Dissociation is a natural and normal part of the human experience. An inherent mechanism of the primitive brain, dissociation allows for needs to be met and for protection when one feels especially vulnerable. Understanding the intricacies of dissociation is imperative if a therapist or other helping professional wishes to be as trauma-focused as possible. Trauma and dissociation go hand-in-hand, and this interplay can manifest in ways that are clinically puzzling. However, a main theme of this course is that understanding one's own relationship with dissociation and internal world of parts is an important educational step to working with dissociation effectively.
- INTRODUCTION
- FUNDAMENTALS OF DISSOCIATION
- DIAGNOSTIC PERSPECTIVES ON DISSOCIATION
- THE DISSOCIATIVE PROFILE EXERCISE
- FOUNDATIONS OF WORKING WITH CLINICALLY SIGNIFICANT DISSOCIATION
- PERSONAL METAPHOR AND PARTS WORK
- ADDICTION AS DISSOCIATION
- SUCCESSFUL TREATMENT PLANNING
- CONCLUSION
- RESOURCES
- Works Cited
- Evidence-Based Practice Recommendations Citations
This course is designed for psychotherapists, counselors, social workers, and other helping professionals practicing in a variety of modalities and from a variety of traditions.
The purpose of this course is to equip clinicians with the knowledge and skills that they need to better understand dissociation and its connection to trauma.
Upon completion of this course, you should be able to:
- Define dissociation in a trauma-focused manner.
- Describe the impact and manifestations of trauma and dissociation on the brain.
- Identify common myths about working with dissociative clients in psychotherapy, including historical roots.
- Outline diagnostic criteria for dissociative disorders.
- Describe the Dissociative Profile exercise.
- Describe the screening tools and inventories available for use in clinical settings regarding dissociation.
- Apply personal metaphor and parts work in the care of clients with dissociation.
- Outline the similarities between addiction and dissociation and how they can be framed.
- Discuss key components of successful treatment planning for clients with dissociation.
- Implement approaches for early and later phases of dissociative disorder treatment.
Jamie Marich, PhD, LPCC-S, REAT, RYT-500, RMT, (she/they) travels internationally speaking on topics related to EMDR therapy, trauma, addiction, expressive arts, and mindfulness while maintaining a private practice and online education operation, the Institute for Creative Mindfulness, in her home base of northeast Ohio. She is the developer of the Dancing Mindfulness approach to expressive arts therapy and the developer of Yoga for Clinicians. Dr. Marich is the author of numerous books, including EMDR Made Simple, Trauma Made Simple, and EMDR Therapy and Mindfulness for Trauma Focused Care (written in collaboration with Dr. Stephen Dansiger). She is also the author of Process Not Perfection: Expressive Arts Solutions for Trauma Recovery. In 2020, a revised and expanded edition of Trauma and the 12 Steps was released. In 2022 and 2023, Dr. Marich published two additional books: The Healing Power of Jiu-Jitsu: A Guide to Transforming Trauma and Facilitating Recovery and Dissociation Made Simple. Dr. Marich is a woman living with a dissociative disorder, and this forms the basis of her award-winning passion for advocacy in the mental health field.
Contributing faculty, Jamie Marich, PhD, LPCC-S, REAT, RYT-500, RMT, has disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
Alice Yick Flanagan, PhD, MSW
Margaret Donohue, PhD
The division planners have disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
Sarah Campbell
The Director of Development and Academic Affairs has disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
The purpose of NetCE is to provide challenging curricula to assist healthcare professionals to raise their levels of expertise while fulfilling their continuing education requirements, thereby improving the quality of healthcare.
Our contributing faculty members have taken care to ensure that the information and recommendations are accurate and compatible with the standards generally accepted at the time of publication. The publisher disclaims any liability, loss or damage incurred as a consequence, directly or indirectly, of the use and application of any of the contents. Participants are cautioned about the potential risk of using limited knowledge when integrating new techniques into practice.
It is the policy of NetCE not to accept commercial support. Furthermore, commercial interests are prohibited from distributing or providing access to this activity to learners.
Supported browsers for Windows include Microsoft Internet Explorer 9.0 and up, Mozilla Firefox 3.0 and up, Opera 9.0 and up, and Google Chrome. Supported browsers for Macintosh include Safari, Mozilla Firefox 3.0 and up, Opera 9.0 and up, and Google Chrome. Other operating systems and browsers that include complete implementations of ECMAScript edition 3 and CSS 2.0 may work, but are not supported. Supported browsers must utilize the TLS encryption protocol v1.1 or v1.2 in order to connect to pages that require a secured HTTPS connection. TLS v1.0 is not supported.
The role of implicit biases on healthcare outcomes has become a concern, as there is some evidence that implicit biases contribute to health disparities, professionals' attitudes toward and interactions with patients, quality of care, diagnoses, and treatment decisions. This may produce differences in help-seeking, diagnoses, and ultimately treatments and interventions. Implicit biases may also unwittingly produce professional behaviors, attitudes, and interactions that reduce patients' trust and comfort with their provider, leading to earlier termination of visits and/or reduced adherence and follow-up. Disadvantaged groups are marginalized in the healthcare system and vulnerable on multiple levels; health professionals' implicit biases can further exacerbate these existing disadvantages.
Interventions or strategies designed to reduce implicit bias may be categorized as change-based or control-based. Change-based interventions focus on reducing or changing cognitive associations underlying implicit biases. These interventions might include challenging stereotypes. Conversely, control-based interventions involve reducing the effects of the implicit bias on the individual's behaviors. These strategies include increasing awareness of biased thoughts and responses. The two types of interventions are not mutually exclusive and may be used synergistically.
#76081: Demystifying Dissociation: Principles, Best Practices, and Clinical Approaches
Dissociation is great puzzlement to many clinical professionals, and often it is through no fault of their own. Many graduate training programs skim over the dissociation part of the Diagnostic and Statistical Manual of Mental Disorders (DSM) and teach that dissociative identify disorder (DID) is extremely rare. Likewise, very little may be included on trauma as well, so the potential association with dissociation is often left unexplored.
Since 2000, there has been more interest and a greater respect for trauma and what is called trauma-informed and trauma-focused care in the clinical professions. The term trauma comes from the Greek word meaning wound, and in its most general sense, it can be defined as any unhealed wound of a physical, emotional, psychological, sexual, or spiritual nature. Like physical wounds, other types of trauma can be experienced in various degrees and levels of intensity. If left unhealed or unprocessed, problems can result that impair an individual's lifestyle or way of being in the world. The most common trauma-related diagnosis is post-traumatic stress disorder (PTSD), although other clinical diagnoses (e.g., adjustment disorders, reactive attachment disorder, personality disorders) can also have their root in unhealed trauma. As trauma awareness and understanding increases, the field is also realizing that many other diagnoses can have a root in unhealed trauma or their severity can be exacerbated by unhealed trauma.
Some have hypothesized that wherever there is trauma, some aspect of dissociation exists, reflected in the idiom: "If trauma is walking in the door, dissociation is at least waiting in the parking lot." If systems of care are truly going to be trauma-informed (i.e., understanding how unhealed trauma affects the brain and manifests in human distress and behavior), they should also work toward being more dissociation-informed. The hope is that all systems of human services can at least be trauma-informed, yet many clinicians are also in a position to be trauma-focused in their care. Trauma-focused care recognizes the role that unhealed trauma plays in human pathology, and trauma-focused clinicians develop treatment plans using the modalities in which they are trained to actively target sources of trauma and work to bring about resolution[1]. To deliver trauma-focused care, competency in working with dissociation is imperative.
The aim of this course is to equip clinicians with the knowledge and skills that they need to better understand dissociation and its connection to trauma. These knowledge and skills will allow clinicians to be more trauma-informed and trauma-focused in their approach to clinical work. There can be frustration that comes with addressing dissociation, which often originates from myths and misinformation in the field—and teachings on dissociation from some sources that can be too technical.
This phenomenological approach will hopefully empower clinicians to more effectively address dissociation and its various manifestations in clinical practice. Having a sense of dissociation's inherent normalcy in the human experience is a critical aspect of demystifying dissociation. The more one is willing to be introspective throughout this course, as opposed to just reading through the content, the more that can be gained from the course. A series of guided exercises are designed to assist in this process.
Author's Note : The voice with which I am guiding you in this course is one of a trauma and dissociation specialist, trainer, and author. I am also a woman in long-term recovery from a dissociative disorder. I was diagnosed in graduate school when I struggled with internship due to my own unhealed trauma. I endeavor to use my lived experience in concert with modern scholarship about dissociation. Personal stories and experiences will be included throughout the text in italics.
The word dissociation is derived from a Latin root word meaning to sever or to separate. In clinical understanding, dissociation is the inherent human tendency to separate oneself from the present moment when it becomes unpleasant or overwhelming. Dissociation can also refer to severed or separated aspects of self. In common clinical parlance, these separations may be referred to as "parts." Older terminology (e.g., "alters," "introjects") may still be used, although parts is generally seen as more normalizing and less shaming as a clinical conceptualization strategy. Just like all humans dissociate, all humans have different parts or aspects of themselves. In cases of clinically significant dissociation, the separation of parts is typically more pronounced.
The fact that dissociation encapsulates two meanings—the separation from the present moment that can manifest in a variety of ways and the separation from aspects of self—can make learning about and understanding it rather confusing. Consider, however, that the general purposes of dissociation are the same in both constructs: to protect oneself and to get one's needs met. Even the most innocuous example of a person "zoning out" or daydreaming can be seen through this lens. Individuals can go away in their minds to protect themselves from the distress of the present moment, whether that distress shows up as boredom, pain, or overwhelm. Parts, or aspects of self, will either develop over time or fail to integrate with the total self (depending on defining theory) to protect the self or to get needs met, typically needs that primary caregivers are not providing. Underlying theories of dissociation will be discussed in detail later in this course.
One of the leading psychological scholars in the treatment of dissociation is Dr. Elizabeth Howell. In her book The Dissociative Mind, she contends [2]:
Chronic trauma...that occurs early in life has profound effects on personality development and can lead to the development of dissociative identity disorder (DID), other dissociative disorders, personality disorders, psychotic thinking, and a host of symptoms such as anxiety, depression, eating disorders, and substance abuse. In my view, DID is simply an extreme version of the dissociative structure of the psyche that characterizes us all. Dissociation, in a general sense, refers to the rigid separation of parts of experience, including somatic experience, consciousness, affects, perception, identity, and memory.
This contention has inspired scores of clinicians. The key to better understanding dissociation truly rests in normalizing it [2,3].
When contemplating dissociation in a general sense, common expressions that come to mind include daydreaming, "zoning out," inability to make appropriate eye contact, escaping to imaginal or fantastical landscapes in the mind, or losing emotional connection to a story being told. Some people will start to yawn, fall asleep, or lose appropriate volume in their voice when distressed. It is very likely that most (if not all) people have done one or more of these things in their lives and may even do them on a regular basis, with or without a clinically significant dissociative diagnosis. Modern-day examples of dissociation include watching too much television, playing on the smartphone, or mind numbingly scrolling through social media. These activities are not dissociative in and of themselves but can be used in a dissociative manner. Even activities used in therapy for emotion regulation, including guided visualizations, can be dissociative because they remove the practitioner from their present surroundings and experiences. While the intention may be solid and indeed very helpful to many people, consider how a person could continue to use such an exercise as an escape instead of as a healthy coping strategy.
In normalizing dissociation, it is useful to look at the construct of adaptive and maladaptive in describing dissociative phenomenon. These distinctions of adaptive and maladaptive are essential to eye movement desensitization and reprocessing (EMDR) therapy [4]. As constructs, they are similar to the descriptors healthy and unhealthy but with much less of a value judgment. Furthermore, what is adaptive to one person may not be adaptive to another person. What was adaptive at one point in one's life may not be adaptive at other points in his or her life. Consider this example as it relates to dissociation: For a young child growing up in a dysfunctional home, daydreaming was adaptive because it helped him/her survive the perils of this upbringing. However, as an adult, chronic daydreaming can impede one's ability to work and support oneself, keeping one removed from certain realities that need to be faced.
Another example of commonplace dissociation is binge watching television. This practice could be dissociative in a maladaptive sense, but it could also be a needed avenue for self-care that helps a person disconnect from the rigors of work life and day-to-day responsibilities, depending on the relationship and intention with the activity. Clinicians can assist clients in making this distinction only after considering how these patterns show up in their own lives. For example, a clinician may regularly binge watch television and feel like it is a healthy outlet for rest. When the clinician is dealing with intensity in their feelings and life, it is important that they take a break. One could argue that it would be more dissociative, as an avenue to escape feelings, if the clinician dove into doing more work to keep from being present. Work can be tricky for individuals to evaluate, because while it is often an inherently positive activity, it can be taken to a maladaptively dissociative place. A later section of this course will more fully examine the intricate relationship between dissociation and addiction, but briefly, addictive behaviors generally begin as dissociative coping, usually in response to trauma or to distress.
In normalizing dissociation, it is also imperative to examine the notion of parts or aspects of self. Again, this will be more fully explored later in this course, but before starting this activity, take a moment to examine whether or not you relate to having different parts, sides, or aspects of yourself. Many use the common terminology of "inner child," vis-à-vis the more rational, presenting adult. If you have ever used this language, you are already recognizing the construct of parts. Some people, especially those who struggle with addiction, may reference having a "Dr. Jekyll and Mr. Hyde" phenomenon happening within them. Some people will even say that their sadness, anger, or other emotional experience can take on a life of their own, which can also speak to the separation of parts, or that they feel "cut off" from their bodies due to an injury, illness, or other distress. As illustrated in the passage from Dr. Howell, diagnoses like DID or other dissociative disorders refer to a more rigid separation of this very natural part of the human condition [2].
There have been many advances in better understanding trauma and dissociation through a neurobiologic lens. While this section will conclude with some of that research, it is important to obtain a basic understanding of the human brain and how unhealed trauma can impact its functioning. The simplest explanatory model that seems to work the best for clinicians to gain this understanding is the triune model of the human brain, originally developed by psychiatrist Paul MacLean [5]. It is important to note that some view this way of approaching the brain as overly simplistic, with some going so far as to say it is debunked [47]. However, many neuroscientists continue to support the model as a good basis of organizational explanation for most trauma therapists. Many modern scholars (e.g., Bessel van der Kolk, Daniel Siegel) continue to use it as a base of explanation.
The triune brain model espouses that the human brain operates as three separate brains, each with its own special roles—which include respective senses of time, space, and memory [5]:
The R-complex or reptilian brain: Includes the brainstem and cerebellum. Controls instinctual survival behaviors, muscle control, balance, breathing, and heartbeat. Most associated with the freeze response and dissociative experiences. The reptilian brain is very reactive to direct stimuli.
The limbic brain (mammalian brain or heart brain): Includes the amygdala, hypothalamus, hippocampus, and nucleus accumbens (responsible for dopamine release). The limbic system is the source of emotions and instincts within the brain and responsible for fight-or-flight responses. According to MacLean, everything in the limbic system is either agreeable (pleasure) or disagreeable (pain). Survival is based on the avoidance of pain and the recurrence of pleasure.
The neocortex (or cerebral cortex): Contains the frontal lobe. Unique to primates and some other highly evolved species like dolphins and orcas. This region of the brain regulates our executive functioning, which can include higher-order thinking skills, reason, speech, and sapience (e.g., wisdom, calling upon experience). The limbic system must interact with the neocortex in order to process emotions.
Many strategies in the psychotherapeutic professions work primarily with the neocortex. For a person with unprocessed or unhealed trauma symptoms, the three brains are not optimally communicating with each other when the limbic system gets triggered or activated [6]. During periods of intense emotional disturbance, distress, or crisis, a person cannot optimally access the functions of the neocortex because the limbic, or emotional brain, is in control. In essence, a dissociative phenomenon occurs. Blood flow slows to the left prefrontal cortex when the limbic system is triggered to some degree. Thus, a person may be aware of what is happening around them, and yet that disruption or dissociation from the brain's innate totality impedes a person's capacity to process or make sense of it.
Consider these examples that may be familiar to your clinical practice: Have you ever tried to reason with someone in crisis? Have you ever asked someone who has relapsed on a drug or problematic behavior, "What were you thinking?" Have you ever tried to be logical with someone who is newly in love or lust? Attempting any of this is like trying to send an e-mail without an Internet signal. You may have awesome wisdom and cognitive strategies to impart and you can keep clicking send, but the message is not ever going to get through. Moreover, because the activated person has awareness, they may grow increasingly annoyed by persistence, which can activate the limbic responses even further.
Triggers are limbic-level activities that cannot be easily addressed using neocortical interventions alone. If a stimulus triggers a person into reaction at the limbic level, one of the quickest ways to alleviate that pain/negative reaction is to feed the pleasure potential in the limbic system. As many traumatized individuals discover, alcohol use, drug use, food, sex, or other reinforcing activities are particularly effective at killing/numbing the pain. For children growing up in the high distress of a traumatic home, dissociation can become the brain's natural and preferred way to escape the pain. Cultural commentators and scholars have referred to dissociation as a "gift" to the traumatized child for this reason [7].
Dissociation, trauma-related disorders, and addiction are inter-related because dissociation is a defense that the human brain can call upon to handle intense disturbance. People dissociate in order to escape—to sever ties with a present moment that is subjectively unpleasant or overwhelming, stemming from unhealed trauma and its impact. In referencing the triune brain model, dissociative responses—often conceptualized as similar to freeze responses—are even deeper than the limbic brain, taking place in the R-complex or brainstem [8]. This is a testament to their primary, protective quality.
Precise neurobiologic explanations of dissociative phenomenon are still being investigated, and understanding remains incomplete. In their comprehensive review, Krause-Utz, Frost, Winter, and Elzinga summarize that there is a suggested link between dissociative symptoms and alterations in brain activity associated with "emotion processing and memory (amygdala, hippocampus, parahippocampal gyrus, and middle/superior temporal gyrus), attention and interoceptive awareness (insula), filtering of sensory input (thalamus), self-referential processes (posterior cingulate cortex, precuneus, and medial prefrontal cortex), cognitive control, and arousal modulation (inferior frontal gyrus, anterior cingulate cortex, and lateral prefrontal cortices)" [9]. Electrical neuroimaging studies show a correlation between the temporoparietal junction—an area involved in sense of self, agency, perspective taking, and multimodal integration of somatosensory information—and dissociative symptoms, and specific forms of dissociation are connected with brain areas in question [10].
While the neurobiologic implications of dissociation are discussed in detail later in the course, this section has endeavored to give enough base knowledge to understand that trauma and dissociation are inter-related. Basically, dissociation can be described as an inherent mechanism of the human brain that can be called upon to manage distress. The higher the degree and the more intense the trauma, the greater the likelihood that some aspects of dissociation, whether clinically significant or not, can manifest. Dr. Paul Miller, a psychiatrist based in Ireland, cautions against reducing the phenomenon of dissociation down to one thing happening in the brain [48]. A variety of mechanisms in the complex human brain can leverage dissociation to protect, to get needs met, and to keep people alive when they are traumatized, especially when they are living in states of chronic, complex trauma.
Dissociative identity disorder or DID, formerly referred to as multiple personality disorder, can make for fascinating plot points and opportunities for characterization in the media. Unfortunately, these media portrayals have fed perpetuated myths and misconceptions about dissociative disorders that persist in the general public and in mental health professions. In many cases, the media only showcases the most extreme or sensationalized cases of DID [11]. Many clinicians do not realize that their clients are experiencing distress that can be described through the lens of a dissociative disorder because their clients are not presenting with symptoms that look as extreme or severe as the largely fictionalized Sybil or the highly sensationalized portrayal in the 2016 film Split. If clinicians are only using these media portrayals as their point of reference, they may be unnecessarily frightened to treat their dissociative clients, fearing violence, self-injury, or other expressions they may not feel prepared to handle.
Many individuals who dissociate express trepidation about making their condition known to the general public; this can even include fear about coming out to one's partner or one's therapist in fear of judgment. For example, I, a mental health professional active in addiction and trauma care, found "coming out" fully as a person with a dissociative disorder was much scarier than being out as someone in recovery from addiction or being out as a bisexual woman. There was a great fear that I would no longer be taken seriously, especially among professional colleagues, if I was public and open about my experiences.
In 2010, Jaime Pollack started the Healing Together Conference with the goal of providing survivors of complex trauma who identify as having a dissociative disorder a place where they could feel safe enough to share freely. Pollack and others did not feel welcome to share from personal experience as non-clinicians at professional conferences that address trauma and dissociation. Even professional clinicians have experienced a similar sense of disregard for the lived experience. Spaces like Healing Together give people with dissociative disorders from a variety of professional backgrounds a chance to be open and share freely, something that can be a rarity in this world.
There is a variety of myths and misconceptions regularly encountered from clinical professionals and from colleagues who also work as trauma trainers. The most common are the usual fears about people with dissociation acting out and causing harm to self or to others, although clinical experience and evidence suggests that there is no more risk of these behaviors than with other diagnoses [12]. The next set of myths revolves around treatment. There can be a sense that people with clinically significant dissociation, especially DID, do not respond well to treatment and cannot live full and functional lives. In many cases, professionals who hold such myths generally do not have enough grounding in trauma-informed or trauma-focused care to realize the connection between unhealed trauma and the successful treatment of maladaptive dissociation. The other major treatment myth is that for successful treatment of DID or another dissociative disorder to occur, there must be an integration of the various alters or parts into one presenting person. While this is discussed further in the section on treatment, for the time being, please know that many exist functionally and adaptively with the help of their system, and integration in the simplistic sense is never achieved—nor does it need to be.
Many individuals with DID or other dissociative disorders do not shun the word integration, but instead view integration as a healthy sense of cohesion or communication between the system. The term working wholeness may be preferred. However, when working with a client with dissociation, integration can be quite a triggering word, because previous providers may have used the term incorrectly or abusively, making them believe that they must integrate if they want to live a normal life. This can cause upheaval in the system, especially if more vulnerable parts believe they are going to be forced out. Consider this metaphorical comparison: For many years the United States was referred to a "melting pot" of sorts, suggesting the people from various backgrounds came together and blended. This metaphor has garnered criticism because a melting pot suggests that various peoples come together, melt down, and then a single, ideal alloy of an "American" emerges. While some people would like this to be so, it is neither culturally inclusive nor sensitive. An alternate metaphor refers to the United States as a salad or a bowl of stew, indicating that each ingredient brings their own unique flavor while contributing to the whole. This metaphor is also workable when referencing dissociative systems.
Many individuals with clinically significant dissociative disorders do not reach the "integration" debate stage of treatment with their providers because many mental health providers are not willing to take on their cases. Screening out for dissociation and making referrals is very common, leaving many with a message that they are "too much to handle." Often, individuals with dissociative disorders can be prematurely admitted into psychiatric facilities at the mention of self-harm or blanking out time. While clinical professionals should not go against their ethical training if there is a viable intent or a plan articulated for injury to self or others, bear in mind that suicidal ideation and self-harm can be a very normal complex trauma response and part of one's dissociative profile. In some cases, having these feelings normalized and a viable plan for addressing them developed is insufficient. Yet, many individuals who struggle with dissociative issues will not articulate struggles to their providers out of fear of being committed to an institution, which can be an unsafe place for someone with a dissociative disorder. Perhaps the biggest misconception in the mental health field is that dissociation is not real, does not exist, or, if it does, is extremely rare. Not only is this an invalidating experience for individuals, they can end up receiving a host of other diagnoses that result in excessive or improper pharmacotherapy. To understand more about the invalidation factor, please read on to the next section, which discusses historical perspectives on dissociation, how to treat it, and how to diagnose it.
The issue of dissociation and how to diagnose it has been historically shrouded in controversy in the psychological and helping professions, largely because trauma can make people uneasy. Giving people, especially children, trauma-related diagnoses can be an uncomfortable matter. When a child gets a diagnosis like attention deficit and hyperactivity disorder (ADHD) or bipolar disorder, the implication and suggestion of the medical model is that something is impaired with their brain. Medications, although often prescribed in concert with some kind of behavioral therapy, are typically emphasized as the solution. However, when a child receives a trauma-related diagnosis, generally someone is responsible—a parent or guardian who exposed them to harm, the school system, or even society at large. This meanders into uncomfortable territory for many people. Further, most medications used in the treatment of dissociative disorders focus on comorbid symptoms (e.g., depression, anxiety); psychotherapy remains the cornerstone of treatment.
Although clinically significant dissociation can develop in adulthood as a response to trauma or other distress, its etiology is usually traced to significant, complex trauma in early childhood. Often, this trauma is of a developmental nature, meaning that it happened when a child was still vulnerable and often involved betrayal by someone they loved or trusted. Useful distinctions between trauma as an incident or event (typically associated with the PTSD diagnosis as presented by the DSM) and complex or development trauma is that complex trauma experiences [13]:
Are repetitive or prolonged
Involve direct harm and/or neglect or abandonment by caregivers or ostensibly responsible adults
Occur at developmentally vulnerable times in the victim's life, such as early childhood
Have great potential to severely compromise a child's development
Initially, even Freud seemed to be convinced of trauma's impact in his early investigation of dissociative phenomenon. As is well-established in the history of psychology, widespread pressure from his influential colleagues resulted in Freud backing down from this hypothesis and instead focusing more on repression and subconscious desires as etiology for mental and emotional disorders. The gendered label of hysteria was put into wide use, a construct that modern trauma scholars now view as a manifestation of complex trauma and dissociation [14]. Much of the early thinking in the field, especially from Pierre Janet, suggested that there is an element of dissociative phenomenon in all mental and emotional disorders, even conceptualizing what would come to be known as schizophrenia through this lens [12]. Other French colleagues of his era proposed similarly.
The dissociative disorders formally debuted in the DSM-III in 1980. The PTSD diagnosis also appeared in that edition as an anxiety disorder, but dissociative disorders were presented as a separate category. Although new to DSM-III, their discussion and inclusion were not new to the field [15]. With every iteration of the DSM since then, up to the current DSM-5, there has been intense debate and scrutiny over the dissociative disorders as being worthy of inclusion. In reality, many leaders of the field, especially those on DSM work groups, openly doubt their existence [16]. The purpose of this course is not to engage in this debate—clearly the position of this course is that dissociative disorders do exist and are potentially more widely prevalent than once thought and reported. However, major medical and psychological groups continue to report that dissociative disorders are extremely rare. This approach to dissociative disorders and resistance to their existence is borne from the same discomfort about trauma and responsibility that Freud encountered in the early days of his work. Although the general phenomenon of dissociation can show up in a wide array of clinical diagnoses, it has been established that unhealed trauma is a major etiologic factor in the development of clinically significant dissociative disorders [17].
Clinicians interested in reading more about the history and debate around dissociation, trauma, and memory are directed to Anna Holtzman's article exploring the "memory wars" in the field of psychology, written in the wake of the Harvey Weinstein trials (Resources). The memory wars refer to decades of debate in the field about the trustworthiness of memory, particularly as it relates to accusations of abuse by survivors of trauma. She discusses the history of the False Memory Syndrome Foundation, founded by the parents of Dr. Jennifer Freyd (a former president of the International Society for the Study of Trauma and Dissociation [ISSTD]). Dr. Freyd accused her parents of abuse and their response was to establish an organization to discredit survivors of abuse.
As long as unhealed trauma continues and people are threatened by its impact or made to feel responsible for it, there is a likelihood that such debate, even in scholarly settings, will continue. The general state of the evidence suggests that not only are dissociative disorders real, the prevalence is higher than previously thought [18].
While the ISSTD and mainstream advocates in the field of dissociation have promoted research and scholarship to prove that dissociation exists, there is a concern by advocates that such a focus may measure the experiences of survivors without adequately including their voices into the advocacy. In the spirit of both/and, this course acknowledges that while scholarship and research are always critical to validate constructs in the mainstream, clinicians can get overwhelmed by trying to study dissociation in this manner. Normalizing dissociation as a human phenomenon and describing how trauma and distress can impact its manifestations should also be a part of the discussion moving forward.
Because dissociation can be explained as a coping device that crosses the line to being a maladaptive symptom for some individuals, it can be contended that trauma-associated dissociation manifests in a variety of clinical diagnoses. In this section, the primary diagnoses categorized in the Dissociative Disorders chapter of the DSM-5 are presented [19]. However, remember that these are not the only places where dissociation may show up diagnostically. Substance use and other disorders, for instance, have a strong dissociative component, and these will be handled separately in another section. There is also a great deal of confusion about where the line exists between distraction (that might be more commonly associated with diagnoses like ADHD, but can also appear in clients with PTSD) and dissociation. Moreover, in the most recent updates to the DSM, there is a new subtype of PTSD that specifically addresses dissociation, which will be included in this section.
For an individual to meet any of the diagnostic criteria that follow, dissociation must not be better explained by a phenomenon like intoxication. Thus, it becomes imperative for clinicians to understand the intricacies of how trauma and dissociation manifest, because many different diagnoses may be on the proverbial table for consideration.
The following sections have been reprinted with permission from The Infinite Mind [20]. These summaries are clinically sound (reflecting what appears in the DSM-5) while also being written in a language that the general public will likely find friendly.
DID, formerly called multiple personality disorder, develops as a childhood coping mechanism. To escape pain and trauma in childhood, the mind splits off feelings, personality traits, characteristics, and memories into separate compartments which then develop into unique personality states. Each identity can have its own name and personal history. These personality states recurrently take control of the individual's behavior, accompanied by an inability to recall important personal information that is too extensive to be explained by ordinary forgetfulness. DID is a spectrum disorder with varying degrees of severity. In some cases, certain parts of a person's personalities are aware of important personal information, whereas other personalities are unaware. Some personalities appear to know and interact with one another in an elaborate inner world. In other cases, a person with DID may be completely aware of all the parts of their internal system. Because the personalities often interact with each other, people with DID report hearing inner dialogue. The voices may comment on their behavior or talk directly to them. It is important to note the voices are heard on the inside versus the outside, as this is one of the main distinguishers from schizophrenia. People with DID will often lose track of time and have amnesia to life events. They may not be able to recall things they have done or account for changes in their behavior. Some may lose track of hours, while some lose track of days. They have feelings of detachment from one's self and feelings that one's surroundings are unreal. While most people cannot recall much about the first 3 to 5 years of life, people with dissociative identity disorder may have considerable amnesia for the period between 6 and 11 years of age as well. Often, people with DID will refer to themselves in the plural [20].
The most common of all dissociative disorders and usually seen in conjunction with other mental disorders, dissociative amnesia occurs when a person blocks out information, usually associated with a stressful or traumatic event, leaving him or her unable to remember important personal information. The degree of memory loss goes beyond normal forgetfulness and includes gaps in memory for long periods of time or of memories involving the traumatic event [20].
Having depersonalization has been described as being numb or in a dream or feeling as if you are watching yourself from outside your body. There is a sense of being disconnected or detached from one's body. This often occurs after a person experiences life-threatening danger, such as an accident, assault, or serious illness or injury. Symptoms may be temporary or persist or recur for many years. People with the disorder often have a great deal of difficulty describing their symptoms and may fear or believe that they are going crazy [20].
Symptoms of unspecified dissociative disorder do not meet the full criteria for any other dissociative disorder. The diagnosing clinician chooses not to specify the reason that the criteria are not met [20].
The other specified dissociative disorder category is used in situations in which the clinician chooses to communicate the specific reason that the presentation does not meet the criteria for any specific dissociative disorder [20].
Many experts have expressed confusion that dissociative disorders were separately categorized instead of being included in the DSM-5-TR chapter grouping trauma- and stressor-related disorders. This may reflect some of the controversy and misunderstanding about dissociative disorders, or a lack of cohesion among the work groups that determine the categories in the DSM.
The chapter of trauma- and stressor-related disorders (which includes PTSD, acute stress disorder, adjustment disorders, reactive attachment disorder, and disinhibited social engagement) does make mention of dissociative symptomology as a potential feature of PTSD. In the DSM-5 version of the PTSD diagnosis, there is a qualifier option of PTSD with predominant dissociative symptoms. Dissociation can play out in all five symptom areas of the PTSD diagnosis, with flashbacks (under Criterion B, intrusion) specifically being described as a dissociative phenomenon. In DSM-5, depersonalization is defined as "persistent or recurrent experiences of feeling detached from, as if one were an outside observer of, one's mental process or body" (potentially an avoidance or negative mood/cognition manifestation) [19]. Derealization is defined as "persistent or recurrent experiences of unreality of surroundings" (potentially a part of the PTSD symptoms of intrusion, avoidance, or negative mood/cognitions) [19]. Although depersonalization and derealization still appear as their own diagnoses in the dissociative disorders category, those diagnoses should be ruled out if PTSD is the better explanation.
This is a gray area to navigate diagnostically, particularly because people struggling with clinically significant dissociative disorders likely meet the criteria for PTSD. With PTSD long being conceptualized as a more event-centric diagnosis that does not accurately encapsulate the depth of complex trauma, this qualifier may be more appropriate for adults who experience a traumatic event not connected to childhood or developmental trauma and develop these dissociative tendencies as a result.
The Dissociative Profile is a process used to evaluate and become aware of one's own tendencies to dissociate, both adaptively and maladaptively, and identify best strategies for directing one's knowing awareness back to the here and now. Therapists and helping professionals should first know their own dissociative profile and by doing this, will help clients to investigate their own [21]. This exercise is not only valuable as an exploratory device—the knowledge gleaned from it can become a valuable part of treatment planning, especially in managing distress that may rise between sessions. This approach is presented prior to discussion of formal psychometric measures with the intent that a general understanding and ability to identify association will help you truly understand these psychometrics and how to use them.
Before engaging in this exercise, please remember that every human dissociates; it is natural and normal. This is not intended to be an exercise in shaming; rather, it should focus on self-inquiry. To engage in the Dissociative Profile exercise, take the following steps, using the sample Dissociative Profile (Table 1) as a guide as needed.
SAMPLE DISSOCIATIVE PROFILE EXERCISE
| My Dissociative Tendencies | What Helps Me Return to Present Moment |
|---|---|
| Daydreaming when I'm bored. This was adaptive when I was a kid; it's how I survived my parents' fighting. Somewhat of a problem/maladaptive now, as it can keep me from paying attention at work or with the kids. | Telling myself to "snap out of it" helps sometimes. This is something I'd like to work on though, because it can be hard to get out of the dream world. |
| Playing too much Candy Crush on the phone. Boredom also seems to trigger this. Doesn't seem to be a problem at the level of addiction or anything; I just know I do it. | Sometimes my eyes get too strained or tired, and that helps me put it down. When I know I have something more exciting/stimulating to work on, I stop. This can include having a conversation with people I enjoy. |
| Saying "it's no big deal" to my own therapist whenever I get too emotional. It's clear that this protected me at home growing up (adaptive), but I know it gets in the way of me doing deeper work | Having my therapist, who I fundamentally trust, gently call me out on it seems to help. When she can guide me through one of her mindfulness exercises encouraging me to notice my body and sit with whatever is coming up, I make steps in the right direction. |
| Problems paying attention when I drive (only sometimes). I'm not sure if this is dissociation or just general distraction. Either way, it does seem to happen when I'm overwhelmed. | Playing music I like in the car helps. I haven't yet taken my therapist's suggestion of taking a few deep breaths before I start driving regardless of how I'm feeling; perhaps I should try that. |
Take out paper or open up a word processing program on your computer. Make two columns. Title the left-hand column "My Dissociative Tendencies," and title the right-hand column, "Strategies for Returning to the Present Moment."
Take as much time as you need to make a list of the ways in which you tend to dissociate—this can be general patterns like "zoning out or daydreaming when I'm bored," or "spending time on Facebook wondering what everyone else is doing." You can take this inventory a step farther by noting if these strategies or behaviors are adaptive, maladaptive, or both (depending on context). Also note, perhaps, how often you engage in these dissociative strategies and if you have knowing awareness about what triggers them (e.g., boredom, emotional pain, overwhelm, conversations with certain people).
After the left column feels complete, go to the right column and beside each item on the left, make some notes about what helps you return to the present moment when you need to. This can be more intrinsic skills (e.g., my mindfulness practice, especially grounding with solid objects), or more externally motivating factors (e.g., hearing my child call out that they need me). Remember that this is not an interrogation; it is simply a true assessment of where you stand. You are also free to be honest and note that you are not sure yet how to draw yourself back to present moment awareness when you get stuck in certain patters.
After finishing your own dissociative profile, take a moment to notice whatever you notice. Is there anything that surprises you? Is there anything you ought to consider sharing with your own therapist, friend, partner, or members of your support system? How can you use what you discover here to assist you in your own personal development and goals or intentions for healing, whatever those may be?
If you are guiding a client through this exercise, be open to debriefing their discoveries with them and developing a plan of action. This can form a solid base for engaging in treatment planning. Moreover, many trauma-focused approaches to therapy stress the importance of having a skills-and-strategies plan for between sessions so the client stays as safe as possible, especially if distress arises in between sessions. Engaging in the Dissociative Profile exercise gives you and your client a general sense of where they stand in terms of existing adaptive skills, and what they need to build for more adaptive engagement with the present moment.
The introduction and first section of this course are designed to provide a foundation to understand the phenomenon of dissociation and how it manifests in the human experience. With this foundation in place, this section seeks to take you deeper into some of the tools, models, and strategies that may be useful in clinical settings to optimally work with dissociation. These may also help to inform treatment planning, which is covered in a later section of the course.
There are a variety of psychometrics and clinical interview guides available for clinicians to help in their identification of dissociation. It is important to keep in mind, as a trauma-focused clinician, many of these devices may be too interrogatory, Use good clinical judgment about whether some of these scales or measures are a good fit for your practice and your clients. They have all played a role in research and helping to validate the existence of dissociative disorders. However, taking a test for a psychometric evaluation can be triggering in its own right and can lead to a sense of confusion in a person's system if they are not properly guided.
At a minimum, clinicians should be familiar with the Dissociative Experiences Scale (DES), developed by Eva Bernstein Carlson and Frank Putnam [22]. This is a screening device, not a pure diagnostic evaluation, so a clinical interview will be necessary in order verify a diagnosis. Even as a screening device, the DES can be a conversation starter and vehicle for investigation, regardless of a person's specific diagnosis. The DES is a 28-item screen in which people are asked to give a general impression of how often they engage in a certain behavior or activity that can be potentially dissociative. Sample items include [22]:
Some people have the experience of driving a car and suddenly realizing that they don't remember what has happened during all or part of the trip.
Some people sometimes have the experience of feeling as though they are standing next to themselves or watching themselves do something as if they were looking at another person.
Some people sometimes find that they become so involved in a fantasy or daydream that it feels as though it were really happening to them.
In the DES-II, people taking the evaluation rate these items by percentage (e.g., this happens to me about 20% of the time). In the DES-III, a basic 0–10 scale is adapted that corresponds with percentages; both versions are approved for clinical use.
To get an average score on the DES-II, you add up the total number of percentages and then divide by 28 (the number of items on the evaluation). Anything above 30% is generally considered to be cautionary for a clinically significant dissociative disorder. Anything greater than 40% is generally considered to be in the range of a clinically significant dissociative disorder. The DES is a starting point for clinicians and clients alike who are not familiar with addressing dissociation. Of course, nothing significant occurs at 30% or 40%; these are simply meant to be a guide for further diagnostic evaluation. One concern is that training programs in specialty therapies that use the DES to screen for dissociation can promote fear. For example, in the EMDR therapy community, some programs can promote the idea that people with a DES score greater than 30% are not appropriate candidates for EMDR or other types of deep trauma work. This is another of the myths and misconceptions. If the DES is greater than 30%, precautions should be taken and therapists can use the information gleaned from the DES to obtain a better sense of a person's relationships to dissociative responses based on their trauma.
After a client takes the inventory (preferably in office, so a therapist is available if they have any questions or concerns or get triggered), review the high item responses with them (greater than 30% to 40%) and ask them to talk more about when they started noticing that response over the course of their life and how it plays out for them presently. You may also ask if they notice how the specific behavior helps them to cope in any way. This information is more valuable, both in diagnosis and treatment planning (which also includes between-session safety planning) than any specific number.
In the spirit of getting to know one's own dissociative profile and relationship with dissociation, clinicians should take the DES for themselves first. It can be scored, but it may be more valuable to investigate how some of the higher scoring items fit into the Dissociative Profile exercise completed in the previous section. Other psychometrics in use clinically include:
Structured Clinical Interview for Dissociative Disorders (SCID-D)
Dissociative Disorders Interview Schedule (DDIS)
Multidimensional Interview of Dissociation (MID)
Many of these tools are available online (Resources).
One of the classic concepts and articles in the field of dissociation studies is Fraser's Dissociative Table Technique. This concept was key to introducing the idea that a person with dissociative parts could get to know their system and how the various parts inter-relate with each other. Publication of Fraser's seminal article led to the popularization of the "conference table" metaphor for individuals with dissociation mapping out their parts and how they inter-relate. Fraser introduces a variety of other metaphorical possibilities as well for this mapping, with an emphasis that the table metaphor is only one part of his larger technique [23,24]. In his core article, he discusses the use of the following approaches that make up the Dissociative Table exercise [23]:
Relaxation imagery: Using guided imagery as preparation and resourcing.
Dissociative table imagery: Presented as the most important component of the exercise, this involves using the principle of imagery for a client to begin seeing their internal system take seats around a table (with modifications if tables feel unsafe). He credits this as a Gestalt-based technique.
Spotlight technique: Sets up the idea of the spotlight being shined on the alter (or part) that is directly speaking to the therapist (with modifications if the light feels unsafe).
The middleman technique: Establishes a system of communication between the alters or parts whereby one can speak on behalf of several others. This technique addresses the concept of co-consciousness, referring to two or more parts/alters sharing consciousness at the same time (not blacking out, "going away," etc.).
Screen technique: A distancing technique whereby distressing memories can be viewed as if they are on a screen in the same room as the table.
Search for the center ego state (inner self-helper): Establishing or revealing what may be referred to as the "core self" of the presenting self that has the strongest overview/sense of the entire system. This may be referred to as the presenting adult or the core self. Some controversy exists over whether or not it is necessary for some dissociative systems to have a center ego state.
Memory projection technique: Another technique for furthering communication between the various alters/parts and their memories, using the various parts to bring in resources as other states may work to process or heal other memories on the screen.
Transformation stage technique: A technique that can be used to transform a person's relationship to the memory and how they see themselves in the memory in terms of time, space, and age.
Fusion/integration techniques: Although there is some controversy and trigger potential around integration in these techniques (as discussed previously), Fraser ultimately seems to be an advocate of integration using some of these fusion points as stepping stones.
The original article is a vital source of information for those interested in working more deeply with dissociation (Resources). Although it has its flaws, Fraser's Table can be a good starting point for clinicians who want direction on how to work with a system. The piece is also important because Fraser advocates for the reality of dissociation and how to work with it. He also addresses one of the controversies around dissociation—the idea that the therapist inserts parts or alters and their memories. While clinicians can guide people into identifying their own system and understanding how it works, it is vital that they do not force agendas and ideas on a person about what is happening. In EMDR therapy, there is a concept of therapists staying out of the way as much as possible and viewing themselves as facilitators or guides. Such an attitude is very helping, regardless of orientation, in helping people work with and identify their parts.
While Fraser's Table is arguably one of the most popular approaches in the first wave of dissociation studies following the formal introduction of dissociative disorders into the DSM-III, the Theory of Structural Dissociation, developed by Onno van der Hart, Ellert Nijenhuis, and Kathy Steele, has become the focus of dissociation studies in the 21st century. Many trauma-focused professionals are advocates of this theory because, at its heart, it is nonpathologizing, positing that everyone is born with a fragmented or dissociative mind [25]. This is normal for infants, who get their various needs met in the absence of speech, language, or a more developed neocortex. Healthy development is defined by needs being consistently met engendering a natural integration of the personality structure. Yet, in the presence of unhealed trauma, disorganized attachment or developmental distress, a natural separation can remain.
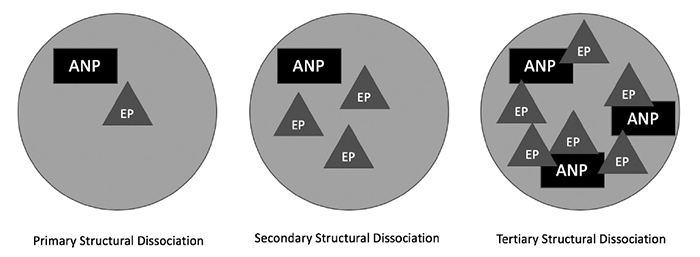
The two main terms used in the Theory of Structural Dissociation are apparently normal personality (ANP), which is similar to Fraser's idea of the center ego state, and emotional part or personality. Emotional parts remain to protect or to meet a need, and some systems contain a more complicated interconnection of emotional parts and ANPs than others. While this is a bit of an oversimplification of how structural dissociation plays out systemically, it gives people new to this theory a good frame of reference. The model also makes use of the terms primary structural dissociation (which is more likely to be used in relation to PTSD and other trauma-related disorders), secondary dissociation (mainly related to personality disorders, dissociative disorders other than DID, and complex PTSD or developmental trauma), and tertiary dissociation (classically presented as DID). Figure 1 provides a visual presentation of how this may play out.
The Theory of Structural Dissociation is certainly not without criticism. For example, psychiatric leader in the field of dissociation Dr. Colin Ross proposed an extensive modification to the theory. In his modification, Ross proposes that an emotional part does not have to be separate entities in and of themselves; instead, they can hold a fragment or experience like a thought, feeling, memory, or sensation. In this modification to the model, he expands on the Janetian idea that many disorders can be viewed through the lens of dissociation and that the idea of parts can be used as treatment conceptualization for conditions like substance use disorders and compulsive behaviors.
The theory of structural dissociation is a step in the right direction, and Ross' modifications expand the scope of what is possible and gives more permission to modify, which is essential in any facet of trauma-focused care. If rigidly interpreted, the original model is too inflexible, which is dangerous when applied to the phenomenon of systems that is fundamentally fluid and unique to the individual. Another consideration is the potentially offensive use of the adjective "normal" to describe the core self or presenting adult (ANP). This speaks to a reality of care in helping people to identify and to get to know their system; part of this is helping them to identify the terminology that best works for them and their understanding.
Over the past several years, there has been increased criticism of the Theory of Structural Dissociation, with one lived experience advocate contending that it is ablelist [49]. While it may stand as a decent explanatory model, especially when modifications are made, adherents to the theory of structural dissociation may have fear of treating people with DID. There is a fear that talking to emotional parts directly is somehow doing a disservice to people with dissociative identities. Some find that the use of this or any model to encourage people with dissociative identities to "hold it all together" is inherently problematic. Speaking from my lived experience, the prouder that I got of my parts and having them and feeling like I could share about them more openly and freely, my mental health ultimately improved.
In working with clients with dissociation and identifying your own dissociative tendencies, clinicians can lean into the metaphorical possibilities that people can develop as they endeavor to understand their systems and how they work. Fraser's metaphors are a solid start, and the circles and shapes often used to represent structural dissociation are a good jumping off point. However, because creativity and expression are part of what defines the dissociative mind, using more creative metaphors may be better serving to you and to your clients [21].
Consider Ms. M, a client with an unspecified dissociative disorder. Ms. M is aware of a very defined inner world before coming into therapy, an inner world that she describes as a series of eight parts, all with their own name and purposes. Ms. M is delighted and surprised when her new therapist allows her to reference her parts and talk this way about them, as previous therapists discouraged her from using this language and conceptualization to refer to herself. "Show up as the adult," is something she heard more times than she ever cared to count.
The therapist asks Ms. M if she sees her parts in any specific way, and she answers immediately—"Yes, I see them as a dollhouse!" She goes on to describe that each part has their own room, and that when she wants them to come together and have a discussion, she senses that they all meet in the living room for a gathering of sorts. They use this mapping of her system as vital information in developing her treatment plan and approach. Interestingly, Ms. M did not require assistance in developing this metaphor—it was already innate within her, and she just needed permission and space to speak it. Other clients may require more of a guide or some examples to help them map out their parts and how they interplay within a system. This can be a creative exploration to understanding the self whether or not a person has a clinically significant dissociative disorder. Other metaphorical possibilities include:
A car or van
A circle of people, like you see in group therapy or a 12-step meeting
Balloons
Bouquet of flowers
An orchestra or band
Salad or stew
Mosaics
Hindu gods
Gathering of saints
The elements (i.e., earth, air, water, and fire)
Keys on a ring
Movie references (e.g., the houses used in Harry Potter, ensemble pieces like Star Wars, Guardians of the Galaxy, Black Panther, orThe Wizard of Oz)
Other pop culture references (e.g., television shows, songs on a playlist, characters from literature)
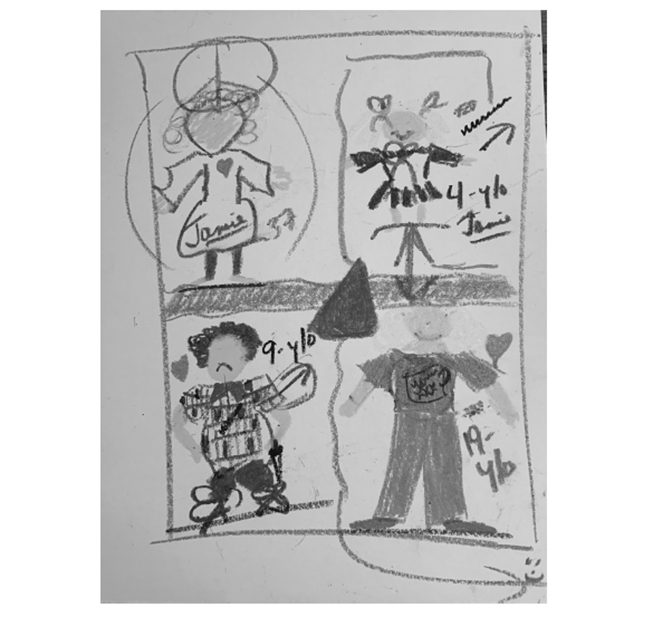
Figure 2 is an example of how visual representation or other art work can be used to help a person identify the parts of their system and how the inter-relate.
The example in Figure 2 is from my own healing journey. I find the car or the van to be a particularly useful metaphorical construct for helping me (and others) to understand my system and how the parts inter-relate. The way I know myself, my presenting adult or core self is always driving the car. However, if the various parts that ride along with me— who I call 4, 9, and 19 (representing their ages)—are not getting their needs met or are not being listened to, they can start to act out or withdrawal in the car. For me, they usually do things like tap on my shoulder, pull my hair, or scream until I pay attention to them and what they are trying to tell me. During an earlier period of my own healing, when the 4-year-old state had some serious healing work to do, it literally felt like she was sneaking behind me and covering my eyes with her hands just so I would pay attention to her. Clearly that caused some distress in my life, and I was not able to return to a place of equilibrium and optimal functioning until I engaged in therapeutic work that helped to heal the four-year-old, the actual age when my own traumatic experiences intensified. If you have ever been on a road trip with children, you know that keeping the peace can be a delicate balance. That is what my mind feels like when I am not listening to the consensus of my system. My 9-year-old part, for instance, is now good about telling us when we need to pull over and take a break. Although she originally developed as the part that held destructive behaviors like self-injury and suicidal thoughts, she has become the voice, in our healing, that tells us when we need to take care of ourselves. I have also used my 19-year-old part as a middle-woman of sorts (using the Fraser term) to broker peace between the 4 and 9 year old, who can annoy each other. Although 19, who has a babysitter quality, can be good at this, she has recently become very good at telling me when this tires her out too much and she needs her own space. Interestingly, I experienced a series of traumatic losses and also crossed the threshold into active addiction at 19 years of age, which is why she emerged or stayed around as a separate emotional part in my system. In healing, I have come to appreciate 19 as a strong, rebellious spirit who started to question the norms in which she was raised. Though this naturally brought about some distress for her, healing from this distress has helped to heal our whole system.
I hope this personal look at a few metaphorical possibilities has been helpful to you as you begin to conceptualize systems and parts work.
Some clients will develop names for their parts, some will refer to them just as numbers or ages (as in the related experience), and others will refer to them just by descriptive qualities (e.g., my angry side, my soft side, the shame part, the inner child). Before beginning work with people using Fraser's Table, mapping in the spirit of structural dissociation theory, or one of these more creative metaphors, clinicians are encouraged to first do some mapping of their own internal system. In essence, this is an important continuation of the Dissociative Profile exercise.
To do this, first spend some time brainstorming, preferably writing down, how you see the parts of yourself. Remember that if you are stuck and nothing you are reading here resonates, you can use the basic presenting adult/inner child construct. If that is the case, how do you see them inter-relating? Staying with the idea of the table, perhaps you simply imagine them sitting down to interact over a cup of tea (or maybe your adult drinks the tea and you pour lemonade for the inner child).
Using paper and whatever basic art supplies you might have on hand (or even just a pen or pencil), begin to map how you see your internal system inter-relating. Doing this exercise does not diagnose you with a dissociative disorder. We all have parts, and seeing ourselves in this way can be a useful strategy for conceptualizing.
This exercise is not about being an outstanding artist—you are not being graded or judged. Simply think of this as drawing out a rudimentary map (and for that matter—the "map" itself could be another useful, metaphorical example). Some people like to use the idea of a circle (e.g., in some cases using plain white paper plates) as the backdrop for how they map out their system.
Take as much time as you require to complete the exercise. When you are though, consider journaling/writing some impressions or sharing them with a friend or colleague. What have you learned about how the various parts of your system inter-relate? Where is there room for a greater sense of communication or understanding in your system? Are there any blocks that are apparent to communication, cohesion, or wholeness?
An exercise like this offers creative, client-centered insight into working with parts or mapping a system, and it may certainly be used with clients, especially in the early stages of working together. What you learn here can phenomenally inform your strategies for treatment planning, which is covered in a later section. Perhaps you are already beginning to understand that what works for one part of the system for resourcing and healing may be different than what other parts in the system require. This will be valuable information for moving forward with treatment.
The addiction treatment field is making steady steps toward becoming more trauma-informed, but a deficit in professionals' ability to identify signs and symptoms of dissociation persists [26]. This is a problem, especially because of the strong interplay between dissociation and addiction. Many clients will be unaware of dissociative symptoms experienced in childhood because drinking and using drugs can become their dissociative outlet in adulthood. Specific dissociative symptoms (e.g., "zoning out" at work or when emotionally overloaded) can develop in sobriety, and will require trauma-focused treatment. This phenomenon is relatively common in recovery circles, but it is often written off as "the pink cloud of recovery is passing," or "things are getting tough." When a person has a difficult time staying sober after getting sober, unhealed trauma is usually the culprit, and dissociation is a possible manifestation [6,26].
In an article on the importance of dissociation-informed treatment, several other dissociative behaviors that manifest clinically but that professionals often fail to identify were identified [26]. They included clients struggling to pay attention in group, at 12-step meetings, or during lectures; a client changing tone (e.g., "It's like I'm suddenly speaking to a 5 year old") when something distressing comes up in sessions or in group; and other manifestations of blocking or resistant client behaviors. When a client gets belligerent or angry, this may be a sign of dissociation. In some clients, these types of behaviors could be a part speaking out to protect the system or to get a need met.
The Addiction as Dissociation Model posits that addiction is a manifestation of dissociation. When children grow up in traumatizing, invalidating, or high-stress environments, the natural tendency is to dissociate in order to get needs met and protect themselves. If this happens frequently, the systems bond to this dissociative experience. At a later point in life, when chemicals or other reinforcing behaviors are introduced as possibilities, the chemical impact enhances the potency of an already familiar experience [27].
The term addiction is controversial in the modern era, because many critics feel that term is stigmatizing and not adequately trauma-informed [28]. To address this, the Addiction as Dissociation Model defines addiction as "the relationship created between unresolved trauma and the continued and unchecked progression of dissociative responses" [27]. In presentations where primary addiction treatment has failed to address trauma, dissociative experiences may produce a dissociative disorder or clinically significant symptoms of dissociation. Similarly, if dissociation in trauma has not been treated accordingly, addiction can often manifest [29]. The model contends that addiction develops in relation to trauma and dissociation, because trauma (cause) produces dissociation (effect).
According to the dissociation in trauma concept, there is a "division of an individual's personality, that is, of the dynamic, biopsychosocial system as a whole that determines his or her characteristic mental and behavioral actions" [29]. This distinction can also be seen in Waller, Putnam, and Carlson's taxometric analysis regarding nonpathologic and pathologic (e.g., adaptive and maladaptive) dissociative traits, of which "dissociation in trauma" would be represented by the latter [30]. Dissociation is what creates safety and ultimately pain relief in the moment of need. Trauma deeply impacts a person's psyche—extreme limits are pushed, and extreme reactions become necessary.
Mergler, Driessen, Ludecke, et al. examined the relationship between the PTSD dissociation subtype (PTSD-D) and other clinical presentations [31]. In a sample of 459 participants, the PTSD-D group demonstrated a statistically significantly higher need for treatment due to substance use problems, in addition to higher current use of opioids/analgesics and a higher number of lifetime drug overdoses. They ultimately concluded that PTSD-D is related to "a more severe course of substance-related problems in patients with substance use disorder, indicating that this group also has additional treatment needs" [31]. Such a connection seems like clinical common sense, but it has not been fully explored in the treatment literature.
Table 2 illustrates the tenets of the Addiction as Dissociation Model, a cohesive presentation of what exists in the literature on the inter-relation and interplay of trauma, addiction, and dissociation. While the literature clearly exists to support such a model, the model represents the first cohesive discussion of their interplay. The implications for treatment, which are summarized here and continued into the next section, are various.
ADDICTION AS DISSOCIATION MODEL
| Foundation: The Human Brain | ||||||||
| ||||||||
| The Impact of Trauma-Dissociation-Addiction | ||||||||
| ||||||||
| Treatment and Healing Implications | ||||||||
|
Case conceptualization that respects addiction as dissociation and the related interplays between trauma, dissociation, and addiction acknowledges that addictive behavior is a dissociative response that can elicit its own continued trauma. Moreover, case conceptualization in this model defines and validates the symptoms of addiction accurately and sees the survival behavior as adaptive. This model presents how trauma and dissociation become addictive (i.e., highlights the endogenous neurochemical processes that create the dependent bond in dissociation/addictive processes), how unconscious re-enactments and feedback looping are foundational to recidivism, and provides the justification for comprehensive treatments to directly incorporate a memory reconsolidation phase.
This contention does not suggest that time-honored interventions for treating addiction should be abandoned. However, these interventions should be fortified based on the light of evolving knowledge about trauma and dissociation [6]. Solutions worth highlighting include developing the power of nonjudgmental support communities and the importance of cultivating daily practices that lead to lifestyle change. As such, the community of mutual help fellowships also benefits from an understanding of trauma and dissociation. Peer support services and fellowships like Alcoholics Anonymous, Narcotics Anonymous, Al-Anon, and Adult Children of Alcoholics can provide a safe place to discuss solutions, as long as there is a reasonable degree of trauma-informed ethics in the culture of the meeting.
Cognitive-behavioral therapy (CBT), dialectical behavioral therapy (DBT), and Seeking Safety (SS) are often used in the treatment of addiction. There is an evidence base for their use in successfully treating addiction and other substance use disorders [32]. Yet with the public health crisis of addiction continuing, it is clear that more should be done to address the root of the problem—trauma. Each of these approaches lacks a comprehensive definition of addiction, a conceptualization of where addiction fits into the psychopathology of mental health disorders, and an appreciation for how addiction is experienced as traumatic and how addiction relates to trauma and dissociation. Furthermore, they do not directly incorporate memory resolution or memory reconsolidation as an aspect of treatment.
Treatments like DBT and SS specifically offer PTSD symptom management, and they can be helpful to clients in early stages of treatment for addiction and for individuals with clinically significant dissociative disorders. However, they are not comprehensive therapies if one appreciates addiction as a manifestation of dissociation, as the memory resolution phase of the three-stage consensus model of trauma treatment is absent [33]. Clinicians who mainly practice CBT are advised to incorporate trauma-focused CBT (TF-CBT) to work with both trauma and addiction memory. While processing the narrative or explicit memories is important, having ways to process the physical aspects of trauma is necessary for adaptive resolution and to produce personal transformation [34,35,36,37].
Ultimately, incorporating trauma resolution and memory reconsolidation therapies is essential to bring about healing of the root of the problem, not just the symptoms. Memory reconsolidation is based on the belief that the brain, through a process of memory retrieval and activation, can delete unwanted emotional learning [35]. Progressive counting, emotional coherence, brainspotting, deep brain reorienting, and EMDR therapy provide more direct ways of resolving traumatic/addiction memories [4,35,37,38,39].
A 2024 study suggests that bringing in neurobiolgical research and educating clients about these advances is important in the treatment of dissociative disorders [50]. While this approach can be helpful with clients who respond to hard science evidence of their condition and how to treat it, for others an overemphasis on the hard science can remove the humanity and warmth from clinical treatment. The push toward explaining everything through neuroscience and "fixing" the brain can feel like eugenics or emphasizing only the medical model of disability. In contrast, adopting a more social model of disability would allow clients to accept dissociative minds as they are and teach clinicians how to work with such minds. The approaches proposed in this course largely reflect the social model of disability.
No instant cure or approach to psychotherapy exists for healing trauma, dissociative disorders, or any mental health conditions. In fact, if a professional claims that they have the curative answer for working with trauma and dissociation, proceed with caution. Particularly when working with dissociative systems, the answer to successful treatment rests in finding the approach or series of approaches that works best for that client to achieve their treatment goals. With the intricacies of parts and dissociative systems, it is very likely that a variety of tools and approaches will be necessary, as what works for one part may not resonate with another. This is where being an eclectic or integrated therapist, albeit with a solid understanding of trauma, will serve best.
This section does not endorse any one specific approach for working with or treating dissociation. Some people approach coming to treatment to address clinically significant dissociation as a process of healing maladaptive dissociation while fundamentally working to embrace the aspects of having a dissociative mind that serve them. As with treating any mental health condition using any approach (or approaches) to psychotherapy, it is important to get a sense of what the client's goals and intentions are for engaging in treatment. Never assume that integration is the client's goal or promote any biases that integration is what is required for a person to heal and to live an adaptive life, especially when a client presents with DID or any other dissociative condition that involves parts. Plausible goals that may appear in a treatment plan include:
To manage problematic dissociative symptoms that get in the way of day-to-day life by more regularly using coping skills focused on grounding and mindfulness.
To eliminate acting out behaviors (e.g., drinking, dangerous sex) that are more likely to happen when intense feeling is trying to be avoided.
To promote a greater sense of communication in the internal system that will lead to a reduction of acting out behaviors and dissociating in situations that may be harmful (e.g., driving, at work).
To decrease incidents of acting out inappropriately at work (e.g., shouting at superiors, ignoring colleagues) when feeling triggered. This will require working on two of the protector parts and the origin of their traumatic experience.
To complete a creative project (writing a book) that is currently in progress, learning how to harness the potential of the mind and its dissociative qualities to help in reaching this goal.
After treatment goals have been established in the early stages of rapport building and setting the foundation for treatment, paths for intervention can be more clearly established. Please bear in mind that treatment goals can change and evolve throughout the course of treatment, and this is especially true when working with complex trauma and dissociation. Regardless of the specific interventions a clinician is trained to use, the general recommendation in working with complex trauma and dissociation is that the three stages of treatment established by Janet in 1889 be used as a general guide for treatment planning [33]. The field of trauma study generally refers to this model as the three-stage consensus model of trauma treatment because a consensus does exist on their use as a general structure in treatment planning for anything connected to trauma or dissociation.
The stages and their tasks, as presented in modern language are [40]:
Stage 1: Stabilization, symptom-oriented treatment, and preparation for liquidation of traumatic memories
Stage 2: Identification, exploration, and modification of traumatic memories
Stage 3: Relapse prevention, relief of residual symptomatology, personality reintegration, and rehabilitation
Put simply, clients work to become prepared to handle the symptoms that show up in day-today life while also preparing for a deeper level of work, if they have the intention to go there and heal trauma at its root. Treatment should also include preparing clients to adjust to the changes in their life that happen as a result of unhealed trauma being addressed and transformed. Trauma resolution is only part of treatment—it is not the entire process. Preparation and adjustment to life are also major components of treatment.
These three stages are accepted by the current academic literature reviews that guide formal treatment for dissociation in adults by the ISSTD [41]. Clinicians can access the academic papers cited by ISSTD as best practice treatment guidelines free of charge on the ISSTD website (Resources).
The three-stage consensus model is not without controversy or challenge. In a 2016 review, de Jongh, Resick, Zoellner, et al. contend that the three-stage consensus model has no clear evidence base in treatment of more complex manifestations of trauma [42]. They generally contend that survivors of trauma may not be able to achieve any semblance of stabilization until they first engage in some type of complex trauma work. This debate speaks to one of the greatest clinical puzzles that exists in working with complex trauma—when is a client ready to do the work of trauma resolution? Is taking them to the core of their traumatic memories for healing dangerous and thus focus ought to be on symptom resolution?
Unfortunately, the answer is that there is no easy answer; it must be evaluated on a case-by-case basis. When a dissociative system is involved, clinical judgment should take into account how the entire system works. In EMDR therapy, the term preparation is used instead of stabilization [4]. Perfect stabilization likely will not exist for a survivor of trauma unless they have engaged in some degree of trauma work. Stabilization, like dissociation, really can be seen as a continuum. So, the better question may be: Is the client stable enough or sufficiently prepared to take their healing to a deeper place? Preparation suggests that certain skills will need to be in place to manage life on a day-to-day basis, and widening a person's (or a system's) affective window of tolerance will be required for experiencing emotions and body sensations that are imperative in true trauma resolution work. Evaluating what a client has and what they may need to prepare themselves for meeting their treatment goals is a natural by-product of the Dissociative Profile exercise discussed previously.
Many of the approaches to treatment that exist in the mental health field make wide use of guided imagery or visualization in preparation; these techniques are exclusively cognitive. In working with trauma, especially complex trauma and dissociation, it is vitally important that clinicians have a wide variety of skills that they can offer clients for use during and between sessions. These skills should work with all of the senses and many avenues of human experience [6,43]. Grounding is the very practice of using all available senses and all available channels of human experience to remain in or return to the here and now.
Although clients will not respond favorably to all of these skills and strategies, it is important to offer choice. This choice becomes even more imperative when working with a dissociative system, because one skill may work well for one part when they are active and not another. Certain skills may work better to prevent maladaptive dissociative responses, while others are superior for helping a person (or certain parts) return to the present moment when they experience problematic dissociation.
Skills that may be used for preparation and widening affect windows of tolerance generally fall into the following categories:
Basic awareness/mindfulness and grounding strategies
Breathing strategies
Muscle tensing/releasing exercises
Visualization and multisensory soothing
Containment (i.e., having a visual strategy or actual physical container to "hold" material until the timing is better to address; different than avoiding or pushing something away)
Movement strategies
Identification of other recovery capital (e.g., hobbies, support systems, mutual/self-help/church groups, advocacy activities, community support resources, pets)
Video teachings on skills in each of these categories are available online via the Trauma Made Simple website (Resources).
Some may be further ahead than others in use of such skills in clinical practice, so some clinicians may require a deeper investigation on how to use these skills personally and teach them to others. Regardless of the skills a clinician uses, it is important to trauma-inform the language and leave people plenty of options for modifying. Reading an exercise out of a book, showing a client a video, or even reading one of the skills word-for-word from this course will generally not be sufficient. If a client expresses that something is not working, it could be that they are overwhelmed; a general best practice is to modify the skill either in length or style.
In modern clinical work, many of the skills advocated for helping people to ground or widen their affective window of tolerance can be described as mindfulness practices. Mindfulness is fundamentally about remaining in or returning to the here and now. Consider that dissociation, by its nature, is the antithesis of mindfulness. Forner posits that mindfulness is fundamentally about connection (e.g., to the self, to the present moment, to others), whereas dissociation is ultimately about surviving disconnection [44]. If a person dissociates long enough or becomes bonded to this state (as proposed in the Addiction as Dissociation Model), they can become phobic of mindfulness. As with any other phobia, the answer is not to avoid teaching mindfulness strategies. Rather, clinicians should be cognizant of the idea that when mindfulness strategies are presented to people who dissociate, they are being asked to try something that can feel radical and new. Small steps are required to help people become more comfortable with being present.
Strategies for trauma (and dissociation)-informing existing practices are diverse [1]. First, remember that eyes can stay open. Many clinicians and approaches to therapy or meditation automatically will tell people to "close the eyes," either because they have been trained to do this or because closed eyes help them to focus more effectively. Consider, however, that many people feel claustrophobic or closed in/trapped when their eyes are locked shut. This can promote anxiety. Moreover, closed eyes can be a dissociative response that can create a greater sense of drift or separation from the task at hand. Any exercise can work just as well with the eyes open, and for many clients with dissociation, keeping the eyes open can create a very necessary dual awareness between the room they are in (the present moment) and the memories or experiences that they are visiting in their work.
Second, time in the exercise is variable. Different approaches to clinical work and meditation will often write up skills with suggested lengths of time spent in each strategy, ranging from 3 to 5 minutes up to 25 minutes. Skills on the high end are generally too long for people who dissociate or who are just getting used to working with mindful skills and strategies. Clinicians are always empowered to alter the length of time that they guide a person through an exercise. Even 15 to 30 seconds at first can be an accomplishment for a client, and they can always build on this progress.
Next, let people know how long the exercise, particularly the silence, will last. Many people are triggered or further activated to dissociate when they are not sure how long something will last, especially periods of silence. While a goal may be to help people sit with silence for longer periods of time, be advised that a clinician's voice can be an anchor in many of these exercises. If there will be a period of silence in a meditation or skill, preface the exercise with, "We will now sit silently for the next 30 seconds."
It is also important to clarify any misconceptions or misinformation about what mindfulness, meditation, or yoga means. Many people think that these strategies are automatic relaxation devices, but in reality, their intent is to help people be with what is, even if that present moment experience is something distressing or upsetting. A solid working definition of mindfulness is the practice of returning to the present moment or noticing whatever is in the present moment without judgment.
Be open to variations in practice. Some people associate mindfulness as purely a sitting meditation practice. While this is a popular and potentially very beneficial way to work with mindfulness, any activity can be a vehicle for practicing mindfulness. Many find that walking, engaging in expressive arts practices, using grounding objects (e.g., rocks, crystals, soft blankets), or even activities of daily living (e.g., cleaning, cooking) are better avenues, especially at first. It is all about the intention and where the client is keeping their focus.
Clinicians are encouraged to have their own mindfulness practice. Clinicians who have their own practices realize the importance of modifications and can draw on this experience in teaching clients.
The following grounding skills are written in language that clinicians might use with clients, with the intent to model the principles of trauma-informing exercises. The modifications and variations presented are not exhaustive. Consider what else might be coming up as variations that can be used in presenting these skills. For example, some may not like a word like "grounding," especially if they feel shamed for not being able to ground. Words like "anchoring" and "settling" may be viable modifications. It is important that therapists not expect all-or-nothing adherence to these skills. This can be modeled by saying things like, "Get as grounded as you can," or "Get as comfortable as you can." These modifications are especially important for people living with disabilities or chronic pain.
Basic Grounding and Sensory Scan
Take a look around the space that you are in right now. Start naming the different things you see. Be as specific as possible. For instance, you might say "I see the carpet below my feet. The carpet is blue with some bits of brown in the thread. I see the lamp on the desk. The base of the lamp is brown glass, and the shade is beige." Keep going for as long as you need, until you feel fully present in the space.
If you need, move on to the other senses. What are you hearing (or not hearing) in this moment, in this space? Observe and describe. What are you smelling? What are you tasting? Use your hands and either touch your clothes or make contact with the chair or the table. Observe and describe the touch sensation.
If you are working with an entire system, feel free to ask if all of the parts in a system feel sufficiently grounded and "here." If the answer is no from the presenting adult or the person/parts you work with primarily, invite those part(s) to engage in the same exercise. In using strategies like this, it is recommended you continue to speak to the present adult, using only a middleman (Fraser's term) or speaking directly to the parts in question if needed. In the case of DID in which there are multiple ANPs/presenting adults, the general advice is to work with whoever is present with you.
Mindful Breathing
In working with complex trauma and dissociation, it is important to recognize that breath work may be both a trigger and a resource. So, while deeper breathing strategies may be appropriate eventually, know that starting with basic breath tracking is sufficient.
Pay attention to your normal breathing for 30 seconds to 1 minute. If your mind starts to drift, that is okay, just bring the focus back to your breath.
A whole minute can be a challenge to start. Do not worry; start slowly and be gentle with yourself. If you can eventually work your breath practice up to three minutes, you will find that your breath will be there for you to help you calm yourself when you need it most. It takes practice. If you need the extra help, consider using this classic mantra as a guide, saying it to yourself as you breathe: "As I breathe in, I know I'm breathing in—as I breathe out, I know I'm breathing out." A simple "in-out" also works.
Clench and Release
Start with your hands, if they are available to you. Clench your fists together and notice your edge. Do not hurt yourself. Once you feel you are squeezing as tightly as possible, begin to notice your nails make contact with your skin. Notice the tension. As you do this, bring to mind a person, place, or thing that is causing you distress. Hold the clench as long as you can, at least 10 to 20 seconds.
When you feel like you no longer want to hold on, slowly release the grip of the fists. Feel each finger unlock and spread out. Notice the sensation of letting go and how you experience that in your body. Take a few breaths of your choice as you notice the sensations of release. Repeat as many times as necessary until you are at your desired level of relaxation about the stressor.
Optional: You can also choose to take a deep breath in with the fist clench and hold it as you clench your fists. Release the breath as you release the fists. Only do this if you feel comfortable enough holding the breath.
Variation: Some people are not able to make fists due to body differences or medical conditions (e.g., rheumatoid arthritis), or it may not be considered culturally appropriate. Any muscle group can be tensed and released for this exercise, including the shoulder, the stomach, the forearms, the thighs, or the feet.
Mountain Pose/Standing Meditation
In this practice, we will be working with one of the core poses of Hatha yoga—mountain pose—to explore the idea of standing tall and holding your ground, no matter what distress may exists around you. You do not need a yoga mat for this practice; just use the ground on which you stand.
Come to the front of your mat or to a place on the floor where you feel strong in your stance. Keep your feet together. If this puts too much pressure on your knees or hips, modify by stepping the feet apart slightly (no wider than hip width) while maintaining your balance. Press down into your feet and extend up through the crown of your head. Keep your eyes open and look straight ahead. Bring your hands into prayer position in front of your chest. To engage the energetic potential of the pose even more, become firm through your buttocks and inner thighs and drop the tailbone.
As you inhale, extend your arms straight overhead, interlacing your fingers if possible. If this is not available in your body, keep the arms straight overhead, palms facing each other, shoulder distance apart. Do your best to keep the arms alongside your ears and slightly back.
Use your breath to help you support the holding of the pose. This is not a contest to see how long you can hold the pose. Rather, when you first notice that you want to come out of it, challenge yourself to use your breath and other tools you now have to help you sustain the pose. Remember that the purpose of an edge is never to strive or push through pain. Always honor your body and back off when you need to.
Reset and try again if possible. The lesson we can learn in doing this type of work is of one's ability to practice adaptability by taking a break, resetting the breath, and then trying again.
Variations: You are free to use the wall or a chair for support. You can stand up and come up against the wall for that extra support. If using a chair, you can stand behind the chair and hold on with one hand, and do your best to use the other hand and arm for the overhead component of the pose. If you are not able to stand, feel free to modify the spirit of this pose as needed from a sitting position. Press down wherever you can in your lower body, and bring the upper body into position as you are able.
After engaging in this practice with a system, you can also inquire to see if all of the parts in the system responded well to this pose or if any struggled. If so, explore the source of that struggle and ask, perhaps, if there is a resource you can align for working with that part when they are standing up. For instance, some parts may not like the prayer hands, especially if they experienced spiritual or religious trauma. It may feel better to keep them at the side. Another part may like to envision a bright and healing light while they are standing tall. The options are limitless if you are willing to get feedback from clients as you go and explore options and variations.
The therapeutic connection clients experience with providers can be more important than any technique, strategy, or modality used [48]. While the therapeutic alliance is an important feature of any therapy and in working with any population, issues around therapeutic alliance should be attended to in a special way when working with the spectrum of dissociation. A clinician's willingness to admit that dissociation is real and that a system is not manifestation of one's imagination is a great start in building rapport. As always, clinicians should be mindful not put their own agendas or projections on to a client, even in taking a more normalizing approach to dissociation.
Navigating the particulars of the therapeutic relationship can be sensitive. For instance, some parts in the system may not like a therapist or not be a fan of therapy in general. Clinicians are encouraged to roll with this resistance and take great care not to take any insults personally. Rather, consider what that particular part may find distressing and work to explore a solution. In doing clinical work, "hearing out" a part is generally more beneficial than trying to fight it.
Another potential problem area is a tendency for therapists to over-attach to younger or more vulnerable parts. There can be a desire for younger parts to turn the therapist into a parent figure, and this can cause some enmeshment and blurring of boundaries. While it is certainly possible to validate a client's or system's desire to see one as a parent, it is important to be clear that you are not their parent. This can feel cruel, but many of clients suffer because good boundaries were not modeled for them in early childhood. So, clinicians are in a position to validate their feelings and also challenge them into action, all while modeling and offering instruction about healthy boundaries. If this type of relationship is developing, ask the client/parts what qualities are being exhibited that they may have needed in a parent. These qualities can be used when evaluating what resources need to be built or worked on for younger parts in the system.
The following meditation and resourcing strategy may prove helpful for you and your clients in this process. As always, feel free to adjust and modify if needed.
Protector figure resources may include people (real or imagined), spiritual entities, or even fictional characters to whom the client has a special attachment can be used. Another adjective may feel better than protector, including guardian, nurturer, advocate, or healer. Precautions should be taken, especially if using people who are still alive or may qualify as a mixed resource (i.e., they possess adaptive and maladaptive qualities). The exercise is written to go slowly and be adapted to the specific person and their system. Guided visualization may be used for this, as can expressive arts strategies or any strategy that works in the system of therapy in which you are trained.
Single Figure
Start by working with just a single figure. Try to stay away from real people at first. Think of the spiritual realm, fictional characters, or an entity that you create using the power of your imagination. You can choose if you want to use an adjective to describe this figure, like protector figure or sacred figure. Maybe a word like cheerleader or nurturer works better for the intention that you are setting today.
Breathe and notice. Does this figure you chose have a name? What do they look like? What are they wearing? If they have a face, what do you observe on their face? Notice what this figure is doing, or where they are in relation to you in this meditation. Maybe they are literally sitting beside you. Maybe you imagine them putting their hands on your shoulders in support. Maybe you are engaging in an activity with them. Notice whatever you notice.
Then notice the qualities that the figure you have selected brings to you. How do they make you feel about yourself? What are you noticing in your thoughts, your feelings, and your experiences when you are in their presence? Is there a certain bodily sensation that you may be noticing, the deeper you engage or notice this figure of yours? Keep breathing.
To go further, recall a challenging situation that may be coming up in your life the next few days or weeks. What would it look like, or what would it feel like, if you imagined bringing this protector figure with you?
Circle of Figures
After establishing this practice with a single figure, you can go further by imagining a circle of support—people who are spiritual entities or fictional entities from whom we have drawn great strength. Historical figures and inspirational persons who have passed away can also be part of your circle. You can also bring people who are in your life right now into your circle, as long as they feel like a primarily positive resource. Imagine who is surrounding you. Who constitutes your circle of support?
Maybe there are only two figures, or maybe there are several. Maybe each figure takes on a different quality. Perhaps you have a protector figure, a sacred figure, a cheerleading figure, and a nurturing figure.
Notice what you most need in your life today, or in your life in general. Who are some figures that you can ally with to present you with those qualities? Take a moment here to see what comes into focus.
Think of a situation coming up in your life in the next few days or the next week that may present a particular challenge. When that has come into your awareness, notice it. Notice what that would feel like, and what that would look like. Next, notice your response as you imagine your circle of support taking you into this challenge. Keep breathing.
When a client (and their system) experiences an adequate sense of preparation to move forward, the system can begin heal using any number of therapeutic strategies. Before continuing, it can be helpful for clinicians to contemplate what they consider to be their primary therapeutic orientation or orientations. In many cases, professionals can use what they have already learned to help people reach their established goals by assisting them to process or modify how traumatic memories are stored in the brain.
For instance, EMDR therapy is appropriate for working with dissociation if the clinician offering the therapy is well-informed in how dissociation can play out in an individual or their system and plans their targets and strategies with respect to how the system may work. Regardless of the approach used, if a block or a resistance shows up in the work, this is likely another part trying to have their voice heard, either to meet a need or to protect the system. Clinicians should be prepared with protocols in place to address these blocks. Seeking consultation from someone who practices the specific therapeutic approach and is well-skilled in working with dissociation and dissociative parts may be warranted to help build skills and confidence.
Expressive arts therapy, which refers to using any and all available creative forms (e.g. dance/movement, writing, art, drama, music) in combination, or any of the creative arts therapies as singular strategies can be a solid adjunct to any strategy available for processing or transforming trauma's impact in the brain. In many cases, parts in a system are young in terms of chronological age or exist in a state that cannot easily be accessed by words or language. Drawing or dancing may be a way to access the material that needs to be processed. Expressive arts strategies can be used in concert other approaches to trauma-focused therapy if the clinician has a sense of adventure and a willingness to personally try these strategies [45].
Table 3 provides a list of therapeutic approaches and online resources to access additional information. All of these approaches have some form of evidence base for working with the processing of traumatic memories and a protocol for how to best handle dissociation. Some of the modalities require more training than others, and clinicians who feel unprepared to work with processing traumatic memories in a holistic way may consider pursuing additional training in one of these modalities.
RESOURCES FOR THERAPEUTIC APPROACHES TO PROCESSING TRAUMA AND RELATED DISSOCIATIONa
| Approach | Recommended Resource |
|---|---|
| Accelerated experiential dynamic psychotherapy (AEDP) | https://aedpinstitute.org |
| Acceptance and commitment therapy (ACT) | https://contextualscience.org/act |
| Art therapy | https://arttherapy.org |
| Body-centered psychotherapy and somatic psychology | https://usabp.org |
| Brainspotting | https://brainspotting.com |
| Cognitive processing therapy | https://cptforptsd.com |
| Coherence therapy | http://www.coherencetherapy.org |
| Dance/movement therapy | https://www.adta.org |
| Developmental needs meeting strategy | https://www.dnmsinstitute.com |
| Dialectical behavior therapy (DBT) | https://behavioraltech.org |
| Drama therapy | https://www.nadta.org |
| Emotional freedom techniques (EFT) | https://www.emofree.com |
| Energy psychology | https://www.energypsych.org |
| Equine-assisted therapy | https://www.eagala.org |
| Exposure therapy | https://www.apa.org/ptsd-guideline/patients-and-families/exposure-therapy |
| Expressive arts therapy | https://www.ieata.org |
| Eye movement desensitization and reprocessing (EMDR) | https://www.emdria.org |
| Focusing | https://focusing.org |
| Gestalt therapy | https://aagt.org |
| Hakomi mindful somatic psychotherapy | https://hakomiinstitute.com |
| Hypnosis and hypnotherapy | https://www.asch.net |
| Internal family systems therapy (IFS) | https://ifs-institute.com |
| Music therapy | https://www.musictherapy.org |
| Narrative therapy | https://narrativetherapycentre.com |
| Neuro emotional technique (NET) | https://www.netmindbody.com |
| Neurofeedback | https://isnr.org |
| Neuro-linguistic programming (NLP) | https://www.neurolinguisticprogramming.com |
| Play therapy | https://www.a4pt.org |
| Progressive counting (PC) | https://www.childtrauma.com/treatment/pc |
| Psychoanalysis | https://apsa.org |
| Psychomotor therapeutic system | https://pbsp.com |
| The Sanctuary Model | https://www.nctsn.org/interventions/sanctuary-model |
| Sensorimotor psychotherapy | https://sensorimotorpsychotherapy.org |
| Somatic experiencing | https://www.somaticexperiencing.com |
| Trauma-focused cognitive-behavioral therapy (TF-CBT) | https://tfcbt.org |
| Trauma incident reduction (TIR) | https://www.tira.org |
| Trauma Resiliency and Community Resiliency Models | https://www.traumaresourceinstitute.com |
| Yoga therapy | https://www.iayt.org |
| aThis list is not intended to be exhaustive, and other modalities and resources may be appropriate. | |
In the treatment recommendations provided by the ISSTD, no one specific treatment modality is endorsed for doing stage 2 work. What is important is that clinician and client has a solid therapeutic alliance established with good boundaries, and that they understand how to work with abreaction (when material shifts from the sub-conscious into consciousness, with some type of affective release typically accompanying it). Working integration will help a client and their system be able to put the past in its proper place and allow all facets of experience to be attended to. With a system involved, this may not be an easy task; it should be handled with care and attention to the system. The client-driven An Infinite Mind organization also does not endorse any one modality in the treatment of DID. Instead, they emphasize the importance of finding a therapist who believes in dissociation and who is willing to work with it, while also giving a client/survivor of trauma options for care.
An estimated 10% of the adult population is estimated to have a dissociative disorder; the majority are living typical lives and making valuable contributions to society [46]. Prevalence rates are higher in certain populations (e.g., psychiatric inpatients). For the sake of these patients, biases or preconceived notions about the impossibility of healing and optimal functioning in people who clinically dissociate should be put aside. These clients deserve the best available care to address their traumatic memories and improve their quality of life. The third stage of the three-stage consensus model of trauma treatment is generally called reintegration, and its primary objective is to assist people to make adjustments based on healing gains in therapy, ultimately living more adaptive, fulfilling lives.
How a clinician approaches stage three work with individuals who have DID or otherwise dissociate is not unlike how one might approach this stage with any other client impacted by trauma. One should be mindful that this work should be geared toward helping the system function as optimally and as peacefully as possible. Much of the work that took place in the preparation stages has a natural carry over to the reintegration phase. A helpful strategy can be to have the client and their system do the Dissociative Profile exercise at several intervals to see if any adjustments may need made. Completing one after an initial round of some work in stage two and also re-evaluating as termination nears is recommended.
Another question that arises is whether or not people with DID especially will require continued treatment or care for the rest of their lives or if termination is possible. In many ways, DID and other dissociative disorders are no different than any other major mental health disorders when contemplating termination. Some people will need long-term care as they adjust to living a more adaptive life aligned with their goals and intentions; others will reach a place where regular therapeutic care is no longer necessary. Like many issues in mental health, a case-by-case approach should be taken. Pharmacotherapy is outside of the scope of this course, but clients with dissociative symptoms or DID might be prescribed medications under the care of a psychiatrist or addiction medicine specialist. If this is the case, as a therapist, it is important to have regular contact with these providers to assure continuity in care and interprofessional collaboration.
Parts journaling is an exercise based on Gestalt principles and other time-honored strategies in the field of psychotherapy, with an expressive arts twist. Like any exercise in this course, clinicians are encouraged to personally complete it first, and then consider sharing it with clients.
For this exercise, refer to any artwork or mapping that you created for your personal parts exploration. The purpose of that exercise was to provide a sense of how your system works. In this exercise, the objective is to further explore how the system interacts. Where might some areas of communication need to take place? As you examine the artwork you created, is there one part, segment, or facet that is most jumping out or resonating for you right now? If so, notice it and consider this question: If that part had a message for me right now, what would it be? It is permissible to use the presenting adult/core ego state/ANP, if that is what you are noticing the most. Take about three to five minutes to free write.
After this initial writing, look at the art work once more and notice if there is a second part, segment, or facet that is also calling your attention. Follow the same steps—notice and ask if that part had a message for me right now, what would it be? Again, take about three to five minutes to free write.
Now you are encouraged to write a dialogue between the two parts, segments, or facets. Take at least three to five minutes to let this unfold, although you can take longer if you wish. Consider the following example:
Adult Jamie (AJ): I'm working on my presentation for the EMDR conference.
9: Oh, boy. You still go to that?
AJ: Of course. It's gotten better for me. For all of us, I think.
9: What are you teaching on this year?
AJ: Dissociation—about how our mind works.
9: Oh, brother. Do you think we can handle it without chewing their heads off?
AJ: I'm hoping we can. Can I get your input first?
9: You really sure you want to hear from me on this one?
AJ: Yes, I do.
You can name your parts, segments, or facets whatever you wish. (What appears in the example reflects how I specifically engage in parts journaling.) As with every exercise outlined in this course, it is important not to censor yourself—let whatever unfolds happen, being open to any surprises or insights. If at any point you feel too overwhelmed, you have permission to stop and go back to one of your grounding or other coping skills. You can choose to resume the exercise later or leave it. What did you notice about yourself, the process, and your own internal world as a result of this exercise?
Parts journaling can be particularly useful for clients working with material in the system between sessions. There are also many implications for this sense of dialogue and communication can be used to help one's systems and internal world live more adaptively. When using this exercise with a client, it is strongly advised that it is personally completed first and that the client do the exercise in the presence of the clinician the first time it is attempted, so they have assistance working through any distress or overwhelm they might experience. As always, it is vital to use good clinical judgment about assigning this as therapeutic homework between sessions. Clients may do very well with this on their own after they understand its intention—to give voice to parts of the system that may need to speak and to engender a higher degree of communication. Although one should begin writing between only two parts to start, the voices of other parts can be brought in, especially if they have a mediating influence or hold an important part of the solution.
Other expressive arts possibilities (e.g., art, movement) can be integrated into parts journaling work. For some people, after they engage in the parts journaling, it can feel nourishing and transformative to make art (even if it is scribbles or doodles) on top of the words. With any kind of journaling, it is important to let clients know that they do not need to keep the writing or leave their words exposed; ripping pages or burning them safely are always options. Making art on top of the words is another option that speaks to this idea of making something beautiful out of something potential painful. If working with movement, consider this variation: If Part A's message could be expressed in a movement or a gesture, what would that be? If Part B's message could be expressive in a movement or a gesture, what would that be? Then spend a few minutes going back-and-forth between the movements/gestures and see what naturally unfolds.
Dissociation is a natural and normal part of the human experience. An inherent mechanism of the primitive brain, dissociation allows for needs to be met and for protection when one feels especially vulnerable. Understanding the intricacies of dissociation is imperative if a therapist or other helping professional wishes to be as trauma-focused as possible. Trauma and dissociation go hand-in-hand, and this interplay can manifest in ways that are clinically puzzling. However, a main theme of this course is that understanding one's own relationship with dissociation and internal world of parts is an important educational step to working with dissociation effectively. There is a time-honored piece of wisdom—we cannot take our clients farther than we have personally gone ourselves. A clinician's willingness to do this work, even if it starts with the three experiential exercises that appeared in this course, will go a long way. Moreover, clinical consultation, or consultation with a trauma survivor who has DID or another dissociative disorder, can be valuable. As with any pursuit in the helping professions, it is important not to let the science over-ride the art.
| An Infinite Mind |
| https://www.aninfinitemind.com |
| DID Research |
| https://www.did-research.org |
| Dissociative Disorders Interview Schedule |
| https://www.rossinst.com/ddis |
| Dissociative Experiences Scale-II |
| http://traumadissociation.com/des |
| How to Use Fraser's Dissociative Table Technique to Access and Work with Emotional Parts of the Personality by Kathleen Martin |
| https://connect.springerpub.com/content/sgremdr/6/4/179 |
| Harvey Weinstein's "False Memory" Defense and Its Shocking Origin Story by Anna Holtzman |
| https://medium.com/fourth-wave/harvey-weinsteins-false-memory-defense-and-its-shocking-origin-story-2b0e4b98d526 |
| Institute for Creative Mindfulness |
| Dissociation and Addiction Resources |
| https://www.instituteforcreativemindfulness.com/dissociation--addiction-resources |
| International Society for the Study of Trauma and Dissociation |
| https://www.isst-d.org |
| Multidimensional Interview of Dissociation (MID) |
| http://www.mid-assessment.com |
| Dissociative Disorders Interview Schedule (DSM-5 Version) |
| https://www.rossinst.com/Downloads/DDIS-DSM-5.pdf |
| Trauma and Dissociative Disorders Explained |
| http://traumadissociation.com |
| Redefine Therapy |
| https://redefinetherapy.com |
| Guidelines for Treating Dissociative Identity Disorder in Adults |
| https://www.isst-d.org/resources/adult-treatment-guidelines |
| Guidelines for the Evaluation and Treatment of Dissociative Symptoms in Children and Adolescents |
| https://www.isst-d.org/resources/child-adolescent-treatment-guidelines |
| The Plural Association |
| https://powertotheplurals.com |
| Multiplied by One |
| https://multipliedbyone.org |
| Petals of a Rose (a film) |
| https://www.dylancrumpler.com/watch-petals-of-a-rose |
| System Speak |
| https://systemspeakcommunity.com |
| A Couple of Multiples Podcast |
| https://www.acoupleofmultiples.com |
| Beauty After Bruises |
| https://www.beautyafterbruises.org |
1. Marich J, Dansiger S. EMDR Therapy and Mindfulness for Trauma-Focused Care. New York, NY: Springer Publishing Company; 2018.
3. Howell E. Trauma and Dissociation-Informed Psychotherapy: Relational Healing and Therapeutic Connection. New York, NY: W.W. Norton & Co.; 2020.
4. Shapiro F. Eye Movement Desensitization and Reprocessing: Basic Principles, Protocols, and Procedures. 3rd ed. New York, NY: The Guilford Press; 2018.
5. MacLean PD. The Triune Brain in Evolution: Role in Paleocerebral Functions. New York, NY: Plenum Press; 1990.
6. Marich J. Trauma and the 12 Steps: An Inclusive Guide to Recovery. Berkeley, CA: North Atlantic Books; 2020.
7. Gingrich HD. Restoring the Shattered Self: A Christian Counselor's Guide to Complex Trauma. Downers Grove, IL: InnerVarsity Press; 2020.
8. Schauer M, Elbert T. Dissociation following traumatic distress: etiology and treatment. Journal of Psychology. 2010;218(2):109-127.
9. Krause-Utz A, Frost R, Winter D, Elzinga B. Dissociation and alterations in brain function and structure: implications for borderline personality disorder. Current Psychiatry Reports. 2017;19(1):6.
10. Cacioppo S. What happens in your brain during mental dissociation? A quest towards neural markers of a unified sense of self.Current Behavioral Neuroscience Reports. 2016;3:1-9.
11. Marich J. Interview with Jaime Pollack. Available at https://www.youtube.com/watch?v=yntseh3XCJs&t=2s. Last accessed May 23, 2024.
12. Miller P. EMDR Therapy for Schizophrenia and Other Psychoses. New York, NY: Springer Publishing Company; 2016.
13. Courtois C, Ford J. Treating Complex Traumatic Stress Disorders: An Evidence-Based Guide. New York, NY: The Guilford Press; 2009.
14. Marich J. Trauma Made Simple: Competencies in Assessment, Treatment, and Working with Survivors. Eau Claire, WI: PESI Publishing and Media; 2014.
15. Okano K. Dissociative disorder: the concept and its history. Seishin Shinkelgaku Zashhi. 2011;113(9):888-896.
16. Frances A. Saving Normal: An Insider's Revolt Against Out-of-Control Psychiatric Diagnosis, DSM-5, Big Pharma, and the Medicalization of Ordinary. New York, NY: William Morrow & Co.; 2014.
17. van der Hart O, Moskowitz A. Multiple states of consciousness, complexes, personalities, or parts of the personality? An historical perspective and contemporary proposal on trauma-related dissociation. Rivista Sperimentale di Freniatria. 2018;1(2018):51-71.
18. Waseem M, Aslam M. Dissociative Identity Disorder. Available at https://emedicine.medscape.com/article/916186-overview. Last accessed May 23, 2024.
19. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Text revision. Washington, DC: 2022.
20. An Infinite Mind. What is a Dissociative Disorder? Available at https://www.aninfinitemind.org/dissociation-information. Last accessed May 23, 2024.
21. Marich J. A Personal (and Professional) Take on Dissociative Disorders. Available at https://themighty.com/2018/12/dissociative-disorders-professional-personal-perspective. Last accessed May 23, 2024.
22. Carlson EB, Putnam FW. An update on the Dissociative Experience Scale. Dissociation. 1993;6(1):16-27.
23. Fraser G. The dissociative table technique: a strategy for working with ego states in dissociative disorders and ego state therapy. Dissociation. 1991;4(4):205-213.
24. Fraser G. Fraser's Dissociative Table Technique revisited, revised: a strategy for working with ego states in dissociative disorders and ego state therapy. Journal of Trauma and Dissociation. 2003;4(4):5-28.
25. van der Hart O, Nijenhuis E, Steele K. The Haunted self: Structural Dissociation and the Treatment of Chronic Traumatization. New York, NY: W.W. Norton & Co.; 2006.
26. Marich J, O'Brien A. Demystifying Dissociation: A Clinician's Guide. Available at https://www.hmpgloballearningnetwork.com/site/addiction/article/mindfulness-and-psychotherapies/demystifying-dissociation-clinicians-guide. Last accessed May 23, 2024.
27. O'Brien A, Marich J. Addiction as Dissociation Model. Available at https://www.instituteforcreativemindfulness.com/icm-blog-redefine-therapy/addiction-as-dissociation-model-by-adam-obrien-dr-jamie-marich. Last accessed May 23, 2024.
28. Ashford RD, Brown A, Brown T, et al. Defining and operationalizing the phenomena of recovery: a working definition from the Recovery Science Research Collaborative. Addiction Research & Theory. 2019;27(3):179-188.
29. Nijenhuis ERS, van der Hart O. Dissociation in trauma: a new definition and comparison with previous formulations. Journal of Trauma and Dissociation. 2011;12(4): 416-445.
30. Waller N, Putnam FW, Carlson EB. Types of dissociation and dissociative types: a taxometric analysis of dissociative experience. Psychological Methods. 1996;1(3):300-321.
31. Mergler M, Driessen M, Ludecke C, et al. Relationship between a dissociative subtype of PTSD and clinical characteristics in patients with substance use disorders. Journal of Psychoactive Drugs. 2017;49(3):225-232.
32. Center for Substance Abuse Treatment. Substance Abuse Treatment for Persons with Co-Occurring Disorders. TIP Series 42. Washington, DC: U.S. Government Printing Office; 2013.
33. Cloitre M, Coutois CA, Ford JD, et al. The ISTSS Expert Consensus Treatment Guidelines for Complex PTSD in Adults. Available at https://istss.org/ISTSS_Main/media/Documents/ComplexPTSD.pdf. Last accessed May 23, 2024.
34. Scaer R. The Trauma Spectrum: Hidden Wounds and Human Resiliency. New York, NY: W. W. Norton & Company; 2005.
35. Ecker B, Ticic R, Hulley L. Unlocking the Emotional Brain: Eliminating Symptoms at Their Roots Using Memory Reconsolidation. New York, NY: Routledge; 2012.
36. van der Kolk B. The Body Keeps the Score: Brain, Mind and Body in the Healing of Trauma. New York, NY: Penguin Books; 2014.
38. Lasser KA, Greenwald R. Progressive counting facilitates memory reconsolidation. The Neuropsychotherapist. 2015;10:30-37.
39. Grand D. Brainspotting: The Revolutionary New Therapy for Rapid and Effective Change. Boulder, CO: Sounds True; 2013.
40. van der Hart O, Brown P, van der Kolk B. Pierre Janet's treatment of post-traumatic stress. Journal of Traumatic Stress. 1989;2(4):1-11.
41. Chu JA, Dell PF, van der Hart O, et al. Guidelines for treating dissociative identity disorder in adults, third revision. Journal of Trauma & Dissociation. 2011;12(2):115-187.
42. de Jongh A, Resick P, Zoellner L, et al. Critical analysis of the current treatment guidelines for complex PTSD in adults. Depression and Anxiety. 2016;33:359-369.
43. Postlewaite M. Grounding: coming into the here and now by using our bodily sensations. In: Fehr SS (ed). 101 Interventions in Group Therapy. 2nd ed. New York, NY: Routledge; 2016: 78-80.
44. Forner C. What mindfulness can learn from dissociation and dissociation can learn from mindfulness. Journal of Trauma & Dissociation. 2019;20(1):1-15.
45. Marich J. Process Not Perfection: Expressive Arts Solutions for Trauma Recovery. Warren, OH: Creative Mindfulness Media; 2019.
46. Sar V. Epidemiology of dissociative disorders: an overview. Epidemiol Res Intern. 2011;2011:404538.
47. Cesario J, Johnson D, Eisthen H. Your brain is not an onion with a tiny reptile inside. Current Directions in Psychological Science. 2020;29(3):255-260.
48. Marich J. Dissociation Made Simple: A Stigma-Free Guide to Embracing Your Dissociative Mind and Navigating Life. Berkeley, CA: North Atlantic Books; 2023.
49. Power to the Plurals. Why the Theory of Structural Dissociation is Ableist: A Strong Opinionated Article. Available at https://powertotheplurals.com/why-the-theory-of-structural-dissociation-is-ableist. Last accessed June 12, 2024.
1. Chu JA, Dell PF, Van der Hart O, et al. Guidelines for treating dissociative identity disorder in adults, third revision. Journal of Trauma & Dissociation. 2011;12(2):115-187. Available at https://www.isst-d.org/wp-content/uploads/2019/02/GUIDELINES_REVISED2011.pdf. Last accessed May 30, 2024.
Mention of commercial products does not indicate endorsement.