the term "paroxysmal atrial fibrillation" should be used.
As a secondary arrhythmia, atrial fibrillation may be caused by cardiac and noncardiac causes. Common cardiac causes include [37,38,39]:
Hypertension
Rheumatic heart disease
Mitral valve disease (e.g., mitral stenosis, mitral valve prolapse, mitral valve annular calcification)
Congestive cardiomyopathy/congestive heart failure
Acute myocardial infarction
Sick sinus syndrome
Pericarditis
Hypertrophic cardiomyopathy
May occur following cardiac/coronary artery bypass graft (CABG) surgery
The persons at highest risk to develop atrial fibrillation are those with long-standing hypertension, valvular heart disease, left ventricular hypertrophy, depressed left ventricular function, and coronary artery disease. Atrial fibrillation associated with cardiovascular disease may initially have a paroxysmal onset; however, the arrhythmia can continue to progress to persistent or chronic atrial fibrillation. Noncardiac, systemic diseases may also cause atrial fibrillation. Diabetes mellitus is a major risk factor for the development of atrial fibrillation. Other noncardiac causes include [2,37,38,39]:
Hyperthyroidism
Male sex
Advancing age
Obesity
Obstructive sleep apnea
Genetic factors
Alcohol and drug use
Noncardiac surgery
Noncardiac diagnostic procedure
Pulmonary conditions/hypoxemia caused by pulmonary conditions (e.g., pneumonia, chronic obstructive pulmonary disease [COPD])
Pulmonary embolus
Over-the-counter use of some herbs, such as ephedra or ginseng
Emerging risk factors for atrial fibrillation include [2]:
Subclinical atherosclerosis
Chronic kidney disease
Inflammation
Increased height, birth weight
Smoking
Caffeine intake
Ethnicity
Atrial fibrillation caused by noncardiac causes is frequently reversible once the underlying condition is resolved. In some instances, the atrial fibrillation may spontaneously convert to normal sinus rhythm. In other cases, the arrhythmia responds well to pharmacologic or electrical cardioversion to restore normal sinus rhythm [37].
Patients in atrial fibrillation can present with symptoms that range from asymptomatic to severely incapacitating. Consider these patient examples:
Patient K is 68 years of age. He is found to be in controlled atrial fibrillation during a routine physical before surgery for a total knee repair. He reports that he has experienced no symptoms and has never before been told that he has an irregular heartbeat or arrhythmia.
Patient J is 45 years of age. She presents to the emergency department with atrial fibrillation with rapid ventricular response. An ECG shows her heart rate to be 160 bpm. She complains of feeling palpitations and slightly short of breath. She gives a history of intermittent episodes of palpitations and dyspnea that start and stop abruptly. She reports feeling frightened and out of control because her symptoms occur without warning and without obvious precipitating cause.
Patient W is 76 years of age. He presents to the emergency department with severe dyspnea and dizziness. His blood pressure is hypotensive at 85/50 mm Hg. His respirations are 32 breaths per minute, and he has rales in both lung bases. His oxygen saturation on room air is 87%. His ECG shows atrial fibrillation with rapid ventricular response at a rate of 140–160 bpm. Patient W gives a history of coronary artery disease, previous myocardial infarction, and long-standing hypertension. He reports that his symptoms started about a week earlier and have gradually grown worse.
Patient C is 58 years of age. She makes an appointment to see her physician and reports that she has been experiencing a "pounding heartbeat" intermittently for the last few days. She denies other symptoms but admits that she has been "more tired" than usual and that she has not "gotten as much done during the day as usual." Patient C has a history of mitral valve disease and a mitral valve replacement several years earlier. She also has mild (Class I/II) congestive heart failure. An ECG shows Patient C to be in atrial fibrillation at a relatively controlled rate of 80–90 bpm.
As the simulated patient examples show, symptoms of atrial fibrillation may include one or more of the following [37,38,39]:
Palpitations
Decreased blood pressure
Fatigue
Dizziness
Shortness of breath
Exacerbation of congestive heart failure
Chest pain (angina)
Syncope or near syncope
Reduced exercise tolerance
Because of the unpredictable pattern of paroxysmal atrial fibrillation, patients with this type of atrial fibrillation may feel frightened and out of control. They may choose to curtail their usual level of activity in an attempt to prevent the arrhythmia from occurring. Depression and a sense of helplessness may occur.
Atrial high-rate episodes may be detected by a cardiac implantable electronic device. These cases should result in further evaluation to establish the diagnosis and guide treatment decisions [40].
Physical assessment findings in atrial fibrillation may include the following [28,37]:
Rapid heart rate and irregularly irregular heart rhythm
Irregular jugular venous pulsations
Variable loudness of S1
Variable pulse pressure. This results from the variable ventricular filling caused by the irregular conduction of atrial impulses through the AV node to the ventricles.
A blood pressure that appears to vary widely. In atrial fibrillation with a controlled or slow ventricular response, there may be long pauses between some beats. When an electronic, noninvasive blood pressure device is used (or when the pressure is released too rapidly during manual auscultation of blood pressure), the systolic blood pressure reading may vary widely. Taking serial blood pressure readings and using an average of readings to estimate the patient's actual blood pressure may be needed.
Hypotension, especially if cardiac output is significantly reduced
Signs of congestive heart failure, such as decreased oxygen saturation and rales/crackles in lung fields
Signs of poor peripheral perfusion, such as diminished peripheral pulses and impaired capillary filling
Assessment of the patient with atrial fibrillation should include laboratory and diagnostic tests to identify any factors that may be contributing to the development of the arrhythmia as well as to rule out any noncardiac causes of the arrhythmia. Appropriate laboratory and diagnostic tests may include the following [10,28,37,38,39]:
Serial cardiac enzymes to evaluate for possible acute myocardial infarction
Arterial blood gases to assess for hypoxia
Thyroid function studies to evaluate for hyperthyroidism
Serum electrolytes, particularly imbalances in sodium, potassium, or magnesium
Complete blood count to evaluate hematocrit and hemoglobin. Anemia may aggravate angina and signs of decreased cardiac output.
Chest x-ray to evaluate for signs of congestive heart failure or underlying pulmonary disease/pneumonia
Ultrasound studies (i.e., echocardiography [ECHO]) to identify valvular disease and evaluate left ventricular function
Transesophageal ECHO (TEE) to evaluate for presence of clots in atria (most sensitive and specific technique for this purpose)
12-lead ECG to evaluate arrhythmia
Continuous ambulatory ECG monitoring for patients who complain of symptoms associated with atrial fibrillation but are in normal rhythm upon presentation to healthcare system/emergency department
Nuclear medicine cardiac studies
When a patient does not speak the same language as the clinician, a professional interpreter should be consulted to ensure accurate communication. A systematic review of the literature has shown that the use of professional interpreters provides better clinical care than the use of "ad hoc" interpreters, with the former improving the quality of care for patients with limited English language skills to a level equal to that for patients with no language barriers [41,42]. Use of professional interpreters has been associated with improvements in communication (errors and comprehension), utilization, clinical outcomes, and satisfaction with care [41,42]. Individuals with limited English language skills have indicated a preference for professional interpreters rather than family members [43].
Effective clinical management of the patient with atrial fibrillation is based on evaluation of the patient's status, identification of appropriate medical goals, and determination of which specific therapies will be most effective in assisting the patient to reach the identified goal(s).
Until the 2000s, no consensus existed about what therapy or combination of therapies is the most effective in the clinical management of atrial fibrillation. In 2001, the ACC/AHA/ESC task force was formed to make recommendations for the management of persons with atrial fibrillation. Through a process of rigorous and expert evaluation of published data, the Task Force derived specific guidelines that have been published in the American Journal of Cardiology and are available on the AHA website [44]. The Task Force updated these guidelines in 2014 and again in 2019 [28,40]. Effective clinical management of the person with atrial fibrillation begins with a thorough history and assessment of the patient to identify the patient's type and pattern of atrial fibrillation [28,40]. Based on the patient's type and pattern of atrial fibrillation, symptoms, and underlying cause, appropriate medical goals should be identified. Specific therapies are then selected based on the identified goals [45].
Adequate patient assessment should focus on the patient's symptoms, past medical history, any concurrent illnesses, and psychosocial issues. When assessing the patient, consider the following [46]:
What type of atrial fibrillation does the patient have? Is this a first detected episode? Does the patient have recurrent paroxysmal, recurrent persistent, or permanent atrial fibrillation?
How often does the patient experience atrial fibrillation? How long does it last? What precipitates it? What terminates it?
What specific symptoms does the patient have?
What impact do the symptoms have on the patient's ability to work? Take care of himself/herself? His/her activity tolerance? Does the patient feel frightened? Disabled by the symptoms?
What impact is the atrial fibrillation having on any other medical problems that the patient has? Is it exacerbating his/her angina? Is it exacerbating his/her congestive heart failure?
Does the patient have some type of cardiovascular disease? Coronary artery disease? Hypertension? Valvular heart disease? History of myocardial infarction? History of congestive heart failure?
Does the patient have some other systemic problem that is precipitating the atrial fibrillation?
Is the patient elderly?
Has the patient been treated for atrial fibrillation? What treatment was prescribed? How effective was that treatment? Did the patient follow the prescribed treatment? Did it work? Did side effects develop?
How will the patient pay for his/her medical care and medications? What medications and treatments will his/her insurance pay for?
Is the patient able and willing to comply with prescribed medication therapy? Has the patient been compliant with medication therapy in the past?
What is the patient's renal and hepatic function? Are these normal?
Based on a thorough evaluation of the patient's status and other factors, one or more medical goals should be identified. The initial goal for a patient who is hemodynamically unstable is the immediate restoration of normal sinus rhythm through electrical cardioversion. The initial goal for patients who present with atrial fibrillation with a rapid ventricular response is rate control. Once the patient's status has stabilized, long-term goals may be developed. When developing long-term goals, consider the following points [17,28,40,45,46,47,48,49]:
Use of antiarrhythmic therapy may not be necessary for persons with asymptomatic paroxysmal atrial fibrillation.
Use of antiarrhythmic therapy is indicated for persons who experience severe symptoms with paroxysmal atrial fibrillation.
Long-term rate control is indicated for persons with paroxysmal, persistent, or permanent atrial fibrillation.
Long-term rate control is also indicated for patients who have repeatedly reverted to atrial fibrillation following electrical or pharmacologic cardioversion. Ablation for symptomatic persistent atrial fibrillation and for severely symptomatic recurrent atrial fibrillation may be indicated. AV nodal ablation is usually reserved for elderly patients, because it leads to pacemaker dependency.
Catheter ablation performed in experienced centers may be indicated to maintain sinus rhythm in select patients with significantly symptomatic, paroxysmal atrial fibrillation who have failed treatment with an antiarr-hythmic drug and have normal or mildly dilated left atria, normal or mildly reduced LV function, and no severe pulmonary disease.
Catheter ablation is indicated for symptom-atic patients with atrial fibrillation who have Wolff-Parkinson-White (WPW) syndrome. Prompt direct-current cardioversion is recommended for patients with WPW syndrome and rapid ventricular response who are hemodynamically compromised.
Restoration of normal sinus rhythm is indicated for those who have persistent signs of decreased cardiac output during episodes of atrial fibrillation.
Direct-current cardioversion may be indicated as part of a long-term management strategy to restore sinus rhythm in patients with atrial fibrillation.
Maintenance of normal sinus rhythm may be indicated for persons who spontaneously convert from atrial fibrillation to sinus rhythm.
Maintenance of normal sinus rhythm is indicated for persons who are successfully converted by pharmacologic or electrical means.
Elimination or interruption of the arrhythmia through radiofrequency ablation (of the focal source of the arrhythmia or the AV node) is indicated for patients who cannot tolerate antiarrhythmic therapy, whose arrhythmia is not successfully controlled by optimal doses of antiarrhythmic therapy, or who cannot be successfully cardioverted through pharmacologic or electrical means. Some patients with atrial fibrillation who also have atrial flutter may benefit from treatment with radiofrequency ablation.
To assist the clinician in selecting and prioritizing appropriate medical goals, the ACC/AHA/ESC Task Force established recommendations for the management of various types of atrial fibrillation. These recommendations are summarized in Table 1.
RECOMMENDED MANAGEMENT FOR PERSONS WITH ATRIAL FIBRILLATION
| Type of Atrial Fibrillation | Recommended Management Strategy | |||||||
|---|---|---|---|---|---|---|---|---|
| First-detected, self-limiting |
| |||||||
| First-detected, persistent |
| |||||||
| Recurrent paroxysmal |
| |||||||
| Recurrent persistent |
| |||||||
| Permanent |
|
Antiarrhythmic medications are the mainstay of treatment for atrial fibrillation. They may be used for acute and chronic rate control. They also may be used for pharmacologic cardioversion of atrial fibrillation to normal sinus rhythm and maintenance of normal sinus rhythm following successful conversion; however, their use for achieving rhythm control has decreased due to evidence of greater safety and lower costs for hospitalization obtained from the use of rate-control strategies [28,50]. The AHA/ACC/HRS recommends treating the precipitating or reversible causes of atrial fibrillation prior to initiating antiarrhythmic drug therapy [28]. Whatever the goal of treatment, selection of specific antiarrhythmic medications should be guided by the following [28,50]:
Patient characteristics (e.g., age, disease states, renal function, concurrent drug therapies)
Effectiveness of the medication in meeting identified goals (i.e., controlling rate within desired parameters, limiting episodes of atrial fibrillation)
Specific action of the medication on the cardiac cycle and its risk of proarrhythmias and other serious side effects
Medical contraindications to the use of some antiarrhythmic medications in the presence of specific cardiovascular disorders
Convenience of administration (i.e., dosing, frequency, schedule of doses)
Cost and ready availability of the medication(s)
With the increasing emphasis on reduction of healthcare costs, there has been an increase in the use of generic (as opposed to proprietary) medications. Almost every state has passed regulations encouraging the substitution of less expensive drug products for more expensive proprietary products. State regulations may approve substitutions only for medications on an approved list, or the regulations may permit the substitution of any medication, except those specifically listed on a list of exclusions. On the national level, the FDA provides a specific list of approved drugs. This list is updated on a monthly basis [51].
When a pharmaceutical company develops a new drug, the company may apply for one or more patents for (1) the drug itself; (2) the manufacturing process; (3) how the drug is delivered to the bloodstream; or (4) how the medication is to be used. Although the patent gives the company exclusive rights to the new drug for 17 years, this period often involves at least 10 years of development. In reality, the company may have only seven years to exclusively sell the drug. A newly developed drug is given several names. The generic name, which is the medication's official name (derived from the drug's chemical name, structure, and/or formula), must be unique. Generic names are frequently difficult to pronounce, remember, and spell. The new drug is also given a trade name or proprietary name that signifies that the drug is the exclusive property of its company. Trade names are simpler, easier to remember, and often emphasize an attribute of the medication. Trade names must also be unique. After the patent on a specific drug has expired, other companies may manufacture and sell that drug under its generic name. Generics are frequently sold at a lower price than trade/proprietary drugs. Generic versions of a drug must meet FDA approval, specifically the following three points [51,52]:
The generic preparation must contain the same amount of active drug ingredient as the original proprietary preparation.
The generic must be manufactured according to federal standards as defined in the Good Manufacturing Practices.
In the human body, the generic medication must be released in equivalent fashion (i.e., same rate, to same extent) as the proprietary drug. This is referred to as "bioequivalence." Bioequivalence is established by a drug company through the use of small research studies. For time-release medications, the process of establishing bioequivalence is more strict, extensive, and time-consuming. Because there is more variation inherent in the use of time-release forms, more extensive testing is required to ensure bioequivalence. Because of the cost and extensiveness of the process, very few time-release generic drugs are available.
Proprietary and generic versions of a medication may vary in several respects [33,52]:
Appearance of the medication. By law the size, color, and shape of the generic must significantly differ from the proprietary. Patients will notice the difference.
Different inactive ingredients. While the active ingredients must be the same, the inactive components may vary. Inactive ingredients are routinely used in medications to add bulk, to keep the tablet from crumbling/disintegrating until use, to help the medication dissolve, or to provide a pleasant taste. There have been instances in which the difference in inactive ingredients has changed the absorption of the active ingredients.
Variable bioequivalence. Regulations permit as much as a 20% variation in bioequivalence. For medications, such as antiarrhythmic medications that may have a very narrow margin for therapeutic effect, this variation may alter how effective the generic medication is in managing the patient's arrhythmia.
Practically speaking, the use of a generic substitution means that the patient could experience different effectiveness with different preparations. Random switching from proprietary to generic or from one generic to another could increase side effects, decrease rate control, and cause more frequent relapse from normal sinus rhythm to atrial fibrillation. For that reason, any generic substitution of antiarrhythmic medications should be done very carefully. With many antiarrhythmic medications, very small variations in the serum blood level may influence the effectiveness of the medication in controlling the arrhythmia and significantly increase the risk of proarrhythmias and serious side effects. Physician groups have made the following recommendations regarding the use of generic antiarrhythmic medications [46]:
Regardless of the preparation used, closely monitor the patient's status and serum drug levels. Adjust dosage as indicated by data.
Avoid substitution of antiarrhythmic medications for patients with life-threatening arrhythmias, arrhythmias that cause loss of consciousness, or when a change in drug level (increase) can cause life-threatening proarrhythmias.
Use a generic for less serious arrhythmias if an easy, reliable assay is available and a therapeutic drug level is stable and sustained over time.
If generic substitution is necessary, give preference to generic medications that have only one preparation available, thus avoiding multiple switches from one generic product to another. Also give preference to a generic preparation that is widely available in hospital and outpatient pharmacies.
If switching from a proprietary to a generic medication, re-establish effectiveness and proper dose with the new preparation.
The physician may wish to specify on the prescription the exact preparation of a medication to be dispensed. Some states have regulations that limit the physician's ability to specify preparations. Also, specifying a proprietary medication may present a financial issue for the patient; insurance companies may not cover the higher cost preparation.
A classification system for antiarrhythmic drugs was developed in the early 1970s. An antiarrhythmic medication was classified according to its specific effect on the normal cardiac cycle. When the classification system was developed, it was believed that each antiarrhythmic medication had only one action. Electrophysiologic research has shown that the mechanisms involved in the generation and spread of an electrical impulse throughout the heart are complex, and that antiarrhythmic medications may impact more than one of these mechanisms. Although the classification system does not reflect the advances in the understanding of electrophysiology, it is still in common use today. Table 2 summarizes the classification system [53,54].
CLASSIFICATION OF ANTIARRHYTHMIC MEDICATIONS
| Class | Action/Properties | Class Proarrhythmic Effects | Specific Agents | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ia |
|
|
| ||||||||||
| Ib |
|
|
| ||||||||||
| Ic |
| Re-entry arrhythmias |
| ||||||||||
| II |
|
|
| ||||||||||
| III |
|
|
| ||||||||||
| IV |
|
|
| ||||||||||
| AV = atrioventricular; SA = sinoatrial. | |||||||||||||
When selecting and initiating (or changing) antiarrhythmic therapy, the site of care should be considered. Sites of care may include the patient's home, a physician's office, an outpatient clinic, or an inpatient setting. Some antiarrhythmics, such as dofetilide, can only be initiated in an inpatient setting. For others, inpatient initiation is strongly recommended if risk of proarrhythmia is high. Proarrhythmic risk is increased in persons with structural heart disease, congestive heart failure, and those who already have a prolonged QT interval. Persons who have no structural heart disease and whose QT interval is normal are considered to be at low risk for development of proarrhythmias. In these cases, antiarrhythmic therapy may be initiated in outpatient settings. If antiarrhythmic therapy is initiated outside the hospital setting, transtelephone monitoring may be used to intermittently assess the patient's heart rate and rhythm for any undesired changes [55].
When selecting antiarrhythmic agents, potential drug interactions should be considered. Serious interactions may occur between two antiarrhythmic medications, between an antiarrhythmic and other cardiovascular medications, and between antiarrhythmics and noncardiac medications. Interactions that may occur include the following [12,14,19,33,52]:
Other drugs may potentiate or inhibit the effectiveness of antiarrhythmic drugs.
Other drugs may interfere with the normal absorption of antiarrhythmic drugs, thus reducing the serum level and the drug's effectiveness in controlling an arrhythmia.
Other drugs may interfere with the normal metabolism or excretion of another medication, thus increasing the serum levels and increasing the risk of toxicity.
Antiarrhythmic drugs may potentiate or inhibit the therapeutic effects of other medications.
Antiarrhythmic drugs may interfere with the normal absorption, metabolism, or excretion of another medication, thus reducing the serum level and the drug's effectiveness.
When given concurrently with other antiarrhythmic drugs, an antiarrhythmic drug may have cumulative effects on heart rate and blood pressure.
Table 3 lists some common drug to drug interactions.
COMMON DRUG TO DRUG INTERACTIONS OF ANTIARRHYTHMIC DRUGS (AADs)
| AAD | AAD Increases the Level of Action | AAD Inhibits the Action | AAD Serum Levels Increased | AAD Serum Levels Decreased | Other Considerations and Comments | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Amiodarone |
| — |
| — |
| ||||||||||||||||||||
| Digoxin | — | — |
|
| Concurrent administration of medications such as thiazide diuretics, ticarcillin, or amphotericin B that cause hypokalemia can increase risk of digitalis toxicity | ||||||||||||||||||||
| Diltiazem |
| — |
|
| Additive effects on heart rate, blood pressure, force of cardiac contraction can occur with administration concurrently with calcium channel blockers, or beta blockers | ||||||||||||||||||||
| Disopyramide | Warfarin | — |
|
|
| ||||||||||||||||||||
| Dofetilide | — | — |
| — |
| ||||||||||||||||||||
| Esmolol | Succinylcholine | Theophylline | Digoxin | Thyroid preparations |
| ||||||||||||||||||||
| Flecainide | Digoxin | — |
| — |
| ||||||||||||||||||||
| Ibutilide | — | — | — | — | Significant risk of dangerously prolonged QT intervals when administered concurrently with other medications that prolong QT interval | ||||||||||||||||||||
| Metoprolol | May alter effectiveness of insulin and oral hypoglycemic agents |
| — | Thyroid preparations |
| ||||||||||||||||||||
| Procainamide | — | — |
|
| Additive effect if administered with other AADs | ||||||||||||||||||||
| Propafenone |
| — |
| Etravirine |
| ||||||||||||||||||||
| Propranolol | May alter effectiveness of insulin and oral hypoglycemic agents |
| — | Thyroid preparations | Additive myocardial depression possible when administered concurrently with general anesthesia, IV phenytoin, or verapamil | ||||||||||||||||||||
| Quinidine |
| — |
|
| — |
When a person presents with uncontrolled atrial fibrillation, his/her ventricular rate may reach 160 bpm. The immediate goal of medical therapy is to control the heart rate to decrease acute symptoms, relieve hypotension, reduce signs of ischemia, and reduce or prevent signs of congestive heart failure from developing. No single agent has been found to be more effective than others in controlling rapid rates. For acute rate control, the administration route of choice is intravenous. Antiarrhythmic drugs commonly prescribed for acute rate control include diltiazem, verapamil, esmolol, metoprolol, and digoxin [49].
Diltiazem acts by blocking calcium transport into the myocardial and vascular smooth muscle cells. As a result, conduction through the SA and AV nodes is slowed, and the refractory period of the AV node is prolonged. Ventricular rate is slowed, but the underlying atrial arrhythmia is not corrected. Diltiazem should be administered initially as an IV bolus. The usual dose is a 0.25 mg/kg bolus administered over a two-minute period. Diltiazem has a rapid onset of action. If effective, it should slow the patient's heart rate within three to seven minutes of administration. If the initial dose is ineffective in slowing the patient's heart rate, the bolus may be repeated at a higher dose of 0.35 mg/kg over two minutes. The patient's heart rate and rhythm and blood pressure should be monitored during administration. Bradycardia, bradyarrhythmias such as heart block, and hypotension may occur. To achieve or maintain rate control, a continuous infusion may be started following bolus administration. The infusion may be started at 10 mg/hour and increased in increments of 5 mg/hour to achieve rate control if no undesirable side effects occur. Diltiazem should be used with caution in patients with congestive heart failure, known pre-existing conduction defects, and significant hypotension [33,60].
Verapamil, another calcium channel blocker, also slows ventricular rate by slowing conduction through the AV node and prolonging the refractory period of the AV node. Revised guidelines published by the AHA/ACC/HRS recommend a loading or bolus dose of 0.075–0.15 mg/kg administered over two minutes; no maintenance or continuous drip is included in the recommendations [28]. If ineffective in achieving rate control and if no untoward effects occur, the bolus may be repeated at a higher dosage of 10 mg administered 30 minutes after the initial dose [28]. Verapamil should not be used for patients with atrial fibrillation secondary to WPW syndrome or patients who have a wide QRS complex tachyarrhythmia. Verapamil should be used with caution for persons with pre-existing conduction disturbances or left ventricular dysfunction. The patient's heart rate and rhythm and blood pressure should be monitored during and following administration. Bradycardia, heart block, and hypotension may occur [33,61].
Esmolol is a short-acting beta-adrenergic blocker that slows ventricular rate in atrial fibrillation by slowing conduction through the AV node. Initial administration is an IV bolus dose/loading dose of 0.5 mg/kg administered over one minute [28]. The bolus should be followed with an infusion of 0.05 mg/kg/min for four minutes. If the desired rate control is achieved, the infusion should be continued at that rate. If adequate rate control is not achieved at that dose, the bolus should be repeated followed by an infusion of 0.1 mg/min for four minutes. The total dose should not exceed 200 mcg/kg/min [33]. This procedure may be repeated until rate control is achieved or undesirable side effects occur. The patient's heart rate, ECG rhythm, and blood pressure should be monitored during the administration. Hypotension may occur. Once rate control is achieved, the infusion should be reduced to 0.025 mg/kg/min. Because esmolol has a short half-life, the therapeutic effects and side effects usually reverse within 10 to 20 minutes after the infusion is stopped. Because the therapeutic effects wear off quickly, care should be taken when switching the patient to an oral preparation to prevent relapse/loss of rate control. To transition the patient to oral medication, the first dose of the oral medication should be administered while the patient is still receiving esmolol. Thirty minutes after the first oral dose is given, the esmolol infusion should be reduced by one-half. The second dose of the oral agent should be administered at its scheduled time. One hour after the scheduled administration of the second oral dose, assess the patient's heart rate, ECG rhythm, and blood pressure. If rate control is maintained, the esmolol infusion may be discontinued. Note: Esmolol has no oral preparation; long-term control by oral agent requires a different agent [33].
Metoprolol is a longer acting beta-adrenergic blocking agent that decreases conduction through the AV node. Although metoprolol is not labeled for use in the management of atrial arrhythmias, it is used by some clinicians to control/slow ventricular rate in atrial fibrillation with a rapid ventricular response. For acute rate control, an IV bolus of 2.5–5 mg may be given over two minutes and repeated every two to five minutes up to a total of 15 mg in a 10- to 15-minute period. The patient's heart rate, ECG rhythm, and blood pressure should be monitored closely. Bradycardia, bradyarrhythmias, heart block, and hypotension may occur. Use of metoprolol is contraindicated for persons with bradycardia, AV conduction problems, uncompensated congestive heart failure, or asthma [33,62].
Digoxin is an older agent that may be used to control ventricular rate in some patients. Once considered a leading treatment for rate control in atrial fibrillation, digoxin is primarily recommended for persons with atrial fibrillation who also have congestive heart failure caused by systolic dysfunction. Digoxin acts by prolonging the refractory period of the AV node as well as slowing conduction through SA and AV nodes. Digoxin therapy is initiated by either an oral or intravenous loading dose protocol. Intravenous administration should be used in an acute situation. The revised AHA/ACC/HRS guideline notes that one-half the total digitalizing dose (TDD) of 9–12 mcg/kg may be administered over five minutes with the remaining portion as 25% fractions at four- to eight-hour intervals or 0.25 mg may be given intravenously every two hours up to a total of 1.5 mg over 24 hours followed by an oral maintenance regimen [28]. These doses should be given at six- to eight-hour intervals. The usual protocol for an oral loading dose is 0.75–1.5 mg given in three to four doses every six to eight hours. The maintenance oral dose is 0.125–0.25 mg once daily [28]. Careful monitoring of serum digoxin levels is recommended. For digoxin to achieve a therapeutic effect, the serum digoxin level must fall within the therapeutic level of 0.5–2 ng/mL. The therapeutic range for digoxin is very narrow. Serum levels in excess of 2 ng/mL are considered toxic and may cause tachyarrhythmias, bradycardia, heart block and bradyarrhythmias, and other symptoms [12,14,19,33,37,47,63].Table 4 summarizes information about antiarrhythmic medications used for acute rate control.
PHARMACOLOGIC THERAPY FOR ACUTE RATE CONTROL IN ATRIAL FIBRILLATION
| Agent | Class | Action | Dosage/Route | Side Effects | Comments | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Diltiazem | IV |
|
|
|
| ||||||||||||||||||||||||
| Verapamil | IV |
| IV loading dose: 0.075–0.15 mg/kg over 2 mins |
|
| ||||||||||||||||||||||||
| Esmolol | II |
|
|
|
| ||||||||||||||||||||||||
| Metoprolol | II |
| IV loading dose: 2.5–5 mg over 2 mins and repeated every 2 to 5 mins up to a total dose of 15 mg in a 10- to 15-min period |
|
| ||||||||||||||||||||||||
| Digitalis (Digoxin) | None |
|
|
|
| ||||||||||||||||||||||||
| AV = atrioventricular; CHF = congestive heart failure; SA = sinoatrial; TDD = total digitalizing dose. | |||||||||||||||||||||||||||||
If the long-term goal of clinical management is rate control, there are a number of oral preparations to choose from. Clinical decision making includes selecting the category, specific agent, effective dose, and preparation (e.g., short-acting, extended-release). As with acute rate control, no consensus exists on the best medication(s) for every patient. Specific antiarrhythmic agents should be selected on the basis of patient assessment. Again, factors to consider include the cost and complexity of the prescribed regimen, the risk of proarrhythmic effects, concurrent cardiovascular disease, and the risk of other troublesome or serious side effects. When choosing long-term therapy, the patient's lifestyle should be considered as well. Some medications provide effective rate control when the patient is at rest but do not provide adequate rate control during activity or exercise. A heart rate is considered "controlled" if it falls between 60 to 80 bpm at rest and 90 to 115 bpm with moderate exercise [20]. Adequate rate control may be achieved by a single antiarrhythmic drug, or it may require a combination of drugs. Antiarrhythmic drugs commonly used for long-term rate control include calcium channel blockers, beta blockers, and digoxin [49].
See Table 5 for a summary of antiarrhythmic medications that may be used for long-term rate control in atrial fibrillation.
ANTIARRHYTHMIC AGENTS USED FOR LONG-TERM RATE CONTROL IN ATRIAL FIBRILLATION
| Agent | Class | Action | Dosage/Route | Side Effects | Comments | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Diltiazema | IV |
|
|
|
| |||||||||||||||||||||||
| Verapamil | IV |
|
|
|
| |||||||||||||||||||||||
| Digitalis (Digoxin) | None |
|
|
|
| |||||||||||||||||||||||
| Metoprolola | II |
|
|
|
| |||||||||||||||||||||||
| Propranolol | II |
| Oral maintenance dose: 30–160 mg daily in divided doses |
| Propranolol may also be used in the management of angina, hypertension, prevention and management of MI | |||||||||||||||||||||||
| ||||||||||||||||||||||||||||
Oral diltiazem preparations provide chronic rate control in atrial fibrillation and are a drug of choice for persons who have a physically active lifestyle; however, their use for rate control is unlabeled [33]. Diltiazem comes in immediate- and extended-release forms. Immediate-release doses must be taken three to four times per day; extended-release forms require only daily dosing. In addition to bradycardia, hypotension, and heart block, other side effects of oral diltiazem include flushing, angina, insomnia, headache, nausea, syncope, and signs of congestive heart failure. Care should be taken when diltiazem is combined with negative inotropic drugs, other calcium channel blockers, and digoxin. Combination therapy increases the risk of bradycardia, conduction abnormalities, hypotension, and signs of congestive heart failure [33,60].
Oral verapamil preparations may also be prescribed for chronic rate control. Available in immediate- and extended-release forms, oral verapamil can control ventricular rate at rest and with activity. In addition, research has shown that verapamil may have the additional benefit of reducing atrial electrophysiologic remodeling (the process thought to be responsible for frequent recurrence of atrial fibrillation and resistance to successful cardioversion). Immediate-release preparations must be taken three to four times per day at evenly spaced intervals; extended-release dosing may be administered once per day. Oral verapamil should be used with caution in persons with conduction defects and left ventricular dysfunction. Oral verapamil should not be prescribed for persons with WPW syndrome. There is increased risk of bradycardia, bradyarrhythmias, conduction abnormalities, hypotension, and development of congestive heart failure when combined with administration of other calcium channel blockers, negative inotropes, or digoxin [33,61].
Oral digoxin may be the first drug of choice for patients with atrial fibrillation and congestive heart failure caused by systolic dysfunction [67]. Digoxin does not provide adequate rate control during exercise or activity. The usual oral maintenance dose of digoxin is 0.125–0.25 mg daily. Serum digoxin levels should be monitored periodically. The patient should be monitored for signs of digitalis toxicity. The patient and/or family should be taught to recognize key signs of toxicity. These include nausea and vomiting, headache, unexplained weakness, malaise, and visual disturbances as well as slow heart rate. ECG changes that may occur with digitalis toxicity include sinus bradycardia, heart block, and multiple tachyarrhythmias. Digitalis toxicity is more likely to occur in elderly persons. Electrolyte imbalances such as hypokalemia, renal failure, or combined therapy with other antiarrhythmic agents may potentiate the effects of digoxin and increase the risk of digitalis toxicity. Severe digitalis toxicity may be treated with digoxin immune Fab [33].
Fab is an antibody produced in sheep. When Fab is administered intravenously, it binds to unbound digoxin in the bloodstream and facilitates its removal, thus reducing the serum digoxin level. The precise dose of Fab may be calculated on the basis of the amount of digitalis ingested or on the patient's serum digoxin level. In emergency situations when the amount of digoxin ingested is not known and a serum digoxin level is not available, a Fab dose of 800 mg in two divided doses may be administered IV. This dose should be diluted according to package instructions and administered over 15 to 30 minutes. Continuous monitoring of ECG, pulse, blood pressure, and temperature before and during infusion should be done. Following the administration of Fab, persons with atrial fibrillation (or a history of atrial fibrillation) may experience recurrence of the arrhythmia or a loss of rate control, and persons with congestive heart failure may develop signs of an exacerbation such as dyspnea, hypotension, or rales [33].
Oral metoprolol is not labeled for management of atrial fibrillation; however, in patients with coronary artery disease, hypertension, and angina, it may be prescribed for rate control plus its other therapeutic effects. Its off-label use for rate control in patients with paroxysmal, persistent, or permanent atrial fibrillation is recommended by the AHA/ACC/HRS [28]. It may exert cumulative effects on heart rate, rhythm, and blood pressure when given in combination with calcium channel blockers, other beta blockers, or disopyramide resulting in bradycardia, bradyarrhythmias/heart block, and hypotension. The usual oral dose may range from 25–100 mg twice daily. Metoprolol is available in short-acting and extended-release preparations. Extended-release preparations are administered only once per day. Side effects include those common to beta blockers [33].
Oral propranolol, another beta-adrenergic receptor antagonist, may also be prescribed for long-term rate control in atrial fibrillation. Unlike metoprolol, propranolol is approved for use in atrial fibrillation. The usual oral maintenance dose is 30–160 mg per day in divided doses. Side effects include nausea, vomiting, diarrhea, constipation, insomnia, depression, bronchospasm, hypoglycemia, fatigue, and impotence [33].
Based on the assessment of a patient's status, it may be determined that restoration of normal sinus rhythm is a major goal. Persons who continue to demonstrate signs of decreased cardiac output from loss of atrial kick, such as continuing shortness of breath, fatigue, signs of congestive heart failure, and diminished exercise tolerance despite adequate rate control, may require restoration of sinus rhythm to alleviate symptoms and improve quality of life. Restoring normal sinus rhythm can be done using a combination of approaches, including chemically through the use of intravenous or oral medications, through direct current electrical cardioversion, or through the use of radiofrequency catheter ablation in the setting of appropriate anticoagulation and rate control [28]. Although pharmacologic cardioversion remains more popular, it appears to be most effective when initiated within seven days of the onset of atrial fibrillation [28]. Unlike electrical cardioversion, pharmacologic cardioversion requires no anesthesia, has fewer risks, and is less costly. This section will review the antiarrhythmic medications that may be used for pharmacologic cardioversion, including ibutilide, dofetilide, amiodarone, propafenone, procainamide, quinidine, and flecainide [5,19,20,28,37,45,46,49,53,68,69]. See Table 6 for a summary of select antiarrhythmic agents that may be used for pharmacologic cardioversion.
ANTIARRHYTHMIC AGENTS USED FOR PHARMACOLOGIC CARDIOVERSION
| Agent | Class | Action | Dosage/Route | Side Effects | Comments | ||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ibutilide | III |
|
|
|
| ||||||||||||||||||||||||||||||||||
| Dofetilide | III |
|
|
|
| ||||||||||||||||||||||||||||||||||
| Amiodaronea | III |
|
|
|
| ||||||||||||||||||||||||||||||||||
| Propafenone | Ic |
|
|
|
| ||||||||||||||||||||||||||||||||||
| Procainamide | Ia |
|
|
|
| ||||||||||||||||||||||||||||||||||
| Quinidine | Ia |
|
|
|
| ||||||||||||||||||||||||||||||||||
| Flecainide | Ic |
|
|
|
| ||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||
Ibutilide is a drug approved by the FDA for the acute termination of atrial fibrillation and atrial flutter. A Class III antiarrhythmic, ibutilide acts by prolonging the duration of the action potential, the atrial refractory period, and the ventricular refractory period. It also slightly slows the sinus rate and conduction through the AV node. Ibutilide's exact mechanism of action is unknown [33]. On a cellular level, it has been reported to exert its effects by both blocking repolarizing potassium currents and initiating an inward depolarizing sodium current [56]. Ibutilide does not appear to have a direct impact on cardiac output, but monitoring for conduction disturbances and heart block is recommended [33].
Because ibutilide prolongs the ventricular refractory period (reflected by a prolonged QT interval), the risk of torsades de pointes is significant. Torsades de pointes is a rapid, polymorphic form of ventricular tachycardia. See Figure 3 for more information about torsades de pointes. With ibutilide administration, the risk of torsades de pointes is dependent on the dose of ibutilide administered; the higher the dose, the greater the risk.
For an adult weighing 60 kg or more, the initial dose is 1 mg diluted to a total volume of 50 mL administered over 10 minutes. If conversion to normal sinus rhythm does not occur, the dose may be repeated 10 minutes after completion of the first dose. For patients who weigh less than 60 kg, the dose of ibutilide should be reduced to 0.01 mg/kg administered over 10 minutes [33].
If administered with other antiarrhythmics and medications (e.g., tricyclic antidepressants, dronedarone) that prolong the QT interval, ibutilide can interact with these medications to create a dangerously prolonged QT interval [33].
Prior to administering ibutilide, the patient should be assessed and the following data obtained [28]:
When did the patient's arrhythmia begin? Ibutilide has been found to be most effective in patients with atrial fibrillation of less than two months duration.
What medications is the patient currently taking? Other antiarrhythmic medications that prolong the QT interval should be discontinued before ibutilide administration to reduce the risk of excessive QT prolongation and torsades de pointes.
Is the patient adequately anticoagulated? Because of the risk that cardioversion can cause small pieces of an atrial thrombus to break loose and cause embolization, patients should be adequately anticoagulated prior to receiving ibutilide.
Does the patient have any history of polymorphic ventricular tachycardia (torsades de pointes)? Persons with a past history of torsades de pointes should not be given ibutilide.
Are the patient's serum electrolytes within normal limits? The patient's serum sodium, potassium, magnesium, and calcium levels should be assessed. Also, liver function tests, blood urea nitrogen, and creatinine levels should also be checked and be within normal limits. Hypomagnesemia and hypokalemia must be corrected before ibutilide is administered.
What is the patient's baseline QT interval and rate corrected QT (QTc) interval? See Table 7 for information about calculating corrected QT intervals.
MEASURING QT AND QTc INTERVALS
|
The QT interval reflects ventricular depolarization and repolarization. It is measured from the beginning of the QRS complex to the end of the T wave. The length of the QT interval is normally influenced by the heart rate, and when the rate is faster, the QT interval shortens to promote efficient depolarization, repolarization, and contraction. When the rate is slower, the QT interval is slightly longer. As a rough estimate, the QT interval is considered to be "normal" if it is less than one-half of the RR interval. When administering an antiarrhythmic medication that prolongs the QT interval, it is important to differentiate between a normally lengthened QT interval caused by a slowed heart rate and abnormally prolonged QT interval caused by side effects of the medication. This is done through a measurement known as a rate corrected QT interval or QTc. The upper limit of the QTc for women is 0.43 sec or 430 msec; for men it is 0.42 sec or 420 msec. To calculate the QTc, follow these steps:
A QTc interval that increases by more than 25% from baseline (prior to medication administration) indicates that the QT interval has become dangerously prolonged. |
Prior to administration, ensure that the patient has a good IV access. Continuous ECG monitoring should be initiated. Consider the use of equipment that can be used for monitoring, external pacing, and defibrillation. Or, have pacing/defibrillator patches readily available for use in an emergency [33]. Have emergency equipment readily available, including a defibrillator/cardioverter, external noninvasive pacing equipment, and medications such as magnesium used in the treatment of torsades de pointes/sustained ventricular tachycardia. Some experts suggest that administering IV magnesium sulfate before administering ibutilide may lower the risk of torsades de pointes [73]. Initiate continuous blood pressure monitoring. The patient's blood pressure should be checked every five minutes during the infusion.
To prepare the ibutilide infusion for an adult 60 kg or more, 1 mg of ibutilide is diluted to a total volume of 50 mL. Ibutilide is supplied in vials containing 1 mg/10 mL or 0.1 mg/mL. It may be mixed with either D5W or 0.9 NS. When 1 mg is diluted to a total of 50 mL, the concentration of the solution will be 0.02 mg/mL [33].
Ibutilide must be administered using a volumetric pump. The desired rate is 1 mg over 10 minutes [33]. The pump may be set at a rate of 300 mL/hour or 5 mL/minute to deliver the desired dose at the desired rate. Stop infusion immediately if the patient converts to normal sinus rhythm. If the patient develops new or worsening ventricular arrhythmias, stop the infusion immediately. Check the patient's blood pressure and assess for signs of hemodynamic instability. Following the infusion, the patient's ECG should be continuously monitored for four hours or until the patient's QTc returns to his/her baseline. Although the risk of proarrhythmias is greatest within 20 minutes of the infusion, the risk persists for several hours following administration. The administration of other antiarrhythmics (e.g., amiodarone, quinidine, procainamide, disopyramide, dronedarone) that prolong the QT interval should be avoided for four hours following ibutilide administration. Ibutilide may be used in patients who fail to convert after treatment with propafenone. It may also be used in patients whose arrhythmia recurs during treatment with propafenone or flecainide [5,13,33,53,64].
Dofetilide is a Class III antiarrhythmic approved for use in patients with atrial fibrillation and atrial flutter. Major clinical trials on dofetilide, including the European and Australian Multicenter Evaluation Research on Atrial Fibrillation Dofetilide (EMERALD) and Symptomatic Atrial Fibrillation Investigation and Randomized Evaluation of Dofetilide (SAFIRE) studies, have shown that dofetilide is effective in conversion of atrial fibrillation or atrial flutter to sinus rhythm, although it appears to be more effective in conversion of atrial flutter than atrial fibrillation [69]. On the cellular level, dofetilide blocks a specific potassium current, thus prolonging the duration of the cardiac action potential and effective refractory period. Prolonging the action potential and effective refractory period increases the likelihood that the entry atrial impulses will encounter a refractory period when the cardiac cells are unable to accept another electrical impulse, and the arrhythmia will break. Because dofetilide does not slow conduction velocity, the PR and QRS intervals remain normal. It also does not cause hypotension or bradycardia. The major proarrhythmia associated with dofetilide administration is torsades de pointes due to prolongation of the QT interval. The degree of risk is related to the dosage and serum concentration of dofetilide. The higher the dose (or the higher serum concentration), the higher the risk that proarrhythmias will develop. Other proarrhythmias seen with dofetilide administration include premature ventricular contractions, broad complex ventricular tachycardia, nonsustained ventricular tachycardia, and PSVT. Following oral administration, dofetilide is almost completely absorbed; it is primarily excreted by the kidneys [33].
The administration of dofetilide is very heavily regulated by the FDA. Only approved centers and physicians who have completed required educational programming on the initiation of dofetilide may prescribe dofetilide. Physicians and centers initiating dofetilide therapy are also required to provide the patient with specific educational information [33]. This includes information on the action of the medication, its side effects, and how to obtain and take the medication. An educational kit containing a videotape, written information, and prescribing information for the patient to give to other physicians is provided to the patient. Because of the restrictions on dofetilide, only selected pharmacies may dispense the medication. The patient may be unable to obtain dofetilide from his/her usual outpatient pharmacy. At the time of discharge, the patient will be provided with a small amount of dofetilide at the prescribed dose. He/she will then receive a larger quantity of dofetilide in the mail from an approved pharmacy [74]. Dofetilide must be initiated in the hospital setting where continuous ECG monitoring and emergency resuscitation equipment is available [28,74]. Prior to administration, the patient's baseline QTc and creatinine clearance must be assessed. If the patient's baseline QTc exceeds 440 msec (or 500 msec if ventricular conduction abnormalities), dofetilide is contraindicated. The initial dose is determined by the patient's initial creatinine clearance [33]. A detailed algorithm is provided in the dispensing information to assist the physician and pharmacologist in determining the appropriate dosage. If the patient's renal function is severely impaired, dofetilide is again contraindicated.
For persons with normal renal function, studies have shown that an oral dose of 500 mcg twice daily is effective in restoring normal sinus rhythm. In the presence of impaired renal function, the dose should be reduced. The dose may be as low as 125 mcg twice daily. The usual range for the maintenance dose (normal renal function) is 125–500 mcg twice daily. The administration protocol is as follows [33]:
Admit the patient to an inpatient facility approved for dofetilide administration.
Antiarrhythmic medications associated with prolonged QT interval (primarily Class I, Class III) should be discontinued; the guideline is at least three or more half-lives before initiation of dofetilide. Digoxin, beta blockers, and calcium channel blockers may be used to control ventricular rate during the withdrawal period of these drugs.
Electrolyte imbalances, especially potassium and magnesium, should be corrected before therapy is initiated.
QTc should be monitored periodically. Dosage should be reduced if QTc increases by more than 15% or exceeds 500 msec within two to three hours after initial dose. See the package labeling or website information for specific dosage reduction guidelines.
After the second dose, if the QTc interval is greater than 500 msec (or 550 msec in the presence of ventricular conduction abnormalities), dofetilide should be discontinued.
Continue ECG monitoring for a minimum of three days.
An overdose of dofetilide results in a dangerously prolonged QT interval. Emergency measures include isoproterenol infusion and external noninvasive cardiac pacing. If torsades de pointes develops, IV magnesium sulfate is the treatment of choice [74].
Amiodarone has received increasing attention for its ability to convert atrial fibrillation to normal sinus rhythm and to prevent atrial fibrillation in patients undergoing CABG surgery [54,57,75]. Categorized as a Class III antiarrhythmic, amiodarone has properties of all four classes. It inhibits conduction through the AV node, prolongs the action potential and refractory period, and inhibits adrenergic stimulation. It may be safely used for patients with congestive heart failure, coronary artery disease, and persons with accessory pathway conduction. The proarrhythmic effects associated with amiodarone include bradycardia, heart block, ventricular fibrillation, and ventricular tachycardias including torsades de pointes. Hypotension may occur with IV administration. Amiodarone is associated with multiple severe side effects and toxic effects. These include pulmonary fibrosis, impaired vision from corneal deposits, photosensitive skin, thyroid dysfunction, and liver dysfunction [33,76]. Prior to beginning amiodarone therapy, the physician should obtain baseline data. Appropriate data includes a chest x-ray, pulmonary function tests, thyroid function tests, liver function tests, and renal studies. Patients receiving amiodarone therapy should be monitored for development of toxic effects. Serious toxicity, including death due to bradycardia ending in cardiac arrest, has been reported [33]. If symptoms develop, amiodarone should be discontinued. Use of the lowest effective maintenance dose is highly recommended due to the multitude and severity of side effects associated with amiodarone therapy. The FDA has issued a warning regarding concurrent use of amiodarone and simvastatin [77]. In patients who are taking both simvastatin and amiodarone, the dose of simvastatin should not exceed 20 mg/day [33,73].
The usual initial dose of amiodarone is 150 mg over 10 minutes, then 1 mg/minute for six hours, then 0.5 mg/minute for 18 hours or 600–800 mg/day oral in divided doses up to 10 g/day [33]. When a cumulative dose of 10 g is reached, a maintenance dosage of 200–400 mg/day is begun. For elderly patients, dosing should be initiated at the lower end of the adult dosage range, and the maintenance dose is usually 100 mg/day. Elderly persons clear amiodarone more slowly [33,54,57].
Propafenone, a Class Ic antiarrhythmic, slows conduction by changing normal ion transportation across cardiac cell membranes. Studies show it may also have Class II antiarrhythmic effects [78]. It may be used for the conversion of paroxysmal atrial fibrillation to sinus rhythm. For an adult weighing 70 kg or more, an initial dose of 600 mg orally is given, followed by a maintenance oral dose of 150–300 mg every eight hours [33]. Propafenone has less risk of torsades de pointes than other antiarrhythmic agents because it does not prolong the QT interval; however, it is still associated with the development of bradycardia, heart block, and signs of congestive heart failure. For this reason, it should not be prescribed for patients immediately following acute myocardial infarction. Other common side effects include nausea, anorexia, constipation, and headache [33]. One case of a severe drug-drug interaction with mirtazapine leading to propafenone toxicity has been reported [79].
Procainamide, a Class Ia antiarrhythmic, has been used for management of atrial arrhythmias for many years, although it may be less useful than some other agents [28]. It increases both atrial and ventricular refractory periods. It can convert atrial fibrillation to normal sinus rhythm and maintain normal sinus rhythm following conversion. Depending on a patient's status, a loading dose may be administered intravenously or orally. Extended-release forms of oral therapy should not be used for initiation of therapy. Procainamide can have proarrhythmic effects including bradycardia, a prolonged QT interval, and heart block. Worsening or refractory tachyarrhythmias can develop in the presence of procainamide toxicity. Serum levels should be carefully monitored. The therapeutic serum level of procainamide is 4–10 mcg/mL. Toxicity may develop at serum levels of more than 10 mcg/mL. For some patients, especially those with impaired renal function, the combined procainamide/N-acetylprocainamide (NAPA) level should be monitored. NAPA is an active metabolite of procainamide that has antiarrhythmic properties. The combined procainamide/NAPA serum level should not exceed 30 mcg/mL [33].
Quinidine, another Class Ia antiarrhythmic, prolongs the effective refractory period and increases conduction time. It is effective in converting atrial fibrillation to normal sinus rhythm and in maintaining sinus rhythm following conversion. Because quinidine also decreases vagal tone, thereby facilitating conduction across the AV node, it does not slow ventricular rate. It is indicated for use in patients with controlled atrial fibrillation, usually after digoxin or verapamil has been given. Patients who are in uncontrolled atrial fibrillation should receive other antiarrhythmic agents prior to starting quinidine. Although quinidine comes in an IV form, IV administration is associated with a significant risk of severe hypotension, and use of IV quinidine is discouraged [33].
Flecainide is a Class Ic antiarrhythmic that acts by blocking sodium channels so that conduction through cardiac cells is slowed. Flecainide is only administered orally. Flecainide should not be prescribed for patients in the immediate post-myocardial infarction period. It should be used cautiously in patients with congestive heart failure, conduction defects, and impaired renal function [33]. It is a drug of choice for persons with paroxysmal atrial fibrillation [5,12,13,14,19,20,37,46,68].
Direct-current cardioversion involves the delivery of an electrical current that is synchronized to the QRS complexes. Synchronization is necessary to avoid inducing ventricular fibrillation that can occur when a shock is delivered during ventricular repolarization. It is important to differentiate between a cardioversion in which sinus rhythm is not restored, even transiently, and a cardioversion in which sinus rhythm is restored but atrial fibrillation recurs. When sinus rhythm is not restored, approaches that improve energy delivery and allow for successful cardioversion (e.g., increasing shock strength, delivering a biphasic rather than monophasic waveform) should be employed. When sinus rhythm is restored but atrial fibrillation returns, pretreatment with selected antiarrhythmic drugs may increase the likelihood of maintenance of sinus rhythm [28]. The success rate of electrical cardioversion exceeds 75% in patients with atrial fibrillation of relatively short duration in whom the left atrium is not significantly large [37].
Electrical cardioversion has been found to be an effective and safe method for restoring normal sinus rhythm in a number of patients. It is the treatment of choice for persons with hemodynamically unstable atrial fibrillation [28]. Electrical cardioversion is also indicated for [28,40]:
Persons for whom there is a reasonable expectation that normal sinus rhythm can be restored and maintained
Persons who require "atrial kick" to relieve incapacitating or unpleasant symptoms, improve exercise tolerance, and increase their ability to perform their usual daily activities
Persons who would benefit from normal sinus rhythm but who have not been able to be successfully cardioverted pharmacologically (i.e., "failed" pharmacologic cardioversion)
Persons who have severe dyspnea or chest pain with atrial fibrillation or who have pre-excited atrial fibrillation should undergo urgent cardioversion [37].
It is not indicated for prevention of subsequent episodes [80]. Cardioversion of atrial fibrillation and subsequent maintenance of sinus rhythm are more likely to be successful when the duration of atrial fibrillation is less than six months [28]. Because electrical cardioversion carries the risk of thromboembolic complications, it generally should be performed when the patient is adequately anticoagulated. Results of observational studies suggest that thromboembolic risk after cardioversion is highest in the first 72 hours and that the majority of events occur within 10 days [28]. Cardioversion may be performed without first anticoagulating the patient only when he/she is hemodynamically unstable and requires immediate intervention, when the patient has been in atrial fibrillation less than 48 hours, or when the absence of an atrial thrombus has been confirmed by TEE [5,20,28,47,80,81].
Appropriate anticoagulation management around the time of cardioversion is essential for reducing thromboembolic risk. Results of observational studies suggest that thromboembolic risk after cardioversion is highest in the first 72 hours and that the majority of events occur within 10 days [82]. As indicated, anticoagulation before cardioversion is required for most patients. Warfarin should be initiated, and the dose adjusted to reach and maintain a target goal of an international normalized ratio (INR) of 2.5 (range: 2.0 to 3.0). After the patient has been maintained for three weeks at that therapeutic goal, cardioversion may be performed. Following cardioversion, anticoagulation should be maintained for four weeks [28,40].
TEE guidance is an alternative to three weeks of anticoagulation before cardioversion. Therapeutic anticoagulation is achieved and followed by TEE. If no thrombus is seen, cardioversion is performed and anticoagulation is continued for four or more weeks. The absence of left arterial thrombus on TEE does not preclude the need for anticoagulation during and after cardioversion [28,37]. Alternative strategies for achieving rapid anticoagulation include administration of low-molecular-weight heparin or a new oral anticoagulant. If a thrombus is identified on TEE, cardioversion should be postponed, followed by three to four weeks of anticoagulation. Repeat TEE to ensure thrombus resolution is an option before attempting another cardioversion. If a thrombus remains on repeat TEE, an alternative strategy (e.g., rate control plus appropriate anticoagulation) may be considered [28]. TEE is a good predictor of acute risk. If no thrombus is seen in the cardiac chambers, particularly the left atrial appendage, and dense spontaneous echo contrast is not seen, cardioversion has low acute risk of stroke. Effective anticoagulation in patients with atrial fibrillation reduces the risk of stroke three-fold after four to six weeks [37]. Data on cardioversion risks for atrial flutter are limited. However, because atrial flutter can be associated with thrombi and episodes of atrial fibrillation, it is recommended that the anticoagulation management strategy for cardioversion of atrial flutter be the same as that for atrial fibrillation [28].
Prior to the procedure, the patient should be carefully assessed. Serum electrolytes and serum drug levels of medications such as digoxin should be checked. Electrolyte imbalances should be corrected. The administration of IV electrolytes has been found to increase the success rate of cardioversion in patients with persistent atrial fibrillation [83]. Testing for elevated C-reactive protein levels may predict the recurrence of atrial fibrillation following cardioversion [84,85,86,87]. Cardioversion should not be performed if the patient has digitalis toxicity. A baseline 12-lead ECG should be obtained. Oral antiarrhythmic medications, such as oral amiodarone or sotalol, may be started prior to the cardioversion. In some patients, this will facilitate conversion to normal sinus rhythm and maintenance of sinus rhythm following the procedure. The patient should be adequately sedated with a short-acting agent (e.g., midazolam, propofol), and an opioid analgesic, such as fentanyl, is commonly used. Reversal agents (e.g., flumazenil, naloxone) should be available [81]. The risks of the procedure should be explained to the patient and family. Common risks include the problems associated with moderate sedation, skin burns, and the development of proarrhythmias [37,81]. The procedure should be explained briefly to patients. Consider including these points:
An IV access will be established.
The patient will be "nothing by mouth" (NPO) for several hours prior to the procedure.
The patient's ECG, blood pressure, and oxygen saturation levels will be continuously monitored before, during, and following the procedure.
The patient will be sedated or general anesthesia will be used.
Potentially life-threatening postprocedure events may occur, including the induction of ventricular tachycardia/fibrillation, asystole, and transient depression of myocardial function. Techniques to handle these situations should be readily available to prevent complications [80,81].
A variety of commercially available external cardioverters are available for external electrical cardioversion. The physician in charge of the procedure should be thoroughly familiar with the chosen device [66,80]. ECG leads are placed on the patient. The cardioverter delivers a programmed shock in synchronization with the patient's own QRS. Synchronization decreases the risk that the patient will go into ventricular fibrillation from the electrical shock. The initial shock may be a low voltage. If unsuccessful, the voltage will be increased. Following completion of the procedure, the patient will be monitored until he/she is recovered from the anesthesia/sedation. As noted, follow-up care includes oral antiarrhythmic therapy and oral anticoagulation with warfarin sodium [80]. In patients for whom external cardioversion is unsuccessful, an internal shock with electrode catheters has been shown to be successful [80,88,89].
For patients in atrial fibrillation, restoration of normal sinus rhythm may occur spontaneously or through electrical or pharmacologic cardioversion. Regardless of the mechanism of conversion, antiarrhythmic therapy is usually indicated to maintain sinus rhythm (Table 8). Some reversion to atrial fibrillation is likely to occur despite optimal antiarrhythmic therapy. However, some patients may benefit from therapy that restores sinus rhythm for prolonged periods [28]. The effectiveness of antiarrhythmic therapy in maintaining normal sinus rhythm should be based on an evaluation of the severity and duration of episodes and not on their occurrence. The following are general principles for initiating drug therapy for maintenance of normal sinus rhythm [28,54,83]:
Selected medications should be given initially in low doses and increased as needed. Closely monitor the patient for therapeutic effect/desired effect and side effects.
To prevent drug interactions, closely monitor the levels and effectiveness of other agents.
For persons with paroxysmal atrial fibrillation, first consider the use of flecainide, propafenone, and sotalol.
If treatment with a single medication is ineffective, combination therapy may be tried. Effective combinations include use of a beta blocker, sotalol or amiodarone, and a Class Ic medication.
Closely monitor the patient for widening QT intervals.
Counsel the patient to avoid the concurrent use of noncardiac medications that can prolong the QT interval.
ANTIARRHYTHMIC MEDICATIONS USED TO MAINTAIN SINUS RHYTHM
| Agent | Class | Action | Dosage/Route | Side Effects | Comments | ||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Quinidine | Ia |
|
|
|
| ||||||||||||||||||||||||||||
| Disopyramidea | Ia |
|
|
| Monitor patient's QT interval | ||||||||||||||||||||||||||||
| Flecainide | Ic |
|
|
|
| ||||||||||||||||||||||||||||
| Propafenone | Ic |
| Maintenance oral dose: 150–300 mg three times daily |
|
| ||||||||||||||||||||||||||||
| Sotalol | II with Class III properties |
|
|
|
| ||||||||||||||||||||||||||||
| Amiodaronea | III |
|
|
|
| ||||||||||||||||||||||||||||
| Dofetilide | III |
|
|
|
| ||||||||||||||||||||||||||||
| Dronedarone | III |
| Usual oral dose: 400 mg twice daily |
|
| ||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||
Oral antiarrhythmic medications found to be effective in maintaining normal sinus rhythm include quinidine, disopyramide, flecainide, propafenone, sotalol, amiodarone, dofetilide, and dronedarone. However, pharmacologic therapy should be abandoned if symptomatic improvement is not achieved or if the patient experiences any adverse effects [49,90,91]. In addition to possible adverse effects, some antiarrhythmic medications (i.e., disopyramide, quinidine, and sotalol) may increase mortality. Possible benefits on clinically relevant outcomes (e.g., stroke, embolism, heart failure) remain to be established [75].
Quinidine is available in different salts as quinidine sulfate or quinidine gluconate. Its use in patients with paroxysmal atrial fibrillation has not been extensively evaluated, although it appears to be as effective as Class Ic agents. It has been shown to significantly reduce the recurrence of atrial fibrillation [75]. Quinidine can be associated with severe gastrointestinal (GI) side effects, including nausea and diarrhea. Development of proarrhythmia is a concern [33]. The medication should be administered with food or milk to decrease GI effects [33]. If severe GI side effects persist, the type of preparation may be changed (i.e., from gluconate to sulfate or vice versa).
Disopyramide may be administered in a short- or sustained-release form. Because it prolongs the QT interval, it is not indicated as a first drug of choice for persons who also have hypertension. The combination of left ventricular hypertrophy caused by long-standing hypertension and a prolonged QT interval greatly increases the risk of proarrhythmias such as torsades de pointes [33].
Flecainide is the drug of choice for the treatment of atrial fibrillation that has no identifiable cause. It is recommended for use only in the absence of structural heart disease and should not be prescribed for patients who have had a recent myocardial infarction or have abnormal left ventricular function [33].
Propafenone is an effective antiarrhythmic for persons who also have hypertension because it does not prolong the QT interval. Studies suggest it reduces the recurrence of atrial fibrillation [75]. It should not be prescribed for patients immediately following acute myocardial infarction [33].
Sotalol has been gaining popularity in the management of atrial fibrillation. It has both Class II (beta adrenergic blocking) and Class III properties. It slows the heart rate, decreases conduction through the AV node, increases AV node refractory period, and prolongs the cardiac action potential. It has been found to be effective in maintaining normal sinus rhythm. Administered orally, the initial dose for the person with normal renal function is 80 mg twice daily. This dose may be gradually increased over a period of days to a maximum of 640 mg total daily dose. The usual dose is 80–160 mg twice daily. Dosage should be reduced in the presence of renal impairment [33]. For persons undergoing electrical cardioversion, sotalol may be started prior to the procedure to facilitate cardioversion and continued maintenance of sinus rhythm. The manufacturer of the proprietary form of sotalol warns that only one preparation has been labeled for use in atrial fibrillation. See the package insert for additional information [92]. Because it prolongs the QT interval, sotalol has a proarrhythmic effect; arrhythmias associated include torsades de pointes, other forms of ventricular tachycardia, ventricular fibrillation, bradycardia, and heart block. Hypotension and signs of congestive heart failure may occur. Increased risk of all-cause mortality has been suggested [75]. Hypokalemia and hypomagnesemia increase the risk of proarrhythmic effects. Torsades de pointes has been associated with doses in excess of 320 mg/day [33]. The manufacturer recommends that sotalol be initiated in a hospital setting with continuous ECG monitoring. The facility must be equipped with cardiac resuscitation equipment/staff. ECG monitoring is recommended to continue for three days when the patient is on a maintenance dose [33].
Amiodarone is a drug of choice to maintain normal sinus rhythm in patients with congestive heart failure. Studies suggest it reduces the recurrence of atrial fibrillation [75]. It has the added benefit of providing effective rate control, thus eliminating the need for other drugs to control rate. It is a secondary or last resort choice to maintain sinus rhythm in persons with coronary artery disease. Because of the multiple side effects and toxicities of amiodarone, persons receiving it should be monitored periodically, and the lowest effective maintenance dose should be used [33].
Dofetilide may be used for maintenance of normal sinus rhythm. As described, dofetilide therapy must be initiated in an approved hospital by medical practitioners who are approved to initiate and prescribe dofetilide therapy. Evaluation for use of this drug in the elderly is imperative [12,14,19,33,34,46,47,53,54].
Dronedarone is among several new drugs developed for the management of atrial fibrillation. It received FDA approval in 2009 for the management of atrial fibrillation and atrial flutter. Dronedarone shares many antiarrhythmic properties with amiodarone but has a more favorable safety profile and fewer adverse effects. Its use is contraindicated in patients with severe heart failure requiring recent hospitalization [28,33,92,93,94,95,96]. Dronedarone may be considered in the management of patients with paroxysmal atrial fibrillation or after conversion of persistent atrial fibrillation [28]. It should not be used for rate control in permanent atrial fibrillation [28]. Dronedarone may be used for the prevention of recurrent atrial fibrillation [49,75]. In addition, this medication may be initiated in the outpatient setting [28]. It is important to note that the FDA issued a drug safety announcement about cases of rare, but severe liver injury, in patients being treated with dronedarone. The risk of injury has been added to labeling for the drug [97].
The ACC/AHA/ESC Task Force for management of patients with atrial fibrillation has suggested that outpatient maintenance of sinus rhythm, the "pill-in-the-pocket" approach, shows promise. This approach allows for intermittent (rather than daily) administration of oral antiarrhythmic medication as an acceptable treatment option for patients with sporadic episodes of atrial fibrillation. It is not recommended for patients with daily episodes [28]. Self-administration of oral antiarrhythmic drugs improves the patient's quality of life, decreases overall hospital admissions, and reduces treatment costs. Class Ic drugs, such as propafenone and flecainide, are recommended for their efficacy, rapid action, and safety (i.e., no organ toxicity and low incidence of proarrhythmia). They are not recommended for patients with underlying structural heart disease [6,28,91].
Atrial fibrillation has been identified as the most common disorder leading to systemic embolization [5,98,99]. Remember that in atrial fibrillation, the atria merely "quiver." They never fully contract to expel all of the blood from the chambers into the ventricles. The blood that remains in the atria becomes stagnant, allowing clots to form. A thrombus (clot) is most likely to form in the left atrium. Soft, friable fragments of the clot may break off and flow into the ventricle, where they are ejected into the systemic or pulmonary circulation. The most common thromboembolic event linked to atrial fibrillation is the development of a CVA. The statistics are alarming. For example, atrial fibrillation is associated with a four- to fivefold increased risk of stroke and causes an estimated one in seven strokes [1]. The overall mortality rate associated with CVAs is significant. Up to 20% of persons who have a CVA may die within the first year, and one-quarter to one-half of all who survive experience permanent neurologic damage resulting in partial or total loss of independence and activities of daily living [75,100]. The associated direct and indirect costs are high [100]. Persons with atrial fibrillation are at increased risk for CVA if they have one or more of the following risk factors: advanced age, history of previous CVA, history of transient ischemic attacks (TIAs), history of previous systemic embolism, history of left ventricular dysfunction, heart failure, diabetes mellitus, or hypertension [7,101,102].
National recommendations are to anticoagulate persons with atrial fibrillation. Persons who should be anticoagulated include [28,40,45]:
Persons who fail pharmacologic or electrical cardioversion and remain in atrial fibrillation
Persons who experience permanent/persistent/chronic atrial fibrillation
Persons who have converted to normal sinus rhythm but have recurrence of atrial fibrillation
Despite the existence of national recommendations to anticoagulate patients with atrial fibrillation, a systematic review revealed that less than 70% of eligible patients receive oral anticoagulation treatment, including those at highest risk [103]. Another review of anticoagulation therapy in patients with high-risk atrial fibrillation before admission for stroke revealed that 29% were not receiving any anticoagulation therapy, 31% were prescribed antiplatelet therapy, and only about one-fourth of the 39% receiving warfarin achieved therapeutic INR levels [104].
The specific type of therapy recommended depends on an assessment of the patient's level of risk to develop thromboembolic complications, irrespective of the pattern of atrial fibrillation [28,45,49]. Stroke-risk stratification schemes for patients with atrial fibrillation were developed in the late 1990s and later refined and validated in large population studies [105,106,107,108,109]. The CHADS2 score (congestive heart failure, hypertension, age ≥75 years, diabetes mellitus, stroke [double weight]), first published in 2001, was developed to predict the risk of stroke in patients with nonrheumatic atrial fibrillation [106]. It was derived by combining risk factors from prior studies and then testing their validity in a cohort of 1,773 Medicare-aged patients over 2,121 patient years [105; 110]. The CHADS2 score was found to be limited by the non-inclusion of common stroke risk factors and was subsequently expanded to include three additional independent risk factors: vascular disease, age 65 to 74 years, and female sex [111,112,113]. The new, more inclusive scoring system is known as the CHA2DS2-VASc score (Table 9). It has been widely used since 2010 [48,114].
CHA2DS2-VASc SCORING SYSTEM FOR ATRIAL FIBRILLATION STROKE RISK
| Age | <65 years (0 points) | 65–74 years (1 point) | ≥75 years (2 points) | |||
| Sex | Female (1 point) | Male (0 points) | ||||
| CHF History | No (0 points) | Yes (1 point) | ||||
| Hypertension History | No (0 points) | Yes (1 point) | ||||
| Stroke/TIA/Thromboembolism History | No (0 points) | Yes (2 points) | ||||
| Vascular Disease Historya | No (0 points) | Yes (1 point) | ||||
| Diabetes History | No (0 points) | Yes (1 point) | ||||
| ||||||
Note: Adjusted stroke rate scores (Table 10) are based on data from Lip and colleagues [109,115,116,117]. The actual rates of stroke in contemporary cohorts may vary from these estimates.
Generally, a score of 0 indicates that no treatment is needed. A score of 1 indicates either no treatment or treatment with aspirin or an oral anticoagulant may be considered [28]. A score of 2 or greater in men or 3 or greater in women indicates treatment with an oral anticoagulant. Anticoagulant agents routinely used for the prevention of thromboembolism in patients with nonvalvular atrial fibrillation include warfarin, direct thrombin inhibitors (e.g., dabigatran), factor Xa inhibitors (e.g., rivaroxaban, apixaban, edoxaban) (also referred to as direct-acting oral anticoagulants or DOACs), and antiplatelet drugs (i.e., aspirin and clopidogrel). The use of antiplatelets is a class II recommendation for patients with atrial fibrillation who are at increased risk of stroke and who are being treated for acute coronary syndrome [40]. Although anticoagulants have been effective in reducing ischemic stroke in multiple randomized controlled trials, their use is associated with an increased risk of bleeding, ranging from minor bleeding to fatal intracranial or extracranial hemorrhage. Platelet inhibitors (alone or in combination) are less effective than warfarin, are better tolerated by some patients, and are associated with a lower risk of intracerebral hemorrhage. However, they have similar overall rates of major bleeding in some studies. Careful consideration is required to balance the benefits and risks of bleeding in each individual patient [28,40]. The AHA/ACC/HRS class I recommendations for risk-based anticoagulant therapy are summarized in Table 11 [40].
AHA/ACC/HRS CLASS I RECOMMENDATIONS FORSELECTING AN ANTICOAGULANT REGIMEN
| ||||||
| AF = atrial fibrillation, OACs = oral anticoagulants, DOAC = direct oral anticoagulant, INR = international normalized ratio. |
Two medications used commonly in prevention of thromboembolic events are aspirin and warfarin. They may be used singly or in combination to prevent thromboembolic events, but the efficacy of combination therapy has not been established [119,120,121,122]. Warfarin in comparison to aspirin leads to a 39% relative risk reduction in stroke [123]. Rather than adding aspirin, the AHA/ACC/HRS Task Force recommends increasing the intensity of the anticoagulant to a maximum target INR of 2.0–3.0 [28]. Aspirin acts by decreasing platelet aggregation. Because it offers only modest protection against stroke for patients with atrial fibrillation, its use may be considered for low-risk patients [28,49]. As noted, low-risk patients include those who are younger than 65 years of age and have no underlying cardiac disease. It may also be recommended for use in patients, particularly elderly persons, who cannot safely take warfarin. The usual adult dose of aspirin is 81–325 mg oral per day [49].
Warfarin is recommended for patients at high risk to develop thromboembolic events. It acts by inhibiting the synthesis of clotting factors II, VII, IX, and X that are dependent on vitamin K. Once warfarin therapy is initiated, it can take four to five days to achieve a therapeutic level. Effectiveness of warfarin therapy is evaluated by monitoring the patient's prothrombin time (PT) with the INR. The usual target level for the INR is 2.0–3.0 (target of 2.5) [20,49]. Some clinicians recommend using the lower end of that range for elderly patients. The risk of serious bleeding complications is greater in persons older than 75 years of age. Initially the PT/INR should be monitored at least weekly. Once the therapeutic goal is achieved, the monitoring may be reduced to monthly [40]. Drug-drug and food-drug interactions may play a significant role in maintaining a stable INR level for persons taking warfarin. Drugs that may impact warfarin effectiveness and INR levels include many anti-infectives and amiodarone. Food interactions include vitamin K containing foods that can antagonize the action of warfarin. Herbal products and nutritional supplements may contain components that can increase or decrease the effectiveness of warfarin [12,14,124,125].
For patients to take warfarin safely and correctly, they should receive appropriate patient education when the medication is initiated. See Table 12 for a summary of content to include.
WARFARIN PATIENT EDUCATION
| Topic | Content | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Purpose, action of warfarin |
| ||||||||||||||||
| How to take warfarin |
| ||||||||||||||||
| Follow-up care |
| ||||||||||||||||
| Precautions: other medications |
| ||||||||||||||||
| Precautions: diet |
| ||||||||||||||||
| Precautions: measures to reduce risk of bleeding |
| ||||||||||||||||
| Signs and symptoms to report |
| ||||||||||||||||
| Emergency care for cuts |
|
In some cases, warfarin may be considered unsuitable due to patient preference or the physician's assessment of the patient's ability to safely sustain anticoagulation. In these patients, the addition of clopidogrel to aspirin to reduce the risk of major vascular events, including stroke, might be considered in patients with atrial fibrillation [49]. Aspirin as monotherapy for stroke prevention is not recommended [28,40].
Several DOAC alternatives to warfarin have emerged, including the direct thrombin inhibitor, dabigatran, and the factor Xa inhibitors rivaroxaban, apixaban, and edoxaban. The DOACs represent an advance in therapeutic safety and reduced intracranial bleeding as compared with warfarin, including no need for regular monitoring, faster onset of action, and potentially fewer adverse interactions [40,127]. As an alternative to warfarin, the 2019 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation recommends oral anticoagulation with one of these newer agents over warfarin for patients with nonvalvular atrial fibrillation or atrial flutter with prior stroke, transient ischemic attack, or significant stroke risk [40].
Dabigatran
Dabigatran etexilate mesylate (Pradaxa) is currently the only direct thrombin inhibitor approved by the FDA to reduce the risk of stroke and systemic embolism in patients with nonvalvular atrial fibrillation [28,33]. The RE-LY (Randomized Evaluation of Long-Term Anticoagulation Therapy) trial compared dabigatran (110 mg or 150 mg twice daily) with adjusted-dose warfarin in 18,113 patients over a median follow-up of two years [128]. The risk of hemorrhagic stroke was significantly (74%) lower with both doses of dabigatran compared with warfarin. Major bleeding was significantly decreased with the 110-mg dose of dabigatran but not with the 150-mg dose. Both doses had lower rates of intracranial bleeding and life-threatening bleeding but higher gastrointestinal bleeding in the 150-mg dose group. Results were similar for secondary stroke prevention [28].
Dabigatran is contraindicated in patients who have prosthetic heart valves and those who have hemodynamically significant valve disease, severe renal failure, or advanced liver disease [33,129]. Dabigatran acts by inhibiting the synthesis of clotting factors V, VIII, XI, and XIII. The most common complication is bleeding; patients should be monitored for signs and symptoms of bleeding. Risk factors include concurrent use of drugs that increase the risk of bleeding (e.g., heparin). Idarucizumab is recommended for the reversal of dabigatran in the event of life-threatening bleeding or an urgent procedure [40]. Dabigatran is also associated with a significantly elevated risk of myocardial infarction or acute coronary syndrome [130]. The usual adult dose is 150 mg twice daily [33,131].
The factor Xa inhibitors have a unique mechanism of action compared with warfarin. Factor Xa is common to both the intrinsic and extrinsic pathways of the clotting cascade making it an excellent target for anticoagulation therapy. It plays a significant role in the formation of thrombin from prothrombin. Inhibition of Xa leads to a significant reduction in thrombin and ultimately clot formation [132]. All of the currently available factor Xa inhibitors are contraindicated for use in patients experiencing active bleeding. The most serious bleeding event is intracranial hemorrhage. Patients with atrial fibrillation should be assessed for bleeding risk using the HAS-BLED (hypertension, abnormal renal/liver function, stroke, bleeding history, labile INR, elderly, drugs/alcohol concomitant) risk score [28,132]. Additionally, all of the factor Xa inhibitors carry a black-box warning advising that premature discontinuation leads to increased risk for ischemic events. There are no currently approved antidotes for reversal of these agents [33,132].
Rivaroxaban
Rivaroxaban (Xarelto) is a factor Xa inhibitor approved for prevention of stroke and systemic embolism in patients with atrial fibrillation. Rivaroxaban 20 mg once daily was compared with warfarin among 14,264 high-risk patients with atrial fibrillation [133]. Major bleeding was similar for rivaroxaban and warfarin, but fewer cases of fatal bleeding and intracranial hemorrhage were found for rivaroxaban. The risk of stroke was similar for both drugs. Bleeding is the most common complication with rivaroxaban. Major hemorrhages (e.g., intracranial, gastrointestinal, retinal, epidural, hematoma, adrenal bleeding) have been reported. Patients at increased risk of bleeding include those with congenital or acquired bleeding disorders, recent stroke, severe uncontrolled hypertension, renal impairment, advanced age, and/or concomitant use of drugs that affect hemostasis. The patient's renal function and CBC should be evaluated prior to initiation of rivaroxaban [33]. Rivaroxaban is dosed at 20 mg once daily with the evening meal [33].
Apixaban
Apixaban (Eliquis) 2.5 mg twice daily was compared with warfarin in a double-blind randomized controlled trial of 18,201 patients with atrial fibrillation and two or more of the following conditions: age 80 years or older, weight ≤60 kg, or a serum creatinine level ≥1.5 mg/dL [134]. Patients were followed for a mean of 1.8 years. Apixaban was significantly better than warfarin, with fewer overall strokes, systemic emboli, and major bleeding events, but gastrointestinal bleeding complications were similar between apixaban and warfarin. Patients treated with apixaban had fewer deaths than those on warfarin. The benefit of apixaban was independent of type of atrial fibrillation, risk profile, CHA2DS2-VASc score, and whether the patient had a history of prior stroke [134].
Apixaban is indicated for patients with nonvalvular atrial fibrillation to reduce the risk of stroke and systemic embolism [33].The most common complication is bleeding; patients should be monitored for signs and symptoms of bleeding. Risk factors include concurrent use of drugs that increase the risk of bleeding (e.g., nonsteroidal anti-inflammatory drugs). Hepatic function also should be monitored [33,40]. The usual adult dose is 5 mg twice daily [33].
Rivaroxaban or apixaban also may be used for three weeks prior to and four weeks after cardioversion in patients with atrial fibrillation or atrial flutter of 48 hours or more duration or when the duration is unknown [28,35,40].
Edoxaban
Edoxaban (Savaysa) is another factor Xa inhibitor approved for the prevention of thromboembolism in patients with nonvalvular atrial fibrillation. Edoxaban was approved in 2015 on the basis of a double-blind randomized trial of 21,105 patients with nonvalvular atrial fibrillation [135]. Participants were randomized to high-dose edoxaban (60 mg daily), low-dose edoxaban (30 mg daily), or warfarin; creatinine clearance up to 30 mL/min was an exclusion criterion. Edoxaban was found to be noninferior to warfarin with regard to stroke prevention or thromboembolic complications. It also was associated with significantly lower rates of bleeding and death from cardiovascular causes [135]. In patients with upper-range creatinine clearance (95 mL/min or greater), the hazard ratios for developing embolic events were similar between the high-dose edoxaban and warfarin groups [135]. Consequently, the FDA does not recommend edoxaban for patients with end-stage renal disease or for those on dialysis [40,135]. The usual adult dose is 60 mg once daily [33].
Radiofrequency ablation of the AV node is an interventional therapy commonly used in the management of atrial fibrillation. The relative safety of radiofrequency energy has contributed to the widespread adoption of this technique as a therapeutic modality for atrial fibrillation [136,137]. Radiofrequency ablation has been found to be effective for persons who have significant symptoms with atrial fibrillation and/or poorly controlled ventricular rate who also [19,40,49,58,138,139]:
Have remained in atrial fibrillation despite attempts at electrical or pharmacologic cardioversion or who quickly revert to atrial fibrillation following cardioversion (referred to as "failed cardioversion")
Cannot take antiarrhythmic medications because of severe side effects or the development of proarrhythmias
Have inadequate rate control despite optimal dosing of appropriate antiarrhythmic agents
It is indicated for atrial fibrillation with lifestyle-impairing symptoms and inefficacy or intolerance of at least one antiarrhythmic agent [28,140]. Radiofrequency ablation is performed in the electrophysiology lab. See Table 13 for additional details about electrophysiology procedures. To ablate the AV node, radiofrequency waves are sent through catheters positioned at the AV node. Radiofrequency energy is electrical energy produced by a high frequency alternating current. As this current passes through cardiac tissue, it produces heat and creates a lesion in the AV node. The atria remain in atrial fibrillation, but no atrial impulses are conducted through the AV node to the ventricles. With AV node ablation, the patient's only effective ventricular rhythm is a junctional or ventricular escape rhythm. Because this rhythm is insufficient to meet the body's needs for cardiac output, a permanent pacemaker is inserted [19,137].
ELECTROPHYSIOLOGY TESTING AND ABLATION
| Electrophysiology testing is an invasive diagnostic cardiovascular procedure that can confirm and pinpoint the location of accessory conduction pathway(s) in the heart. It is performed in a specially equipped cardiac catheterization lab. Multiple catheters are introduced through the femoral vein into the right side of the heart. Each catheter contains 4 to 16 electrodes for monitoring the heart's electrical activity. The catheters are positioned in various locations in the heart; common sites include the high right atrium, the apex of the right ventricle, the AV junction/His bundle, and the coronary sinus. During the procedure, specific pacing protocols are used to determine the location and characteristics of any accessory pathways. Based on the location and characteristics of the accessory pathway(s), a treatment plan will be developed. Treatment options include medical management of the syndrome and associated arrhythmias and radiofrequency ablation of the accessory pathway(s). If the pathway is to be ablated, another catheter (the ablation catheter) is advanced to the site, and more extensive/precise mapping of the accessory pathway is done. The location of the ablation catheter is adjusted until it is close to the pathway. Radiofrequency energy waves are applied to the pathway until pre-excitation disappears and the tachyarrhythmia cannot be restarted. The procedure may last from three to five hours. Postprocedure care involves bedrest, frequent vital signs, and observing the femoral insertion sites for bleeding or hematoma formation. |
Radiofrequency ablation of the AV junction is the simplest procedure performed in patients with atrial fibrillation. AV nodal modification is less effective and is not frequently performed, except in an attempt to avoid pacemaker implantation. Both approaches are used to achieve good rate control, but unlike ablation techniques in atrial tissue, neither restores normal sinus rhythm. Few absolute contraindications to radiofrequency ablation exist. Left atrial ablation and ablation for persistent atrial flutter should not be performed in the presence of known atrial thrombus [137].
Catheter-based cryoablation was developed after radiofrequency ablation. Cryoablation utilizes tissue cooling to cause tissue necrosis. Low-intensity cooling (-10° C) allows assessment of lesion efficacy and safety, prior to delivering the deeper cooling (-70° C) that causes irreversible tissue necrosis. Cryoablation is not as versatile nor as widely used as radiofrequency ablation, but it is safer for ablation near the AV node [137].
No consensus exists on the optimal ablation technique, nor is there a consensus on what constitutes a clinically successful procedure. Data reveal that it is difficult to eliminate every episode of atrial fibrillation with catheter ablation. However, catheter ablation renders 90% of patients free from symptomatic atrial fibrillation and reduces its burden by more than 99% at one year of follow-up [141]. Single-procedure ablation is successful in 60% to 80% of optimal candidates, but many patients require repeat ablation [141]. The results of a study that compared radiofrequency ablation and two regimens of cryoballoon ablation resulted in no difference in one-year efficacy (53% by time to first recurrence) but greater than 98% burden reduction, as assessed by continuous cardiac rhythm monitoring [142]. A meaningful discussion about ablation success rates must include a definition of success that includes how intensively patient rhythms are monitored [141]. Despite the lack of consensus, ablation for atrial fibrillation is generally more effective than antiarrhythmic drug therapy, especially for those patients in whom pharmacotherapy has failed [139,143].
Prior to radiofrequency ablation of the AV node, the patient should receive information about radiofrequency ablation and permanent pacemaker insertion. Informed consent is obtained. Preprocedure evaluation should include a thorough history, physical examination, and a review ECG (12-lead if available). Laboratory studies should minimally include a complete blood cell count and an assessment of the patient's renal function and electrolyte levels. Other tests that may be indicated include exercise testing with or without cardiac imaging and cardiac catheterization [137]. The patient should be kept NPO for at least six hours prior to the procedure. Cardiac medications with electrophysiologic effects (e.g., beta-blockers, calcium channel blockers, digoxin) and Class I and III antiarrhythmic drugs should be tapered and/or discontinued. Warfarin is usually discontinued for at least a few doses preprocedure [137]. IV access should be established.
In the electrophysiology lab, the patient will be sedated, and continuous monitoring of blood pressure, heart rate and rhythm, and oxygen saturation initiated. Following the procedure, the patient's vital signs and oxygen saturation levels will be monitored closely. The patient's ECG will be monitored to evaluate proper pacemaker functioning. The sites used for insertion of the ablating catheters (usually the right and left femoral veins) will be monitored for signs of bleeding or hematoma formation. Depending on the size of catheters used, the patient may be on bed rest for four to six hours. During this time, the patient will need to keep his/her legs straight to decrease the risk of the bleeding from the catheter insertion sites. The pacemaker insertion pocket (often in the subclavian area) is monitored for signs of bleeding or excessive swelling. The head of the patient's bed is often elevated 30 degrees for 24 hours to maintain stable placement of the pacemaker leads.
Patients who have received pacemakers frequently have many questions and concerns. Careful discharge teaching and provision of written information can help to alleviate anxiety. General measures to cover in discharge teaching include [53,137]:
Check the incision daily for signs of infection or redness, tenderness, or drainage. Notify your physician if these develop.
Do not apply lotion or powder to the incision.
Do not lift more than 10 pounds (or as specified by your physician) for the first four weeks following implantation. Avoid excessive pushing or pulling.
Limit activity involving the affected arm for the length of time directed by your physician.
Always carry your pacemaker identification card with you.
Patients and their family members often have many questions about operating home, office, or industrial equipment. Pacemaker manufacturers provide detailed information in written booklets that should be given to the patient at the time the pacemaker is implanted.
Because the ectopic beats of atrial fibrillation can occur in various portions of the atrium, electrophysiology studies have been performed on many patients to determine the site or sites of the abnormal foci. The most common area of abnormal activity has been found to be in the vicinity of the pulmonary veins in the left atrium. This discovery led to the use of radiofrequency ablation of the pulmonary vein region as a cure for atrial fibrillation. It has even been suggested that the procedure could be used as a first-line approach to cure atrial fibrillation, because there is no need for long-term antiarrhythmic drug use. However, there is not yet a consensus on this approach as curative [137,144,145,146].
Pulmonary vein isolation is achieved in the electrophysiology lab, and a dose of radiofrequency energy is delivered to ablate the desired region. New energy sources such as laser, ultrasound, and cryothermia have also been used [147,148]. Multidimensional computed tomography (CT) and magnetic resonance angiography help visualize the anatomic landmarks necessary for ablation procedures and may also help prevent procedure-related complications [144,147,149]. Increasing evidence suggests that comprehensive evaluation of the left atrium using cardiac magnetic resonance imaging or CT has significant prognostic value for long-term outcomes [149,150]. Complications include fistulas, pseudoaneurysms, TIA, and cardiac tamponade. Pulmonary vein stenosis and stroke are rare, but serious, complications [80,144]. As with other ablation techniques, anticoagulation is initiated at the time of the procedure and continued for at least three months.
This procedure is suggested only for patients who have not responded to pharmacologic therapy with multiple antiarrhythmic medications, patients with paroxysmal atrial fibrillation, and patients with ECG evidence of an underlying electrophysiologic disorder (e.g., WPW syndrome) [70,151]. In 2013, the recommendations for catheter ablation were expanded to include patients with symptomatic persistent atrial fibrillation and symptomatic paroxysmal atrial fibrillation in patients with significant left atrial dilation or with significant left ventricular dysfunction [49].
A common complication of CABG surgery is atrial fibrillation. Although reported rates vary, it is estimated that 15% to 50% of persons undergoing CABG surgery will develop atrial fibrillation postoperatively [152,153]. If a patient undergoes CABG surgery combined with valve repair, the likelihood of developing atrial fibrillation increases markedly. This represents a serious problem, as it increases the length of a patient's stay and cost of care, increases the risk of CVA and of hemodynamic compromise in the postoperative patient, and causes discomfort for the patient from palpitations, dyspnea, and other signs and symptoms. Postoperative atrial fibrillation has also been found to be an independent predictor of poor long-term prognosis and long-term mortality [153,154]. Atrial fibrillation generally occurs within five days following surgery and is most likely to occur within two to three days [155]. However, it can develop as late as three weeks postoperatively [154]. Risk factors associated with development of atrial fibrillation include [46,47,80,153,156,157]:
Increasing age; the risk increases in patients older than 60 years of age
COPD
Abrupt discontinuation of beta blocking agents prior to surgery. Research has shown that after CABG surgery, catecholamine levels may be elevated and normal beta adrenergic receptor function can be altered. These changes have been linked to the development of atrial fibrillation. Preoperative use of beta blockers may provide some protection from these changes.
Length of aortic cross-clamp time during the procedure. Longer cross-clamp times have been linked with an increased incidence of atrial fibrillation following surgery. Less common risk factors include chronic renal failure, an enlarged left atrium, cardiomegaly, and a history of rheumatic heart disease.
Postoperative pericarditis
For prevention of postoperative atrial fibrillation following CABG, many sources recommend that beta-blocker therapy be initiated (or resumed) as soon as reasonably possible following surgery [156,158]. Use of a beta blocker for development of atrial fibrillation following cardiac surgery is a class I recommendation in AHA/ACC/HRS guidelines [28]. Prophylactic use of other antiarrhythmic agents has not been recommended. Use of digoxin has been found to have little effect and is not recommended [28]. Preoperative administration of statins may reduce postoperative atrial fibrillation and shorten the patient's stay on the ICU and in the hospital [28,159]. Studies have found that the postoperative prophylactic use of amiodarone reduces the risk of atrial fibrillation and decreases the total cost of care [158,160,161]. However, the use of amiodarone and other antiarrhythmic medications, such as calcium channel blockers and procainamide has been linked to the unacceptable side effects of bradycardia and hypotension [75]. Early intervention for patients who develop increasingly frequent premature atrial contractions (PACs) has been recommended by some clinicians. However, there is no consensus regarding the best treatment. Immediate intervention is indicated for persons who develop atrial fibrillation in the postoperative period. Based on an assessment of the patient's symptoms and hemodynamic status, medical treatment may involve intravenous medications for rate control, pharmacologic cardioversion, or electrical cardioversion along with identification and correction of factors that may contribute to the development of arrhythmias such as hypokalemia and hypomagnesemia. If atrial fibrillation persists despite appropriate therapy, anticoagulation therapy should be started as soon as the surgeon decides it is feasible. Four to six weeks following surgery, the patient's status should be re-evaluated [162,163]. In some persons, postoperative atrial fibrillation is a relatively transient arrhythmia that may spontaneously resolve. However, for others, the arrhythmia may persist and require medical management as previously described for persons with coronary artery disease [28,40].
Atrial fibrillation is an arrhythmia that may develop in persons with WPW syndrome. Management of atrial fibrillation in WPW is very different than management of atrial fibrillation caused by other cardiac and noncardiac causes. To understand the seriousness of this arrhythmia and rationale for treatment, let's look briefly at the WPW syndrome itself.
During early fetal development, a number of bundles of fibers exist that connect the atria and ventricles. As fetal development progresses, these connections disappear until the AV node is left as the only functional electrical connection between atria and ventricles. In persons with WPW, one or more of these fibrous connecting bundles has persisted into adulthood. The connecting bundle, called an accessory pathway, provides an alternative route for the conduction of an electrical impulse through the heart. Depending on a number of factors, an electrical impulse may travel only through the normal conducting pathway, through both the normal and the accessory pathways, or only through the accessory pathway. When the impulse travels through the accessory pathway, it bypasses the normal delay in the AV node and reaches the ventricles early. It initiates ventricular depolarization before the impulse traveling down the normal conduction pathway can reach the ventricles. The ventricles depolarize abnormally. The abnormal conduction through the accessory pathway alters the normal ECG waveform. The changes include [164]:
A shortened PR interval (less than 0.12 sec). The PR interval is shortened because the impulse from the atria reaches the ventricles through the accessory pathway more rapidly than normal.
The presence of a delta wave. A delta wave is a slurring of the initial deflection (either positive or negative) of the QRS complex. It reflects the early, abnormal depolarization of the ventricles that occurs when the impulse travels through the accessory pathway.
An abnormally widened QRS complex (greater than 0.12 sec). The widened, abnormal QRS occurs when most of the ventricular depolarization is stimulated by an impulse traveling down the accessory pathway. In normal conduction, both ventricles depolarize almost simultaneously. With accessory pathway conduction, one ventricle is stimulated to depolarize before the other.
Abnormal ST waves. An ST wave represents repolarization. When depolarization is abnormal, the pattern of repolarization will also be abnormal.
These ECG characteristics are often very subtle and may be confused with ECG changes associated with other conditions, such as acute myocardial infarction, bundle branch block, and left ventricular hypertrophy. The early depolarization of ventricles through accessory pathway conduction is called pre-excitation. The degree of pre-excitation (i.e., the extent to which the ventricles depolarize from accessory pathway conduction) can vary. Factors that increase conduction across the AV node decrease conduction through the accessory pathway. These factors include exertion, intense emotion that increases adrenergic stimulation, and certain medications, such as procainamide, beta agonists (e.g., epinephrine, albuterol, metaproterenol, terbutaline), and atropine. Factors that inhibit or slow conduction across the AV node increase the extent of pre-excitation. These factors may include a normal increase in vagal tone associated with sleep, and medications such as digoxin, adenosine, beta blockers, and calcium channel blockers. Medications known to slow conduction through the AV node should be not used for persons with WPW [165,166].
The presence of multiple conduction pathways (normal and one or more abnormal) often leads to development of tachyarrhythmias, including atrial fibrillation. Patients with WPW who develop atrial flutter or atrial fibrillation are at increased risk of dangerous ventricular arrhythmias due to the extremely fast conduction across the bypass tract [164]. Atrial fibrillation develops in approximately one-third of persons with WPW. Approximately 80% of patients with WPW syndrome will develop atrial fibrillation and 5% will have atrial flutter [164]. Atrial fibrillation seen in WPW is characterized by [17,19,164,165,166]:
Irregularly irregular rhythm
QRS that may appear different and reflect varying degrees of pre-excitation. Some impulses will be conducted through the normal pathway, others through the accessory pathway.
A higher than usual ventricular rate. In "normal" atrial fibrillation, the AV node blocks conduction of most of the fib waves and keeps the ventricular rate from exceeding 150 to 250 bpm. Because impulses in atrial fibrillation associated with WPW can bypass the AV node, the ventricular rate may approach 350 bpm. At this rate, the risk that the atrial fibrillation will degenerate into ventricular fibrillation is high.
WPW should be suspected in any person who shows the following signs and symptoms:
Shortened PR interval and delta wave associated with accessory pathway conduction present on ECG
Subjective complaint of palpitations
History of syncope, presyncope, or sudden cardiac arrest episodes
Definitive diagnosis can be done through electrophysiology testing [164].
When a patient with WPW presents with atrial fibrillation with rapid ventricular response, the patient's hemodynamic status should be immediately assessed. If there are signs of hemodynamic instability, such as hypotension, signs of congestive heart failure, or ischemic chest pain, the patient should be immediately cardioverted [28,164]. If the patient is not hemodynamically unstable, rate control is the high priority. Appropriate medication selection is critical. Use of medications such as verapamil and digoxin that slow or block conduction through the AV node will aggravate atrial fibrillation in WPW and run the risk of accelerating the ventricular rate to the point that ventricular fibrillation can occur [33,164]. The treatment of choice for hemodynamically stable patients with atrial fibrillation and WPW is IV procainamide or ibutilide [28]. Verapamil, diltiazem, adenosine, digoxin (oral or intravenous), and intravenous amiodarone can precipitate ventricular fibrillation and should not be used [28].
Patient D is a man, 68 years of age, who presents to the emergency department late one evening complaining of increasing shortness of breath, dizziness, and the sensation of his "heart racing." On admission, his heart rate is 160 bpm, blood pressure 100/50 mm Hg, respirations 26 breaths per minute, and oxygen saturation 88% on room air. Patient D says that his symptoms started abruptly earlier that day and have steadily become worse. He reports a history of long-standing hypertension, coronary artery disease, and a recent percutaneous transluminal angioplasty with placement of two stents.
Comments and rationale: Symptoms such as those Patient D presents are common indications of acute onset atrial fibrillation with rapid ventricular response. His past medical history is positive for risk factors for the development of atrial fibrillation. These include a positive cardiac history, with hypertension and coronary artery disease, as well as increasing age.
A 12-lead ECG is obtained. It shows a narrow QRS complex tachycardia with an irregularly irregular rhythm. A diagnosis of atrial fibrillation with rapid ventricular response is made. Oxygen via nasal cannula at 2 liters is started. Patient D is attached to continuous telemetry, oxygen saturation, and noninvasive blood pressure monitoring. Telemetry monitoring shows a variable heart rate ranging from 120 to 160 bpm. At lower rates, fibrillatory waves are present. Crackles are present in the bases of both lungs. Peripheral pulses are diminished and irregular. Patient D's skin is cool but dry. A peripheral IV access is established. After determining that Patient D has no known allergies to medications, 20 mg of diltiazem is prescribed to be given by IV push.
Comments and rationale: ECG characteristics associated with atrial fibrillation with rapid ventricular rate include a QRS complex within normal limits (sometimes called "narrow complex") and an irregularly irregular ventricular rhythm. Sinus P waves are absent. At rapid rates, the irregular rhythm and absence of P waves may be difficult to determine. Fibrillatory waves are present but are often not seen at rapid rates. Because of the variable filling time associated with atrial fibrillation, pulse pressure may be intermittent and some beats may not perfuse well to the periphery. Loss of normal atrial contraction coupled with tachycardic heart rates may precipitate signs of heart failure, such as dyspnea, rales, and hypotension. Patient D is symptomatic with his atrial fibrillation but not dangerously unstable (with rapidly falling blood pressure, rapidly increasing signs of heart failure, or increasing chest pain). Therefore, the initial goal of treatment is to slow his heart rate. Diltiazem, a calcium channel blocker, slows conduction through the AV node and prolongs the AV node refractory period, thus slowing the ventricular rate in atrial fibrillation. It has a rapid onset of action. Because IV diltiazem administration is associated with development of bradycardia, heart block, increased signs of congestive heart failure, and hypotension, the patient should be continuously monitored during and after its administration. If the diagnosis of atrial fibrillation with rapid ventricular response cannot be made, adenosine may be used to establish a diagnosis. Oxygen by nasal cannula is used to increase oxygen saturation and decrease the subjective sensation of dyspnea.
In response to the IV diltiazem, Patient D's heart rate initially slowed to a rate of 110 to 120 bpm but rapidly returned to a high rate. After 15 minutes, another bolus was ordered, followed by a continuous infusion of diltiazem at 5 mg/hour. The orders indicated that the drip could be titrated up to a maximum of 15 mg/hour to achieve the desired rate (as long as Patient D's blood pressure remained within ordered parameters). Additional laboratory and diagnostic tests are ordered to rule out or identify any precipitating causes for the arrhythmia. The tests included a complete blood count, serum electrolytes, thyroid function studies, renal and liver function studies, and cardiac enzymes. A portable chest x-ray is performed. Patient D is questioned about his use of over-the-counter medications, alcoholic beverages, illicit drugs, and dietary supplements or herbal medicines. He is then transferred to an inpatient telemetry unit for further monitoring and clinical management.
Comments and rationale: A diltiazem bolus may be repeated after 15 minutes if the desired rate control is not achieved from the initial bolus. The patient should be monitored for the development of side effects, such as hypotension and bradyarrhythmias. Following a bolus, a continuous infusion may then be started to achieve rate control. Blood pressure, ECG, and oxygen saturation monitoring should be done continuously during continuous intravenous infusion. Signs, such as falling blood pressure, decreasing oxygen saturation, and failure to control rate, should be noted and handled immediately. If intolerable side effects develop, the diltiazem will be discontinued and another medication prescribed. If side effects do not develop but rate control is not achieved, additional medications may be prescribed. Other medications used for rate control include procainamide, esmolol, metoprolol, and propranolol. Patients receiving multiple antiarrhythmics should be monitored closely as combination therapy may result in a cumulative effect on heart rate and rhythm, blood pressure, and the patient's risk of developing congestive heart failure. To effectively manage atrial fibrillation, any underlying or precipitating causes should be identified and corrected. Precipitating causes may include anemia, consumption of alcohol, use of cocaine or other similar substance, hyperthyroidism, and electrolyte imbalances (especially potassium and magnesium). Atrial arrhythmias may also develop during acute stages of myocardial infarction.
Patient D is transferred to an appropriate inpatient unit. Continuous ECG, blood pressure, and oxygen saturation monitoring are maintained. After one to two hours on the diltiazem drip, the patient's heart rate drops and stabilizes at 80 to 90 bpm. Fibrillatory waves and an irregularly irregular ventricular response are clearly present on ECG. His laboratory data comes back showing normal serum electrolytes, renal function studies, thyroid function tests, and liver function tests. His hematocrit and hemoglobin are within normal limits. His cardiac enzymes and troponin are negative for myocardial infarction. His chest x-ray shows some congestion in his lower lobes consistent with mild congestive heart failure. Intravenous furosemide is ordered at a low dose to relieve the pulmonary congestion. Patient D's vital signs improve. His blood pressure increases to 118/70 mm Hg, his respiratory rate slows to 18 breaths per minute, and he reports a decreased sensation of dyspnea and palpitations. After he stabilizes, the process of weaning the IV drip and starting the patient on oral diltiazem is initiated. Low-dose oral diltiazem is effective in maintaining rate control for Patient D when his activity is limited; however, when his activity level is increased, he begins to experience increasing episodes of an uncontrolled rate. The dose is increased, and rate control during activity improves. Evaluation of Patient D's medical therapy shows his heart rate controlled at 70 to 80 bpm, his blood pressure is stable, and his symptoms relieved. Because of the high risk of thromboembolic events and serious consequences of CVA, Patient D is started on anticoagulation therapy. It is determined that he is at high risk for a CVA, and a heparin drip is started. Oral anticoagulation with warfarin also begins at this time. Routine monitoring of his partial thromboplastin time and PT/INR is ordered.
Comments and rationale: Once rate control is achieved and maintained, the patient's vital signs are stable, and other signs (e.g., signs of congestive heart failure, angina) have resolved, the patient may be changed to an oral dose for maintenance therapy. Short periods of a rapid rate may still occur, especially with exertion. If these episodes are intermittent and nonsustained, they may be effectively managed by adjusting the medication dose or adding additional antiarrhythmic medications. Rate control is considered successful if it alleviates troublesome symptoms, relieves dyspnea, increases activity tolerance, and improves the patient's ability to perform activities of daily living. Anticoagulation is indicated for persons who remain in atrial fibrillation. Because the atria never fully contract in atrial fibrillation, stasis of blood can occur, which may lead to the development of clots. To prevent thromboembolic events such as CVA, anticoagulation should be started. For high-risk patients, warfarin is the drug of choice. In an inpatient setting, intravenous heparin may be used to provide adequate anticoagulation until warfarin reaches a therapeutic serum level.
With careful questioning, it is determined that Patient D's subjective symptoms of atrial fibrillation actually began a week or more prior to his admission. Patient D admits to feeling some palpitations and shortness of breath intermittently but did not seek medical care until the symptoms became severe. Current assessment of Patient D's status shows normal breath sounds with absence of rales, the chest x-ray shows resolution of pulmonary congestion, vital signs are stable, and he is able to participate in activities of daily living and ambulate without trouble. It is decided to send Patient D home on oral medication to maintain rate control, on warfarin for anticoagulation, and monitoring his status over the next several weeks to evaluate the effectiveness of this therapy.
Comments and rationale: Options for long-term management of the patient with atrial fibrillation include restoration of normal sinus rhythm through pharmacologic or electrical cardioversion or rate control through use of oral antiarrhythmic medications. For patients known (or suspected) to be in atrial fibrillation for more than 48 hours, national standards recommend adequate anticoagulation for three weeks prior to either pharmacologic or electrical cardioversion. Or, a transesophageal echo may be performed to rule out a left atrial thrombus. If no thrombus exists, the patient may be safely cardioverted. For patients whose symptoms are controlled by rate control, oral therapy/antiarrhythmics coupled with oral anticoagulation often is sufficient treatment. If the patient develops recurrent episodes of rapid atrial fibrillation, or experiences troublesome symptoms at home despite optimal antiarrhythmic therapy, he/she may benefit from restoration of normal sinus rhythm by more aggressive methods.
Patient D receives verbal and written instructions on how to take his warfarin and his antiarrhythmic medications. Appointments with the outpatient laboratory for PT/INR monitoring are set up, and a follow-up appointment with his physician is scheduled. Patient D is instructed on signs and symptoms to report to the doctor, including signs of bleeding and recurrence of his signs of rapid atrial fibrillation. Indications that medical therapy is effective in managing his atrial fibrillation include: ability to perform normal activities without symptoms of fatigue, dyspnea, dizziness, or palpitations; vital signs within desired parameters; absence of annoying or problematic side effects from medications; and absence of signs of thromboembolic events.
Patient W is a woman, 58 years of age, who is admitted to the unit with bradycardia and near syncope. She says that this morning she had been grocery shopping, became very dizzy, and nearly passed out. On admission assessment, her blood pressure is 116/74 mm Hg, and her heart rate is 48 bpm and irregular. Her respirations are even and easy at a rate of 20 breaths per minute. Her oxygen saturation on room air is 99%. Peripheral pulses are slightly diminished. Lung fields are clear to auscultation. Patient W is placed on continuous telemetry monitoring, and a 12-lead ECG is obtained. The ECG shows that her underlying rhythm is atrial fibrillation with a slow ventricular response. Patient W says that she has had atrial fibrillation for several months. Initially, her heart rate had been controlled on oral antiarrhythmic medications. However, over the last month, she has been experiencing increasing episodes of palpitations and a rapid heart rate. Her medication had been increased, but she developed hypotension and a slow heart rate on the increased dose. A few days prior to her admission, her oral antiarrhythmic medication was changed. On the new medication, she has not had any prolonged episodes of a rapid heart rate but experienced some "dizzy spells."
Comments and rationale: Lack of adequate rate control coupled with development of serious side effects such as bradycardia, hypotension, and syncope with multiple oral agents are indications that oral antiarrhythmic therapy is not effective in managing the patient's atrial fibrillation. Other options include pharmacologic cardioversion, electrical cardioversion, radiofrequency ablation with or without pacemaker insertion, or continuation of oral medications with insertion of a demand pacemaker to treat symptomatic bradycardia.
Laboratory tests are ordered, including a complete blood count, serum electrolytes, renal and hepatic function tests, chest x-ray, urinalysis, and PT/INR. A peripheral IV access is established. Continuous telemetry monitoring is maintained, and Patient W's vital signs are monitored every four hours. Her heart rate remains between 48 and 52 bpm. Patient W's oral antiarrhythmic medication is discontinued. Analysis of Patient W's ECG shows that her QTc is 580 msec. The therapeutic options of electrical cardioversion, radiofrequency ablation, and continued oral antiarrhythmic therapy with insertion of a demand pacemaker are discussed with the patient. The patient expresses reluctance to undergo pacemaker insertion at this time. With the patient's agreement, she is scheduled for electrical cardioversion. Patient W expresses the understanding that pacemaker insertion or ablation with pacemaker insertion might still be required if cardioversion is unsuccessful or if she becomes symptomatic on therapy to maintain sinus rhythm following successful cardioversion.
Comments and rationale: Laboratory tests such as a complete blood count and serum electrolytes are ordered to rule out any abnormal findings (e.g., anemia, hypokalemia, hypomagnesemia) that may make management of atrial fibrillation more difficult. Due to Patient W's continued bradycardia, her oral antiarrhythmic medication is discontinued. Her QTc interval is significantly prolonged. Because Patient W has developed bradycardia and a prolonged QTc interval, she is not a candidate for pharmacologic cardioversion.
Patient W's complete blood count, renal and hepatic function studies, and urinalysis come back within normal limits. Her serum electrolytes show hypokalemia but a normal serum magnesium level. IV potassium replacement is given, and a repeat potassium level returns within normal limits. Patient W's INR comes back at 2.7. Her usual warfarin dose is continued. A review of her outpatient laboratory results shows that her INR has been maintained between 2.6 and 3.1 for more than six weeks.
Comments and rationale: Hypokalemia may contribute to the continuation of atrial fibrillation. It should be corrected prior to electrical cardioversion or other intervention. Because of the risk of thromboembolic complications caused by left atrial thrombi for persons with atrial fibrillation of more than 48 hours duration, anticoagulation with warfarin is indicated. National standards require anticoagulation for at least three weeks prior to cardioversion. The therapeutic target for warfarin is an INR of 2.0–3.0.
Patient W is kept NPO for six hours prior to the cardioversion. She is taken to the preoperative area prior to the procedure and sedated with IV medications. Continuous ECG, blood pressure, and oxygen saturation monitoring is initiated. The cardioverter/defibrillator is set for a low-energy, synchronized shock. The initial shock is ineffective in restoring sinus rhythm. A second, slightly higher energy shock is effective. ECG monitoring shows Patient W is now in normal sinus rhythm at a rate of 62 bpm. Her vital signs are monitored closely until she wakes up from the sedation. Patient W is returned to her room. Continuous telemetry monitoring is continued.
Comments and rationale: Electrical cardioversion is a painful procedure; sedation or general anesthesia is required. Because of the risks associated with sedation/anesthesia, and the risk that the patient may go into ventricular fibrillation from an electrical shock, cardioversion should be performed in a setting where emergency equipment for intubation and management of cardiac arrest is readily available.
Patient W remains in normal sinus rhythm at an acceptable rate in the immediate period postcardioversion. Her blood pressure is stable, and her dizzy spells do not recur. She is discharged on a low-dose oral antiarrhythmic and warfarin. Patient W is instructed to notify a physician if she experiences palpitations, dizziness, or near-fainting spells.
Comments and rationale: Oral antiarrhythmic therapy is generally required to maintain normal sinus rhythm following successful cardioversion. Although Patient W had been unable to take higher dose oral antiarrhythmics, she was able to tolerate low-dose therapy. It is likely that Patient W will experience short episodes of atrial fibrillation. However, therapy is considered successful if these episodes are brief, do not cause debilitating symptoms, and resolve without additional treatment. National standards recommend that anticoagulation therapy be continued for at least four weeks following cardioversion.
Atrial fibrillation is an increasingly common health problem in the United States. As the American population continues to age, the number of older adults who require clinical management of atrial fibrillation will also increase. Appropriate clinical management involves careful assessment of the patient's symptoms and status, correction of any underlying or contributing causes, and identification of realistic medical goals. Therapies available for the management of atrial fibrillation include a wide variety of antiarrhythmic medications, pharmacologic cardioversion, electrical cardioversion, and radiofrequency ablation with or without pacemaker insertion. Because the risk of CVA is high for persons with atrial fibrillation, anticoagulation therapy should be considered and initiated when appropriate. Ongoing monitoring of the patent's response to antiarrhythmic and anticoagulation therapy is crucial to the effective management of atrial fibrillation and the prevention of serious complications.
| American Heart Association |
| 1-800-242-8721 |
| https://www.heart.org |
| Heart Rhythm Society |
| 202-464-3400 |
| https://www.hrsonline.org |
| National Heart, Lung, and Blood Institute |
| 1-877-645-2448 |
| https://www.nhlbi.nih.gov |
1. Centers for Disease Control and Prevention. Heart Disease. Atrial Fibrillation. Available at https://www.cdc.gov/heartdisease/atrial_fibrillation.htm. Last accessed September 15, 2023
2. Wyse DG, Van Gelder IC, Ellinor PT, et al. Lone atrial fibrillation: does it exist? J Am Coll Cardiol. 2014;63(17):1715-1723.
3. Stewart S, Hart CL, Hole DJ, McMurray JJ. Population prevalence, incidence, and predictors of atrial fibrillation in the Renfrew/Paisley study. Heart. 2001;86(5):516-521.
4. de Denus S, Sanoski CA, Carlsson J, Opolski G, Spinler SA. Rate versus rhythm control in patients with atrial fibrillation: a meta-analysis. Arch Intern Med. 2005;165(3):258-262.
5. Flaker GC, Nasr S. Immediate management of atrial fibrillation: state of the art. Card Electro Rev. 2001;5(2-3):183-186.
6. News: Medical Life Sciences. Atrial Fibrillation News and Research. Available at https://www.news-medical.net/?tag=/Atrial-Fibrillation. Last accessed September 15, 2023.
7. Luderitz B, Jung W. Quality of life in patients with atrial fibrillation. Arch Intern Med. 2000;160(12):1749-1757.
8. Heart Rhythm Society. Atrial Fibrillation. Available at https://www.upbeat.org/heart-rhythm-disorders/atrial-fibrillation#axzz3CwpfdbKy. Last accessed September 15, 2023.
10. National Heart, Lung, and Blood Institute. Atrial Fibrillation. Available at https://www.nhlbi.nih.gov/health/atrial-fibrillation. Last accessed September 15, 2023.
11. National Heart, Lung, and Blood Institute. How the Heart Works. Available at https://www.nhlbi.nih.gov/health/heart. Last accessed September 15, 2023.
12. Vallerand AH, Sanoski CA. Davis's Drug Guide for Nurses. 14th ed. Philadelphia, PA: FA Davis Co.; 2014.
13. Hall JE. Guyton and Hall Textbook of Medical Physiology. 12th ed. Philadelphia, PA: WB Saunders Co.; 2011.
16. Lee S, Khrestian CM, Sahadevan J, Waldo AL. Reconsidering the multiple wavelet hypothesis of atrial fibrillation. Heart Rhythm. 2020;17(11):1976-1983.
18. Cohen M, Naccarelli, GV. Pathophysiology and disease progression of atrial fibrillation: importance of achieving and maintaining sinus rhythm. J Cardiovasc Electrophysiol. 2008;19(8):885-890.
19. Woods SL, Froelicher ES, Motzer SA, Bridges EJ. Cardiac Nursing. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2011.
20. Naccarelli GV, Dell'Orfano JT, Wolbrette DL, Patel HM, Luck JC. Cost-effective management of acute atrial fibrillation: role of rate control, spontaneous conversion, medical and direct current cardioversion, transesophageal echocardiography, and antiembolic therapy. Am J Cardiol. 2000;85(10a):36-45.
21. Nattel S, Burstein B, Dobrev D. Basic science for the clinical electrophysiologist: atrial remodeling and atrial fibrillation: mechanisms and implications. Circulation. 2008;1:62-73.
22. Nattell S, Harada M. Atrial remodeling and atrial fibrillation: recent advances and translational perspectives. JACC. 2014;63(22):2335-2345.
23. Parra-Lucares, A, Villa E, Romero-Hernández E, et al. Tic-tac: a translational approach in mechanisms associated with irregular heartbeat and sinus rhythm restoration in atrial fibrillation patients. Int J Mol Sci. 2023;24(16):12859.
24. Zhou X, Dudley SC Jr. Evidence for inflammation as a driver of atrial fibrillation. Front Cardiovasc Med. 2020;7:62.
25. Chang YL, Zhang JR, Hu WN, Li SN. Atrial fibrosis underlying atrial fibrillation (review). Int J Mol Med. 2021;47(3):9.
26. Guo YH, Yang YQ. Atrial fibrillation: focus on myocardial connexins and gap junctions. Biology (Basel). 2022;11(4):489.
27. Sagris M, Vardas EP, Theofilis P, Antonopoulos AS, Oikonomou E, Tousoulis D. Atrial fibrillation: pathogenesis, predisposing factors, and genetics. Int J Mol Sci. 2022;23(1):6.
28. January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. Circulation. 2014;130:e199-e267.
29. Borke J. Emergent Management of Atrial Flutter. Available at https://emedicine.medscape.com/article/757549-overview. Last accessed September 15, 2023.
30. Olshansky B. Atrioventricular Nodal Reentry Tachycardia. Available at https://emedicine.medscape.com/article/160215-overview. Last accessed September 15, 2023.
31. Nesheiwat Z, Goyal A, Jagtap M. Atrial Fibrillation. Treasure Island (FL): StatPearls Publishing; 2023.
32. Gupta A, lokhandwala Y, Rai N, Malviya A. Adenosine – a drug with myriad utility in the diagnosis and treatment of arrhythmias.J Arrhythm. 2021;37(1):103-112.
33. LexiComp Online. Available at https://online.lexi.com. Last accessed September 15, 2023.
34. Moses S. Atrial Fibrillation Rate Control. Available at https://fpnotebook.com/CV/EKG/AtrlFbrltnRtCntrl.htm. Last accessed September 15, 2023.
35. U.S. Food and Drug Administration. [Archive]. Lexiscan (Regadenoson) and Adenoscan (Adenosine): Drug Safety Communication—Rare but Serious Risk of Heart Attack and Death. Available at https://wayback.archive-it.org/7993/20170112164514/http://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm375981.htm. Last accessed September 15, 2023.
36. Fang MC, Stafford RS, Ruskin JN, Singer DE. National trends in antiarrhythmic and antithrombotic medication use in atrial fibrillation. Arch Intern Med. 2004;164(1):55-60.
37. Rosenthal L. Atrial Fibrillation. Available at https://emedicine.medscape.com/article/151066-overview. Last accessed September 15, 2023.
38. Mayo Clinic. Atrial Fibrillation. Available at https://www.mayoclinic.org/diseases-conditions/atrial-fibrillation/symptoms-causes/syc-20350624. Last accessed September 15, 2023.
39. MedlinePlus. Atrial Fibrillation or Flutter. Available at https://medlineplus.gov/ency/article/000184.htm. Last accessed September 15, 2023.
40. January CT, Wann LS, Calkins H, et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation. A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm society in collaboration with the Society of Thoracic Surgeons. Circulation. 2019;140(2):e125-e151.
41. Karliner LS, Jacobs EA, Chen AH, Mutha S. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv Res. 2007;42(2):727-754.
42. Ramirez D, Engel KG, Tang TS. Language interpreter utilization in the emergency department setting: a clinical review. J Health Care Poor Underserved. 2008;19(2):352-362.
43. Ngo-Metzger Q, Massagli MP, Clarridge BR, et al. Linguistic and cultural barriers to care: perspectives of Chinese and Vietnamese immigrants. J Gen Intern Med. 2003;18(1):44-52.
44. American Heart Association. Guidelines and Statements. Available at https://professional.heart.org/en/guidelines-and-statements. Last accessed September 15, 2023.
45. Frost JL, Campos-Outcalt D, Hoelting D, et al. AAFP Pharmacologic Management of Newly Detected Atrial Fibrillation: Updated Clinical Practice Guideline. Available at https://www.aafp.org/family-physician/patient-care/clinical-recommendations/all-clinical-recommendations/atrial-fibrillation.html. Last accessed September 15, 2023.
46. Reiffel JA. Drug choices in the treatment of atrial fibrillation. Am J Cardiol. 2000;85(10A):12D-19D.
47. Prystowsky EN. Management of atrial fibrillation: therapeutic options and clinical decisions. Am J Cardiol. 2000;85(10A):3D-11D.
48. Hindricks G, Potpara T, Dagres N, et al. 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): the Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021;42(5):373-498.
49. American College of Cardiology, American Heart Association. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61(18):1935-1944.
50. Kalus JS. Pharmacologic management of atrial fibrillation: established and emerging options. J Manag Care Pharm. 2009;15(6-B Suppl):S10-S18.
51. U.S. Food and Drug Administration. Orange Book: Approved Drug Products with Therapeutic Equivalence. Available at https://www.accessdata.fda.gov/scripts/cder/ob/default.cfm. Last accessed September 15, 2023.
52. Merck Manual Home Health Handbook. Overview of Generic Drugs and Drug Naming. Available at https://www.merckmanuals.com/home/drugs/brand-name-and-generic-drugs/overview-of-generic-drugs-and-drug-naming. Last accessed September 15, 2023.
53. Al-Khatib SM, LaPointe NM, Kramer JM, Califf RM. What clinicians should know about the QT interval. JAMA. 2003;289(16):2120-2127.
54. Roy D, Talajic M, Dorian P, et al. Amiodarone to prevent recurrence of atrial fibrillation: Canadian trial of atrial fibrillation investigators. N Engl J Med. 2000;342(13):913-920.
55. Korantzopoulos P, Siogas K. Drug-induced prolongation of the QT interval. N Engl J Med. 2004;350(25):2618-2621.
56. Wood MA, Ithiel A, Fuller BA. Ibutilide and calcium channel blockers: is there an interaction? Cardiovasc Rev Rep. 2003;24(6):326-330.
57. Letelier LM, Udol K, Ena J, Weaver B, Guyatt GH. Effectiveness of amiodarone for conversion of atrial fibrillation to sinus rhythm: a meta-analysis. Arch Intern Med. 2003;163(7):777-785.
58. Hsu LF, Jais P, Sanders P, et al. Catheter ablation for atrial fibrillation in congestive heart failure. N Engl J Med. 2004;351(23):2373-2383.
59. Daily Med. Available at https://dailymed.nlm.nih.gov/dailymed/. Last accessed September 15, 2023.
60. PubMed Health. Diltiazem. Available at https://pubchem.ncbi.nlm.nih.gov/compound/Diltiazem. Last accessed September 15, 2023.
61. PubMed Health. Verapamil. Available at https://pubchem.ncbi.nlm.nih.gov/compound/Verapamil. Last accessed September 15, 2023.
62. PubMed Health. Metoprolol. Available at https://pubchem.ncbi.nlm.nih.gov/compound/Metoprolol. Last accessed September 15, 2023.
63. Wooten JM, Earnest J, Reyes J. Review of common adverse effects of selected antiarrhythmic drugs. Crit Care Nurs Q. 2000;22(4):23-38.
64. Amabile CM, Spencer AP. Keeping your patient with heart failure safe: a review of potentially dangerous medications. Arch Intern Med. 2004;164(7):709-720.
65. MedlinePlus. Procainamide. Available at https://medlineplus.gov/druginfo/meds/a682398.html. Last accessed September 15, 2023.
66. Zipes DP, Calkins H, Daubert JP, et al. 2015 ACC/AHA/HRS advanced training statement on clinical cardiac electrophysiology (a revision of the ACC/AHA 2006 update of the clinical competence statement on invasive electrophysiology studies, catheter ablation, and cardioversion). Heart Rhythm. 2016;13(1):E3-E37.
67. Mandrola J. Digoxin Stuns in RATE-AF Trial. Available at https://www.medscape.com/viewarticle/936544#vp_1. Last accessed September 15, 2023.
68. Lindeboom JE, Kingma JH, Crijns HJ, Dunselman PH. Efficacy and safety of intravenous dofetilide for rapid termination of atrial fibrillation and atrial flutter. Am J Cardiol. 2000;85(8):1031-1033.
69. Marinelli A, Capucci A. Antiarrhythmic drugs for atrial fibrillation. Expert Opin Pharmacother. 2011;12(8):1201-1215.
70. Wazni OM, Marrouche NF, Martin DO, et al. Radiofrequency ablation versus antiarrhythmic drugs as first-line treatment of symptomatic atrial fibrillation: a randomized trial. JAMA. 2005;293(21):2634-2640.
71. Dave J. Torsade de Pointes. Available at https://emedicine.medscape.com/article/1950863-overview#a1. Last accessed September 15, 2023.
72. Mitchell LB. Torsades de Pointes Ventricular Tachycardia. Available at https://www.merckmanuals.com/professional/cardiovascular-disorders/specific-cardiac-arrhythmias/torsades-de-pointes-ventricular-tachycardia?autoredirectid=20575. Last accessed September 15, 2023.
73. Patsilinakos S, Christou A, Kafkas N, et al. Effect of high doses of magnesium on converting ibutilide to a safe and more effective agent. Am J Cardiol. 2010;106(5):673-676.
74. Pfizer. Tikosyn (Dofetilide): Important Safety Information. Available at https://labeling.pfizer.com/ShowLabeling.aspx?id=639. Last accessed September 15, 2023.
75. Valembois L, Audureau E, Takeda A, Jarzebowski W, Belmin J, Lafuente-Lafuente C. Antiarrhythmics for maintaining sinus rhythm after cardioversion of atrial fibrillation. Cochrane Database Syst Rev. 2019;(9):CD005049.
76. Jaiswal P, Attar BM, Yap JE, et al. Acute liver failure with amiodarone infusion: a case report and systematic review. J Clin Pharm Ther. 2018;43(1):129-133.
77. U.S. Food and Drug Administration. FDA Drug Safety Communication: Revised Dose Limitation for Zocor (simvastatin) When Taken with Amiodarone. Available at https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-revised-dose-limitation-zocor-simvastatin-when-taken-amiodarone. Last accessed September 15, 2023.
78. Stoschitzky K, Stoschitzky G, Lercher P, Brussee H, Lamprecht G, Lindner W. Propafenone shows class Ic and class II antiarrhythmic effects. Europace. 2016;18(4):568-571.
79. Raijpurohit N, Aryal SR, Khan MA, Stys AT, Stys TP. Propafenone associated severe central nervous system and cardiovascular toxicity due to mirtazapine: a case of severe drug interaction. S D Med. 2014;67(4):137-139.
80. American College of Cardiology/American Heart Association. 2006 update of the clinical competence statement on invasive electrophysiology studies, catheter ablation, and cardioversion: A report of the American College of Cardiology/American Heart Association/American College of Physicians Task Force on Clinical Competence and Training: developed in collaboration with the Heart Rhythm Society. Circulation. 2006;114(15):1654-1668.
81. Beinart SC. Synchronized Electrical Cardioversion. Available at http://emedicine.medscape.com/article/1834044-overview#a01. Last accessed September 15, 2023.
82. Airaksinen K, Gröonberg T, Nuotio I, et al. Thromboembolic complications after cardioversion of acute atrial fibrillation: the FinCV Study. J Am Coll Cardiol. 2013;62:1187-1192.
83. Sultan A, Steven D, Rostock T, et al. Intravenous administration of magnesium and potassium solution lowers energy levels and increases success rates electrically cardioverting atrial fibrillation. J Cardiovasc Electrophysiol. 2011:23(1):54-59.
84. Celebi OO, Celebi S, Canbay A, Erqun G, Aydogdu S, Diker E. The effect of sinus rhythm restoration on high-sensitivity C-reactive protein levels and their association with long-term atrial fibrillation recurrence after electrical cardioversion. Cardiology. 2011;118(3):168-174.
85. Liu T, Li G, Li L, Korantzopoulos P. Association between C-reactive protein and recurrence of atrial fibrillation after successful electrical cardioversion: a meta-analysis. J Am Coll Cardiol. 2007;49(15):1642-1648.
86. Korantzopoulos P, Kalantzi K, Siogas K. Goudevenos JA. Long-term prognostic value of baseline C-reactive protein in predicting recurrence of atrial fibrillation after electrical cardioversion. Pacing Clin Electrophysiol. 2008;31(10):1272-1276.
87. Henningsen KM, Therkelsen SK, Bruunsgaard H, Krabbe KS, Pedersen BK, Svendsen JH. Prognostic impact of hs-CRP and IL-6 in patients with persistent atrial fibrillation treated with electrical cardioversion. Scand J Clin Lab Invest. 2009;69(3):425-432.
88. Janardhan AH, Gutbrod SR, Li W, Lang D, Schuessler RB, Efimov IR. Multistage electrotherapy delivered through chronically-implanted leads terminates atrial fibrillation with lower energy than a single biphasic shock. J Am Coll Cardiol. 2014;63(1):40-48.
89. Gerstenfeld EP, Everett TH 4th. Internal atrial defibrillation revisited: how low can we go? J Am Coll Cardiol. 2014;63(1):49-51.
90. Valembois L, Audureau E, Takeda A, Jarzebowski W, Belmin J, Lafuente-Lafuente C. Antiarrhythmics for maintaining sinus rhythm after cardioversion of atrial fibrillation. Cochrane Database Syst Rev. 2019;9:CD005049.
91. Wann LS, Curtis AB, January CT, et al. 2011 ACCF/AHA/HRS focused update on the management of patients with atrial fibrillation (updating the 2006 guideline): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011;123:104-123.
92. U.S. Food and Drug Administration. Label and Approval History: BETAPACE AF (Sotalol HCI). Available at https://www.accessdata.fda.gov/drugsatfda_docs/label/2011/021151s009lbl.pdf. Last accessed September 15, 2023.
93. Tamargo J, Lopez-Farre A, Caballero R, Delpon E. Dronedarone. Drugs Today (Barc). 2011;47(2):109-133.
94. Rosei EA, Salvetti M. Dronedarone: an emerging therapy for atrial fibrillation. Ther Adv Cardiovasc Dis. 2010;4(3):155-164.
95. Brenner R, Delacretaz E. Dronedarone for the management of atrial fibrillation. Swiss Med Wkly. 2010;141:w13158.
96. Schweizer PA, Becker R, Katus HA, Thomas D. Dronedarone: current evidence for its safety and efficacy in the management of atrial fibrillation. Drug Des Devel Ther. 2011;6:27-39.
97. U.S. Food and Drug Administration. Severe Liver Injury Associated with the Use of Dronedarone (Marketed as Multaq). Available at https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-severe-liver-injury-associated-use-dronedarone-marketed-multaq. Last accessed September 15, 2023.
98. Spiezia L, Prandoni P. Prevention of thromboembolic complications in patients with atrial fibrillation. Minerva Cardioangiol. 2008;56(6):643-652.
99. Marinigh R, Lip GY, Lane DA. Stroke prevention in atrial fibrillation patients. Expert Opin Pharmacother. 2010;11(14):2331-2350.
100. Jauch EC. Ischemic Stroke. Available at https://emedicine.medscape.com/article/1916852-overview. Last accessed September 15, 2023.
101. Centers for Disease Control and Prevention. Preventing Stroke: What You Can Do. Available at https://www.cdc.gov/stroke/prevention.htm. Last accessed September 15, 2023.
102. Centers for Disease Control and Prevention. Know Your Stroke Risk. Available at https://www.cdc.gov/stroke/risk_factors.htm. Last accessed September 15, 2023.
103. Ogilvie IM, Newton N, Welner SA, Cowell W, Lip GY. Underuse of oral anticoagulants in atrial fibrillation: a systematic review. Am J Med. 2010;123:638-645.
104. Gladstone DJ, Bui E, Fang J, et al. Potentially preventable strokes in high-risk patients with atrial fibrillation who are not adequately anticoagulated. Stroke. 2009;40:235-240.
105. The SPAF III Writing Committee for the Stroke Prevention in Atrial Fibrillation Investigators. Patients with nonvalvular atrial fibrillation at low risk of stroke during treatment with aspirin: Stroke Prevention in Atrial Fibrillation III Study. JAMA. 1998;279:1273-1277.
106. Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA. 2001;285:2864-2870.
107. van Walraven C, Hart RG, Wells GA, et al. A clinical prediction rule to identify patients with atrial fibrillation and a low risk for stroke while taking aspirin. Arch Intern Med. 2003;163:936-943.
108. Wang TJ, Massaro JM, Levy D, et al. A risk score for predicting stroke or death in individuals with new-onset atrial fibrillation in the community: the Framingham Heart Study. JAMA. 2003;290:1049-1056.
109. Lip GY, Nieuwlat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010;137:263-272.
110. Atrial Fibrillation investigators. Risk factors for stroke and efficacy of antithrombotic therapy in atrial fibrillation. Analysis of pooled data from five randomized controlled trials. Arch Intern Med. 1994;154(13):1449-1457.
111. Olesen JB, Lip GY, Lane DA, et al. Vascular disease and stroke risk in atrial fibrillation: a nationwide cohort study. Am J Med. 2012;125(8):e13-e23.
112. Friberg L, Rosenqvist M, Lip GY. Evaluation of risk stratification schemes for ischaemic stroke and bleeding in 182,678 patients with atrial fibrillation: the Swedish Atrial Fibrillation cohort study. Eur Heart J. 2012;33(12):1500-1510.
113. van Walraven C, Hart RG, Connolly S, et al. Effect of age on stroke prevention therapy in patients with atrial fibrillation: the atrial fibrillation investigators. Stroke. 2009;40(4):1410-1416.
114. CHA2DS2-VASc Score for Atrial Fibrillation Stroke Risk. Available at https://www.mdcalc.com/cha2ds2-vasc-score-atrial-fibrillation-stroke-risk. Last accessed September 15, 2023.
116. Olesen JB, Lip GY, Lane DA, et al. Vascular disease and stroke risk in atrial fibrillation: a nationwide cohort study. Am J Med. 2012;125(8):e13-e23.
117. Lane DA, Lip GY. Use of the CHA(2)DS(2)-VASc and HAS-BLED scores to aid decision making for thromboprophylaxis in nonvalvular atrial fibrillation. Circulation. 2012;126(7):860-865.
118. Ajam T, CHADS2 Score for risk assessment in atrial fibrillation. Available at https://emedicine.medscape.com/article/2172597-overview. Last accessed September 15, 2023.
119. Fiore LD, Ezekowitz MD, Brophy MT, et al. Department of Veterans Affairs Cooperative Studies Program Clinical Trial comparing combined warfarin and aspirin with aspirin alone in survivors of acute myocardial infarction: primary results of the CHAMP study. Circulation. 2002;105(5):557-563.
120. The Organization to Assess Strategies for Ischemic Syndromes (OASIS) Investigators. Effects of long-term, moderate-intensity oral anticoagulation in addition to aspirin in unstable angina. J Am Coll Cardiol. 2001;37(2):475-484.
121. ESPRIT Study Group, Halkes PH, van Gijn J, et al. Medium intensity oral anticoagulants versus aspirin after cerebral ischaemia of arterial origin (ESPRIT): a randomized controlled trial. Lancet Neurol. 2007;6(2):115-124.
122. Hurlen M, Abdelnoor M, Smith P, Erikssen J, Arnesen H. Warfarin, aspirin, or both after myocardial infarction. N Engl J Med. 2002;347(13):969-974.
123. Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med. 2007;146(12):857-867.
124. Ebell MH. Choosing between warfarin (Coumadin) and aspirin therapy for patients with atrial fibrillation. Am Fam Physician. 2005;71(12):2348-2350.
125. Man-Son-Hing M, Laupacis A. Anticoagulant-related bleeding in older persons with atrial fibrillation: physicians' fears often unfounded. Arch Intern Med. 2003;163(13):1580-1586.
126. Bristol-Myers Squibb Company. Medication Guide: Coumadin (Warfarin Sodium) Tablets. Available at https://packageinserts.bms.com/medguide/medguide_coumadin.pdf. Last accessed September 15, 2023.
127. Verheugt FWA. Novel oral anticoagulants to prevent stroke in atrial fibrillation. Nature Reviews Cardiology. 2010;7(3):149-154.
128. Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361:1139-1151.
129. U.S. Food and Drug Administration. FDA Drug Safety Communication: Pradaxa (Dabigatran Etexilate Mesylate) Should Not Be Used in Patients with Mechanical Prosthetic Heart Valves. Available at https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-pradaxa-dabigatran-etexilate-mesylate-should-not-be-used-patients. Last accessed September 15, 2023.
130. Uchino K, Hernandez AV. Dabigatran association with higher risk of acute coronary events: meta-analysis of noninferiority randomized controlled trials. Arch Intern Med. 2012;172(5):397-402.
131. Hills MT. FDA Approves Pradaxa as Alternative to Warfarin for Stroke Prevention in Atrial Fibrillation. Available at https://www.stopafib.org/afib-news-events/news/fda-approves-pradaxa-as-alternative-to-warfarin-for-stroke-prevention-in-atrial-fibrillation/. Last accessed September 15, 2023.
132. McCarty D, Robinson A. Factor Xa inhibitors: a novel therapeutic class for the treatment of nonvalvular atrial fibrillation. Ther Adv Cardiovasc Dis. 2016;10(1):37-49.
133. Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365:883-891.
134. Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365:981-992.
135. Giugliano RP, Ruff CT, Braunwald E, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369(22):2093-2104.
136. Agency for Healthcare Research and Quality. Radiofrequency Ablation for Atrial Fibrillation: A Guide for Adults. Available at https://www.ncbi.nlm.nih.gov/books/NBK45597. Last accessed September 15, 2023.
137. Greenberg ML. Catheter Ablation. Available at https://emedicine.medscape.com/article/1828541-overview#a01. Last accessed September 15, 2023.
139. Marrouche NF, Brachmann J, Andresen D, et al, for the CASTLE-AF investigators. Catheter ablation for atrial fibrillation with heart failure. N Engl J Med. 2018;378(5):417-427.
140. Calkins H, Hindricks G, Cappato R, et al. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Heart Rhythm. 2017;14(10):e275-e444.
141. Calkins H. When it comes to defining the outcomes of catheter ablation of atrial fibrillation, an implantable monitor is a great place to start. Circulation. 2019;140:1789-1791.
142. Andrade JG, Champagne J, Dubuc M, et al. Cryoballoon or radiofrequency ablation for atrial fibrillation assessed by continuous monitoring. Circulation. 2019;140:1779-1788.
143. Hakalahti A, Biancari F, Nelsen JC, Raatikainen MJ. Radiogrequency ablation vs. antiarrhythmic drug therapy as first line treatment of symptomatic atrial fibrillation: systematic review and meta-analysis. Europace. 2015;17(3):370-378.
144. Saremi F, Tafti M. The role of computed tomography and magnetic resonance imaging in ablation procedures for treatment of atrial fibrillation. Semin Ultrasound CT MR. 2009;30(2):125-156.
145. Stabile G, Turco P, La Rocca V, Nocerino P, Stabile E, De Simone A. Is pulmonary vein isolation necessary for curing atrial fibrillation? Circulation. 2003;108(6):657-660.
146. Centurion OA, Shimizu A. Rate control strategy elevated to primary treatment for atrial fibrillation: has the last word already been spoken? J Atr Fibrillation. 2014;7(4):1152.
147. Ernst S, Kuck KH. Current status of catheter ablation for atrial fibrillation. Herz. 2006;31(2):113-117.
148. Stuehlinger M, Hoenig S, Spuller K, et al. CoolLoop® First: a first in man study to test a novel circular cryoablation system in paroxysmal atrial fibrillation. J Atr Fibrillation. 2015;8(3):1287.
149. Kuchynka P, Podzimkova J, Masek M, et al. The role of magnetic resonance imaging and cardiac computed tomography in the assessment of left atrial anatomy, size, and function. Biomed Res Int. 2015;247865.
150. Leong DP, Dokainish H. Left atrial volume and function in patients with atrial fibrillation. Curr Opin Cardiol. 2014;29(5):437-444.
151. National Collaborating Centre for Chronic Conditions. Atrial Fibrillation: National Clinical Guideline for Management In Primary and Secondary Care. London: Royal College of Physicians; 2006.
152. Magee MJ, Herbert MA, Dewey TM, et al. Atrial fibrillation after coronary artery bypass grafting surgery: development of a predictive risk algorithm. Ann Thorac Surg. 2007;83:1707-1712.
153. Tzoumas A, Nagraj S, Tasoudis P, et al. Atrial fibrillation following coronary artery bypass graft: where do we stand? Cardiovasc Revasc Med. 2022;40:172-179.
154. El-Chami MF, Kilgo P, Thourani V, et al. New-onset atrial fibrillation predicts long-term mortality after coronary artery bypass graft.J Am Coll Cardiol. 2010;555:1370-1376.
155. Konstantino Y, Yovel DZ, Friger MD, Sahar G, Knyazer B, Amit G. Postoperative atrial fibrillation following coronary artery bypass graft surgery predicts long-term atrial fibrillation and stroke. Isr Med Assoc J. 2016;18(12):744-748.
156. Mathew JP, Fontes ML, Tudor IC, et al. A multicenter risk index for atrial fibrillation after cardiac surgery. JAMA. 2004;291(14):1720-1729.
157. Stevenson WG, Stevenson LW. Atrial fibrillation and heart failure—five more years. N Engl J Med. 2004;351(23):2437-2440.
158. Arsenault KA, Yusuf AM, Crystal E, et al. Interventions for preventing post-operative atrial fibrillation in patients undergoing heart surgery. Cochrane Database Syst Rev. 2013;(1):CD003611.
159. Chopra V, Wesorick DH, Sussman JB, et al. Effect of perioperative statins on death, myocardial infarction, atrial fibrillation, and length of stay: a systematic review and meta-analysis. Arch Surg. 2012;147(2):181-189.
160. Zebis LR, Christensen TD, Kristiansen IS, Hjortdal VE. Amiodarone cost effectiveness in preventing atrial fibrillation after coronary artery bypass graft surgery. Ann Thorac Surg. 2008;85(1):28-32.
161. Zebis LR, Christensen TD, Thomsen HF, et al. Practical regimen for amiodarone use in preventing postoperative atrial fibrillation.Ann Thorac Surg. 2007;83(4):1326-1331.
162. Singer DE, Albers GW, Dalen JE, et al. Antithrombotic therapy in atrial fibrillation: American College of Chest Physicians evidence-based clinical practice guidelines, 8th edition. Chest. 2008;133(6 Suppl):546S-592S.
163. You JJ, Singer DE, Howard PA, et al. Antithrombotic therapy for atrial fibrillation: antithrombotic therapy and prevention of thrombosis, 9th edition: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141(2 Suppl):e531S-e575S.
164. Ellis CR. Wolff-Parkinson-White Syndrome. Available at https://emedicine.medscape.com/article/159222-overview. Last accessed September 15, 2023.
1. Lip GYH, Banerjee A, Boriani G, et al. Antithrombotic therapy for atrial fibrillation: CHEST guideline and expert panel report. Chest. 2018;154(5):p1121-p1201. Available at https://journal.chestnet.org/article/S0012-3692(18)32244-X/fulltext. Last accessed October 10, 2023.
2. January CT, Wann LS, Calkins H, et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society in Collaboration with the Society of Thoracic Surgeons. Circulation. 2019;140:e125-e151. Available at https://www.ahajournals.org/doi/10.1161/CIR.0000000000000665. Last accessed October 10, 2023.
Mention of commercial products does not indicate endorsement.