Although physicians are responsible for directing and prescribing care for patients with acute coronary syndrome (ACS), nurses play a vital role in promoting adherence to practice guidelines. This course begins with an overview of the scope of the problem and its economic impact on health care in the United States. An overview of the pathophysiology of ACS and its underlying disease process, coronary artery disease (CAD), will be presented to provide background for understanding specific practice recommendations. Clinical signs and symptoms, diagnosis, and management of UA, NSTEMI, and STEMI will be discussed and illustrated through the use of simulated clinical scenarios. Emergent assessment, diagnostic measures, and initial treatment options will be explored, followed by a discussion of follow-up care and preparation for discharge. Key points of secondary prevention, including smoking cessation, treatment of dyslipidemia, and modification of other risk factors will be outlined.
- INTRODUCTION
- DEFINITION OF TERMS
- SCOPE OF THE PROBLEM
- PATHOPHYSIOLOGY OF ACS
- RISK FACTORS FOR CHD
- TRIAGE
- DIAGNOSIS
- TREATMENT OF UA/NSTEMI
- MANAGEMENT OF COCAINE-INDUCED ACS
- TREATMENT OF STEMI
- DISCHARGE PLANNING AND SECONDARY PREVENTION
- ADHERENCE TO EVIDENCE-BASED GUIDELINES
- INTERPROFESSIONAL PRACTICE AND COLLABORATION
- SIMULATED CASE STUDIES
- CONCLUSION
- RESOURCES
- Works Cited
- Evidence-Based Practice Recommendations Citations
This course is designed for nurses practicing in primary care, inpatient, outpatient, and home care settings to enhance their knowledge of the evidence-based guidelines related to the assessment, management, and secondary prevention of acute coronary syndrome.
The pace at which guidelines for acute coronary syndrome are updated make it challenging for clinicians to remain current with the recommendations that lead to improved outcomes for this substantial patient population. The purpose of this course is to reduce the widening gap between care according to guidelines and actual care delivered by providing nurses with knowledge necessary to implement the most appropriate approach to diagnosis and treatment.
Upon completion of this course, you should be able to:
- Explain the pathophysiology of ACS, including the role of plaque formation and rupture.
- Discuss risk factors and key aspects of screening for atherosclerotic plaque and coronary heart disease (CHD).
- Describe components of triaging patients with suspected ACS.
- Identify key elements that should be included in the history and physical examination of patients with suspected ACS, including the role of stress tests.
- List key elements to include in chest pain assessment for a patient with possible ACS.
- Outline the role of 12-lead ECG and cardiac biomarkers in the diagnosis and risk stratification of ACS.
- Review key recommendations for the medical and nursing management of patients with UA/NSTEMI, including initial treatment, early inpatient care, and recommended pharmacotherapy.
- Describe ischemia-guided and invasive strategies related to the management of patients with UA/NSTEMI.
- Discuss key components of medical and nursing management of patients with variant angina and cocaine-induced ACS.
- Explain the role of PCI in the management of STEMI, including the issues of timing, stent selection, supporting pharmacologic therapy, risks, and possible complications.
- Outline the use of fibrinolytic therapy as a reperfusion therapy in the management of STEMI, including the issues of indications, contraindications, supporting pharmacologic therapy, and risks.
- List key measures used to prevent reocclusion in coronary circulation following reperfusion with PCI or fibrinolytic therapy.
- Discuss the role of smoking cessation in reducing the risk of recurrent ACS and tools for helping patients quit smoking.
- Describe other measures patients may take to reduce risk of recurrent ACS and ongoing CHD from hypertension, dyslipidemia, and other modifiable risk factors.
- Explain factors that impact a patient's adherence to prescribed therapy and measures to reduce risk of recurrent coronary disease.
Karen Majorowicz, RN, is currently employed in the Cardiac Intermediate Care Unit at Shands Healthcare at the University of Florida, Gainesville. She received her Master's in Medical-Surgical Nursing in 1978 from the University of Maryland. Karen has created numerous instructional manuals on Medicare and has conducted educational programs on cardiovascular assessment.
Lori L. Alexander, MTPW, ELS, MWC, is President of Editorial Rx, Inc., which provides medical writing and editing services on a wide variety of clinical topics and in a range of media. A medical writer and editor for more than 30 years, Ms. Alexander has written for both professional and lay audiences, with a focus on continuing education materials, medical meeting coverage, and educational resources for patients. She is the Editor Emeritus of the American Medical Writers Association (AMWA) Journal, the peer-review journal representing the largest association of medical communicators in the United States. Ms. Alexander earned a Master’s degree in technical and professional writing, with a concentration in medical writing, at Northeastern University, Boston. She has also earned certification as a life sciences editor and as a medical writer.
Contributing faculty, Karen Majorowicz, RN, has disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
Contributing faculty, Lori L. Alexander, MTPW, ELS, MWC, has disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
Jane C. Norman, RN, MSN, CNE, PhD
The division planner has disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
Sarah Campbell
The Director of Development and Academic Affairs has disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
The purpose of NetCE is to provide challenging curricula to assist healthcare professionals to raise their levels of expertise while fulfilling their continuing education requirements, thereby improving the quality of healthcare.
Our contributing faculty members have taken care to ensure that the information and recommendations are accurate and compatible with the standards generally accepted at the time of publication. The publisher disclaims any liability, loss or damage incurred as a consequence, directly or indirectly, of the use and application of any of the contents. Participants are cautioned about the potential risk of using limited knowledge when integrating new techniques into practice.
It is the policy of NetCE not to accept commercial support. Furthermore, commercial interests are prohibited from distributing or providing access to this activity to learners.
Supported browsers for Windows include Microsoft Internet Explorer 9.0 and up, Mozilla Firefox 3.0 and up, Opera 9.0 and up, and Google Chrome. Supported browsers for Macintosh include Safari, Mozilla Firefox 3.0 and up, Opera 9.0 and up, and Google Chrome. Other operating systems and browsers that include complete implementations of ECMAScript edition 3 and CSS 2.0 may work, but are not supported. Supported browsers must utilize the TLS encryption protocol v1.1 or v1.2 in order to connect to pages that require a secured HTTPS connection. TLS v1.0 is not supported.
The role of implicit biases on healthcare outcomes has become a concern, as there is some evidence that implicit biases contribute to health disparities, professionals' attitudes toward and interactions with patients, quality of care, diagnoses, and treatment decisions. This may produce differences in help-seeking, diagnoses, and ultimately treatments and interventions. Implicit biases may also unwittingly produce professional behaviors, attitudes, and interactions that reduce patients' trust and comfort with their provider, leading to earlier termination of visits and/or reduced adherence and follow-up. Disadvantaged groups are marginalized in the healthcare system and vulnerable on multiple levels; health professionals' implicit biases can further exacerbate these existing disadvantages.
Interventions or strategies designed to reduce implicit bias may be categorized as change-based or control-based. Change-based interventions focus on reducing or changing cognitive associations underlying implicit biases. These interventions might include challenging stereotypes. Conversely, control-based interventions involve reducing the effects of the implicit bias on the individual's behaviors. These strategies include increasing awareness of biased thoughts and responses. The two types of interventions are not mutually exclusive and may be used synergistically.
#30993: Acute Coronary Syndrome: An Overview for Nurses
Acute coronary syndrome (ACS) is an umbrella term for any condition characterized by symptoms of acute myocardial ischemia caused by an abrupt reduction in blood flow to the heart muscle. Three related but distinct clinical entities fall under the category of ACS: unstable angina (UA), non-ST-segment elevation myocardial infarction (NSTEMI), and ST-segment elevation myocardial infarction (STEMI) [1].
Advances in the understanding of the pathophysiology of ACS have led to the identification of UA/NSTEMI and STEMI as distinct clinical entities, with differences in etiology, clinical features, treatment, and outcomes [2,3,4]. In addition, the development and evaluation of pharmacologic therapies and reperfusion procedures in a multitude of large-scale trials have resulted in a redefinition of the diagnosis and treatment of acute myocardial infarction (MI). The results of these trials have formed the evidence base for clinical practice guidelines developed by the American College of Cardiology (ACC) and the American Heart Association (AHA), in conjunction with other specialty organizations [2,3,5,6]. Despite the widespread dissemination of these guidelines and documentation of better outcomes and decreased risk for subsequent events with guideline-driven treatment, adherence to many aspects of guideline-directed treatment could be improved [7,8,9,10]. Variations in practice have resulted in reports of disparities in assessment, treatment, and outcomes across subgroups according to age, gender, race/ethnicity, risk level, type of MI, and practice setting [9,11,12,13,14,15,16,17,18]. Highlighting the different needs of different populations of patients and the disparities in care, as well as emphasizing the appropriate use of treatment guidelines, can help to reduce the gap between evidence-based care and actual care delivered.
Although physicians are responsible for directing and prescribing care, nurses play a vital role in promoting adherence to practice guidelines. Several quality improvement initiatives developed to help improve adherence to established ACS guidelines have met with success [19]. These initiatives include Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes with Early Implementation? (CRUSADE), Guidelines Applied in Practice, and Get With the Guidelines (GWTG) [19,20,21]. Studies have indicated that physicians and nurses as well as healthcare systems can improve the quality of care they provide to their patients by implementing a combination of best practices, including participation in continuing education and in quality management efforts [20].
The purpose of this course is to provide nurses practicing in primary care, inpatient, outpatient, or home care settings, as well as those who practice in emergency rooms or in cardiovascular specialty settings, with current information about the evidence-based guidelines for the management of patients with ACS. The program begins with an overview of the scope of the problem and its economic impact on health care in the United States. An overview of the pathophysiology of ACS and its underlying disease process, coronary heart disease (CHD), will be presented to provide background for understanding specific practice recommendations. Clinical signs and symptoms, diagnosis, and management of UA, NSTEMI, and STEMI will be discussed and illustrated through the use of simulated clinical scenarios. Emergent assessment, diagnostic measures, and initial treatment options will be explored, followed by a discussion of follow-up care and preparation for discharge. Key points of secondary prevention, including smoking cessation, treatment of dyslipidemia, and modification of other risk factors, will be outlined.
Since the early 1990s, an enhanced understanding of the pathogenesis of CHD has helped to create a framework for defining ischemic heart disease. The AHA/ACC define ACS as "a spectrum of conditions compatible with acute myocardial ischemia and/or infarction that are usually due to an abrupt reduction in coronary blood flow" [3]. The concept of ACS is helpful, as the initial clinical presentations of UA, NSTEMI, and STEMI often appear similar. However, UA/NSTEMI and STEMI differ in many ways, including their prevalence, severity, pathophysiology, clinical presentation, treatment, and prognosis.
In patients with CHD, transient imbalances can occur in the supply and demand of oxygen to the myocardium. This ischemia can manifest as precordial chest discomfort, or angina pectoris. Angina is considered stable when it is precipitated by stress or exertion and rapidly resolves with rest or the use of nitrates. Angina is considered unstable when it occurs suddenly (without a precipitating factor); it may occur at rest and may increase in frequency or severity. With both stable angina and UA, ischemia is fully reversible, with no evidence of myocardial necrosis as indicated by elevated levels of serum cardiac biomarkers (e.g., cardiac troponin) [3]. UA may or may not be associated with signs of ischemic changes on electrocardiography (ECG), such as ST-segment depression or new T-wave inversion [3].
UA is closely related to NSTEMI, and the two entities are often indistinguishable from each other, especially during the initial evaluation of a patient [3]. Recognizing the continuum of UA and NSTEMI, the authors of the 2014 AHA/ACC guideline for the management of the conditions created the term NSTE-ACS (non–ST-elevation acute coronary syndromes) to replace "UA/NSTEMI" [3]. Unlike UA, NSTEMI is associated with myocardial necrosis and resultant release of cardiac biomarkers. In addition, the ECG usually shows ST-segment depression, transient ST-elevation, and/or prominent T-wave inversions, but these findings are not required for a diagnosis of NSTEMI [3]. In contrast, STEMI is associated with myocardial damage, with both elevated serum cardiac biomarker levels and persistent ST-segment elevation on ECG [2].
An MI was once defined according to symptoms, ECG abnormalities, and serum cardiac enzyme levels. The advent of more sensitive and specific cardiac biomarkers and imaging studies has led to an ability to detect smaller amounts of myocardial necrosis and, in turn, a need for a more precise definition of MI. The European Society of Cardiology (ESC), the American College of Cardiology Foundation (ACCF), the AHA, and the World Heart Federation jointly developed a consensus document establishing a universal definition of MI, which was most recently updated in 2018 [22]. Among the new concepts introduced, the updated definition differentiates MI from myocardial injury [22]. According to the consensus document, type 1 MI may be diagnosed with the detection of a rise and/or fall of cardiac biomarker levels (preferably high-sensitivity cardiac troponins) with at least one value above the 99th percentile of the upper reference limit (URL) and with at least one of the following [22]:
Symptoms of acute MI
New ischemic ECG changes
Development of pathologic Q waves in the ECG
Imaging evidence of new loss of viable myocardium or new regional wall motion abnormality in a pattern consistent with an ischemic etiology
Identification of an intracoronary thrombus by angiography or autopsy
Type 2 MI may be diagnosed with the detection of a rise and/or fall of cardiac troponin values with at least one value above the 99th percentile URL, and evidence of an imbalance between myocardial oxygen supply and demand unrelated to acute coronary atherothrombosis, and at least one of the following [22]:
Symptoms of acute MI
New ischemic ECG changes
Development of pathologic Q waves on ECG
Imaging evidence of new loss of viable myocardium or new regional wall motion abnormality in a pattern consistent with an ischemic etiology
Other types are defined as occurring in conjunction with percutaneous coronary intervention (PCI), coronary artery bypass grafting (CABG), or stent thrombosis; secondary to increased oxygen demand or decreased supply (e.g., coronary artery spasm, arrhythmias); or sudden cardiac death [22]. The consensus document also coins the term MI with nonobstructive coronary arteries (MINOCA) to describe patients with MI and no angiographic obstructive coronary artery disease. The prevalence of MINOCA is estimated to be 6% to 8% among patients diagnosed with MI and appears to be more common in women than men as well as in patients presenting with NSTEMI compared with those presenting with STEMI [22].
A man presents to the emergency room with complaints of chest pain and shortness of breath. He describes the chest pain as "crushing." When asked to identify the location of the pain, he points to the left substernal area of his chest. He denies previous episodes of chest pain. His initial electrocardiogram (ECG) shows non-specific ST wave changes, and his initial cardiac biomarkers are within normal limits. He is admitted to the cardiology unit with an initial diagnosis of unstable angina.
An elderly man collapses at home. Unable to arouse him, his family calls emergency services. When the paramedics arrive they find him to be in ventricular fibrillation and promptly defibrillate, restoring normal rhythm. An ECG obtained en route shows ST wave changes indicative of an MI. Emergency medical services (EMS) notifies the emergency department that they have a probable ST elevation MI patient en route and call for a STEMI alert.
A young woman presents to the emergency department with complaints of severe chest pain. She is tachycardic with an elevated blood pressure. She has no history of cardiac disease. Her cardiac enzymes are positive for MI, but her 12-lead ECGs show no ST-wave changes. She is admitted to the hospital with diagnosis of NSTEMI.
A woman presents to her primary care physician with complaints of increasing episodes of chest pain. Her physician notes that she was diagnosed with stable angina approximately 3 years earlier. Her "typical" angina attack was precipitated by exertion (walking more than five blocks or climbing a flight of stairs). Now, the patient reports that her angina attacks are occurring at rest and occasionally awaken her at night. A 12-lead ECG in the physician's office shows no characteristic ST wave changes. The patient is sent to the local emergency department with a tentative diagnosis of ACS/UA.
Each of these individuals has ACS.
CHD, which encompasses angina pectoris (stable angina), coronary insufficiency (UA), MI, and CHD-related death, affects an estimated 20.1 million Americans 20 years and older in the United States [23]. CHD is the leading cause of death in the United States, accounting for 23.1% of all deaths [24]. It is estimated that each year an estimated 1,055,000 individuals will have a new coronary attack or a recurrent episode [23]. In addition, approximately 170,000 silent first MIs will occur. As a chronic disease, CHD has a significant impact on quality of life, negatively affecting physical, psychologic, and social well-being. CHD also carries a tremendous economic burden: an estimated direct and indirect cost of $219.6 billion [23].
Atherosclerosis, the underlying condition of CHD, is progressive, with periods of stable and nonstable disease. Periods of instability can cause the occurrence of ACS, a spectrum of life-threatening disorders that includes UA, NSTEMI, and STEMI. More than 1 million hospitalizations in 2016 were associated with a primary or secondary discharge diagnosis of ACS [23]. As with CHD, the financial cost associated with ACS is high; the mean cost for the first ACS admission is more than $71,300 [23].
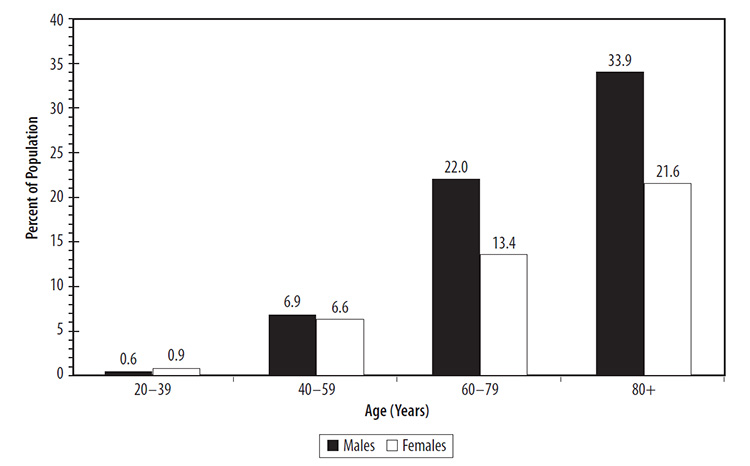
The overall prevalence of CHD among adults is 7.2%, with a higher prevalence among men compared with women (8.3% vs. 6.2%) [23]. The prevalence increases with age, with the highest rates found among people 80 years and older (Figure 1) [23]. Women tend to be older than men at the time of a first cardiac event [11,25,26].
The prevalence of CHD, MI, and angina vary considerably according to gender and race/ethnicity. For CHD, the rate is highest for White men (8.7%) and lowest for Asian women (3.2%). The prevalence of MI is highest for White men (4.4%) and lowest for White and Asian women (2.0% and 0.7%, respectively) (Table 1) [23]. The prevalence of angina is highest for Black women (4.7%) and lowest for Asian women (2.2%) [23].
PREVALENCE OF CORONARY HEART DISEASE (CHD), MYOCARDIAL INFARCTION (MI), AND ANGINA AMONG ADULTS 20 YEARS AND OLDER ACCORDING TO RACE/ETHNICITY
| Condition | Men | Women | ||||||
|---|---|---|---|---|---|---|---|---|
| White | Black | Hispanic | Asian | White | Black | Hispanic | Asian | |
| CHD | 8.7% | 6.7% | 6.8% | 5.0% | 6.0% | 7.2% | 6.4% | 3.2% |
| MI | 4.4% | 3.9% | 3.7% | 2.7% | 2.0% | 2.3% | 2.1% | 0.7% |
| Angina | 4.5% | 3.3% | 3.5% | 2.1% | 4.0% | 4.7% | 4.3% | 2.2% |
ACS is also more prevalent among men; 615,000 of the more than 1.05 million unique hospitalizations for ACS (as a primary or secondary discharge diagnosis) occurred among men, compared with 430,000 among women [23]. Of all of these unique hospitalizations, 1.02 million were for MI alone, and 23,000 were for UA alone [23]. Data on the population characteristics of patients with MI in the ACTION Registry-GWTG provide insight on racial/ethnic variations in MI. Among 667,424 patients, approximately 86.5% were White, 8.8% were Black, and 2.8% were Asian; 0.7% and 0.3% were American Indian/Alaskan or Hawaiian/Pacific Islander, respectively [28]. In addition, approximately 5.8% were of Hispanic or Latino ethnicity [28].
The incidence of STEMI has decreased since 2003, while the incidence of NSTEMI has increased [2]. STEMI continues to be less prevalent than NSTEMI, accounting for 39% of MIs [23]. However, STEMI is more common than NSTEMI among younger patients, with a rate of nearly 30% among patients younger than 55 years of age and 30% among patients 55 to 64 years of age [28]. STEMI is also more common among some racial/ethnic groups; for example, STEMI accounted for a slightly higher proportion of the MIs among White, Asian, and Hispanic/Latino individuals (Table 2) [28].
PREVALENCE OF NON-ST-ELEVATION MYOCARDIAL INFARCTION (NSTEMI) AND ST-ELEVATION MYOCARDIAL INFARCTION (STEMI) ACCORDING TO RACE/ETHNICITY
| Type of MI | White | Black | Asian | AI/AN | Hawaiian/PI | Hispanic or Latino Ethnicity |
|---|---|---|---|---|---|---|
| NSTEMI (111,535) | 83.4% | 13.0% | 1.9% | 0.9% | 0.2% | 6.6% |
| STEMI (71,368) | 85.7% | 10.1% | 2.5% | 0.7% | 0.2% | 6.7% |
| AI = American Indian, AN = Alaskan Native, PI = Pacific Islander. | ||||||
As noted, CHD-related mortality rates continue to decrease; the annual rate decreased 27.9% from 2008 to 2018, and the actual number of deaths decreased approximately 9.8% during that time [23]. Heart disease is still the overall leading cause of death in the United States and represents a similar proportion of all deaths for men and women (24.3% vs. 21.8%) [24]. CHD-related mortality varies by age, with CHD accounting for 11.5% of all deaths among people 45 to 54 years of age, approximately 24.5% of all deaths among people 65 to 74 years of age, and approximately 21.5% of all deaths among people 85 years of age and older [24]. CHD-related mortality is higher among men than women across all age groups, except among those 85 years of age and older where the mortality rate is higher among women [24].
With regard to race, CHD is the leading cause of death among all racial/ethnic populations (Table 3) [24]. Heart disease is the leading cause of death among non-Hispanic White, non-Hispanic Black, and American Indian/Alaska Native populations, and the second leading cause of death in the non-Hispanic Asian/Pacific Islander and Hispanic populations.
CORONARY HEART DISEASE (CHD) AS A PERCENTAGE OF ALL DEATHS ACCORDING TO RACE AND ETHNICITY
| Racial/Ethnic Population | CHD as Percentage of All Deaths |
|---|---|
| Race | |
| White | 23.4% |
| Black | 23.5% |
| Asian | 21.2% |
| American Indian/Alaska Native | 17.8% |
| Native Hawaiian/Other Pacific Islander | 24.9% |
| Ethnicity | |
| Non-Hispanic White | 23.4% |
| Non-Hispanic Black | 23.5% |
| Hispanic | 19.7% |
Improved adherence to evidence-based guidelines has been associated with decreased mortality rates after ACS events. Rates of short-term morbidity and mortality are higher for STEMI than for NSTEMI. A review of data in the National Cardiovascular Data Registry ACTION Registry-GTWG showed in-hospital mortality rates of approximately 6% to 8% for STEMI and rates of approximately 0.5% to 5.5% for NSTEMI [28,29]. The rate of in-hospital cardiogenic shock has also been higher among patients with STEMI (4.4% vs. 1.6%), whereas the rates of in-hospital reinfarction, heart failure, and stroke have been similar (0.8% vs. 0.5%, 4.5% vs. 4.2%, and 0.6% vs. 0.6%, respectively) [28]. At one year, however, the risk of mortality is similar for STEMI and NSTEMI [30].
The underlying cause of ACS is a form of atherosclerosis known as CHD. In CHD, lipids, calcium, fibrin, and other cellular substances/cellular debris are deposited in the lining of the arteries, forming atherosclerotic plaques at sites with low-velocity blood flow (e.g., branch points, inner curvatures) [31]. Although the exact mechanisms are not completely understood, most researchers agree that injury to the inner (endothelial) layer of the artery initiates a series of biochemical events that result in the formation of atherosclerotic plaque. High levels of low-density lipoprotein (LDL) alone can cause atherosclerosis; however, it is most often the case that lower levels of LDL combined with other identified risk factors, including cigarette smoke, low levels of high-density lipoprotein (HDL), hypertension, diabetes, male sex, and family history, lead to atherosclerosis [31]. Individuals with very low LDL typically do not develop clinically significant atherosclerotic plaques, even in the presence of these risk factors.
When the endothelium is injured, an inflammatory response is triggered at the site of the injury. Circulating monocytes respond to the site and become macrophages. These cells act as scavengers, taking up the LDL cholesterol that has penetrated the vessel wall and forming the characteristic foam cell seen in early atherosclerosis. Xanthomas (fatty streaks), the precursors of an atherosclerotic lesion, may be observed in many individuals by 20 years of age. Through complicated mechanisms that include proliferation of smooth muscle cells in the arterial wall and the deposit of extracellular connective tissue, a complex atherosclerotic plaque develops consisting of a fibrous cap overlying a rich lipid core. The fibrous cap may be thick, providing a dense barrier between the circulating blood and the lipid core; this type of lesion is referred to as stable and is less likely to be injured by substances circulating in the blood stream. On some plaques, the fibrous cap is thin and more susceptible to injury; referred to as vulnerable plaque, this type of lesion is more at risk to rupture or erode, causing thrombus formation and disruption of blood flow [1,32,33,34]. Vulnerable plaque has the following hallmark characteristics [31,35]:
Large lipid core (more than 40% of the total lesion area)
Thin, fibrous cap (usually less than 65 micrometers)
High infiltration of macrophages
Few smooth muscle cells
Expansive remodeling preserving the lumen
Neovascularization from the vasa vasorum
Adventitial/perivascular inflammation
Spotty calcification
Growth of plaque narrows the lumen of the affected vessel(s); this disrupts normal blood flow, reduces the blood and oxygen available to the tissue supplied by the vessel, and creates increased turbulent blood flow at the site of the plaque. Initially, the coronary artery responds to the growth of the plaque/narrowing of the vessel lumen through a process of vascular remodeling. In vascular remodeling, the artery enlarges to compensate for the narrowing lumen. However, as the atherosclerotic process continues, the vessel lumen becomes stenosed, unable to dilate or constrict in response to metabolic demands [1,32,33,34].
At one time, it was thought that plaque simply continued to grow larger and larger until the lumen of the affected vessel was totally occluded, disrupting the blood flow and oxygen supply to part of the myocardium. However, today it is acknowledged that the process is much more complex [31,36,37]. Research has shown that the precipitating cause of acute myocardial ischemia is not the plaque itself. Instead, acute ischemia occurs when a thrombus forms in the area of plaque, partially or totally occluding the vessel lumen [1,32,33,34].
It should be noted that atherosclerotic plaques are different from xanthomas. Xanthomas are accruals of foam cells that can be seen with the naked eye after several layers have deposited just beneath the endothelium. These fatty streaks are even present in some fetal and infant aortas, due to maternal risk factor influence, but decline in the years after birth. Xanthomas commonly reappear in adolescence in susceptible areas of the arterial tree (e.g., coronary arteries, aorta), and by 20 to 30 years of age, pathologic intimal thickening (formed by isolated lipid pools) is present in many individuals. Not all xanthomas progress, but those at predilection sites may begin to accumulate acellular lipids and cellular debris, forming a necrotic core. These lipid-rich, debris-filled necrotic cores are irreversible. Why some lesions progress to necrosis is not known, but by 30 years of age many more atherosclerotic plaques have developed in men than in women, despite similar numbers of xanthomas in both [31].
Formation of a thrombus occurs when the fibrous cap of an atherosclerotic lesion erodes or ruptures, exposing the red cell-rich lipid core to circulating blood. It is thought that the same stimuli that are responsible for the initial injury to the vessel wall are also responsible for causing erosion or rupture of vulnerable plaque (i.e., inflammation). Cigarette smoking and high levels of circulating LDL head the list of injurious agents along with hypertension and diabetes [1,31,32,33,34].
Plaque rupture generally begins where the cap is thinnest and has the highest infiltration of macrophages, which release lytic enzymes and toxic metabolites that act to degrade the cap, leading to rupture [31]. Plaque rupture triggers the formation of a thrombus when thrombogenic elements of the lipid core are exposed to circulating blood; rupture and thrombosis may occur at the same time, but a temporary increase in stress (emotional or physical) may be the trigger for a cardiac event. However, a life-threatening luminal thrombus develops only occasionally; it is theorized that other factors are involved, such as thrombogenicity of the exposed plaque material, local flow disturbances, and systemic thrombotic propensity [31]. The presence of plaque material interspersed in a thrombus indicates that severe thrombosis developed immediately after plaque rupture; more often, however, the thrombus develops over several days before an ACS event [31]. In one study, the thrombus was days or weeks old in 49% of patients with STEMI [38]. Researchers have used a variety of imaging techniques to determine the distribution of thin-capped fibroatheromas (TCFAs), and the lesions are most often found in the proximal third of the major coronary arteries, although the left circumflex and right coronary arteries were affected evenly throughout their length in one study [39,40,41]. The findings of another study suggest that TCFAs causing ACS events are also more likely to be found in proximal locations and that the left main coronary artery was less commonly affected [42].
Why some plaque ruptures cause an ACS event and most do not is unclear. Plaque rupture in nonculprit lesions has been found in approximately 14% of patients with ACS, and among these lesions, plaque burden was significantly greater in lesions with plaque rupture than in lesions without plaque rupture [43]. Plaque rupture in combination with large plaque burden and luminal narrowing appears to lead to ACS [2]. Lipid-rich plaque and intracoronary thrombus have been found significantly less often in patients with asymptomatic CHD compared with patients with NSTEMI [44].
It was once thought that the degree of occlusion caused by a thrombus differentiated STEMI from NSTEMI, with complete and sustained occlusion resulting in STEMI, and incomplete or transient occlusion resulting in NSTEMI [45]. However, research is challenging this theory; for example, studies have shown that the degree of stenosis in some cases of acute MI is not severe enough to limit blood flow [45]. Other studies have demonstrated that ACS is often associated with plaque with little or no calcification and positive vessel remodeling (outward expansion of the artery wall) and that plaque rupture, TCFAs, and red thrombus are significantly more common with STEMI than with NSTEMI [27,46].
When a thrombus occludes a coronary artery, oxygen supply to the area of the heart supplied by that vessel is reduced. When the supply becomes insufficient to meet the tissue's metabolic demands, the myocardial cells become ischemic; ischemia can develop within 10 seconds. After 1 minute of inadequate oxygen supply, the heart's function is affected. Irreversible tissue death and damage will occur after 20 minutes of ischemia [34].
While thrombus formation is the most common cause, several other etiologies may cause ACS. These include cocaine and methamphetamine toxicity and variant angina.
The acute effects of cocaine use include coronary artery vasoconstriction/vasospasm, coronary dissection, thrombus formation, and increased myocardial oxygen demand. Cocaine toxicity creates a setting in which oxygen demand is increased and supply is reduced, leading to ischemia and increased potential for infarction. Patients with cocaine toxicity present with a clinical picture that is almost identical to that of non-cocaine-related ACS. The "typical" patient who presents with cocaine-induced ACS is a male younger than 50 years of age, is a smoker, has used cocaine within several hours before the onset of symptoms, and has few risk factors for CHD. Research has found that long-term effects of cocaine use include the development of premature atherosclerosis, progressive myocyte damage, and hypertrophy of the left ventricle [3,34,47,48].
Methamphetamine can also induce ACS. The acute effects of methamphetamine include arrhythmias, hypertension, and tachycardia, and MI may result from coronary spasm or plaque rupture due to increased platelet aggregation [3]. Chronic methamphetamine use is associated with cardiomyopathy, myocarditis, necrotizing vasculitis, and pulmonary hypertension.
Also known as variant or Prinzmetal angina, vasospastic angina is caused by vasospasm of the coronary arteries. With vasospasm, the affected artery tightens and narrows. Blood flow through the artery is significantly decreased, reducing the amount of oxygen reaching the tissue. Vasospasm usually occurs spontaneously but may be precipitated by a stress factor such as exercise, hyperventilation, or cold. Smoking increases the risk that a person may develop vasospastic angina. Variant angina may be characterized by transient, intermittent chest pain; the chest pain may occur at rest. With severe spasm that produces almost total occlusion of a vessel, ST-segment elevation may be seen on ECG. This elevation resolves when the spasm is relieved. Variant angina can occur in the absence of atherosclerotic disease but may occur in the area of plaque in persons with CHD [3,34,47].
For the myocardium to conduct electrical impulses, contract, and pump blood effectively, it requires both oxygen and adenosine 5B-triphosphate (ATP) (Table 4). When blood flow is interrupted, cells are immediately deprived of their oxygen supply. Anaerobic metabolism of glycogen occurs, and less ATP is produced. Without adequate oxygen and ATP, the sodium-potassium and calcium pumps in the myocardium begin to fail. Hydrogen ions and lactate accumulate, resulting in acidosis. The heart's ability to conduct electrical impulses and to contract becomes impaired. Cardiac output drops, and arrhythmias can develop. If the damage to the myocardium is severe, cardiogenic shock will develop [1].
OVERVIEW OF CORONARY CIRCULATION
|
The vessels that supply the myocardium with oxygen and nutrients are called the coronary arteries. Because these arteries lie on the surface of the myocardium, they are sometimes referred to as epicardial coronary arteries. Two main arteries, known as the right coronary artery and the left coronary artery, emerge from the aorta, very near the top of the heart. The right coronary artery supplies blood to the posterior part of the left ventricle, as well as to the right atrium and right ventricle. Occlusions of the right coronary artery can cause ischemia, injury, or infarction of the right atrium, right ventricle, and the back (or posterior) wall of the left ventricle. The left coronary artery consists of three main segments. Together, the three segments supply a large part of the myocardium with blood. The initial segment arising from the aorta is called the left main coronary (or the left main). The left main coronary quickly branches into two arteries known as the left anterior descending coronary artery and the left circumflex coronary artery. The left anterior descending artery supplies blood to the anterior wall of the left ventricle, the interventricular septum, the right bundle branch, and part of the left bundle branch. The left circumflex circles around the left side of the heart, supplying the lateral wall of the left ventricle, the left atrium, and a posterior part of the left bundle branch. Occlusions of the left main coronary artery are extremely dangerous because obstruction at that level disrupts blood flow through both the left anterior descending artery and the circumflex, causing ischemia, injury, or infarct of a large part of the heart muscle. |
When the body senses the drop in cardiac output and blood pressure that occur in the acute phase of myocardial ischemia, compensatory mechanisms activate in an attempt to maintain adequate circulation to vital organs. The sympathetic nervous system (SNS) stimulates the release of the hormones epinephrine and norepinephrine; as a result, heart rate and blood pressure increase [1]. Instead of helping the heart compensate for reduced blood flow and oxygen demands, these mechanisms increase myocardial workload and increase myocardial oxygen demands. In addition, the drop in cardiac output triggers the release of renin and angiotensin by the kidney, causing vasoconstriction and retention of sodium and water in an attempt to compensate for reduced output. The amount of blood volume in the ventricles at the end of diastole increases, again increasing myocardial workload and myocardial oxygen demand. Because the oxygen supply to the myocardium is already inadequate, increasing the demands accelerates the ischemic process. Ischemic tissue can become necrotic, resulting in irreversible damage [1]. If more than 40% of the myocardium is damaged, circulatory collapse and cardiogenic shock can result. There is also an increased risk of life-threatening arrhythmias developing during ischemia and infarction [1,32,33,34].
The impact of MI on the heart's ability to maintain adequate cardiac output depends on whether the damage to the myocardium is reversible ischemia or permanent necrosis and the extent and location of the ischemia/infarction [1,32,33,34]. Ischemia causes an immediate impairment of pumping function in the affected tissue; if blood flow is restored, this loss is temporary. If necrosis occurs, the ability of the affected tissue to conduct electrical impulses and contract normally is permanently impaired. In terms of location and extent, factors include the coronary artery or branch involved and where the occlusion is located in the vessel. Lesions in the proximal part of a vessel can result in more damage than lesions in the very distal portion. The part of the heart muscle supplied by the affected artery is also important.
Other complications can occur after acute MI, including pericarditis and left ventricular aneurysm [34]. Pericarditis is inflammation of the pericardial sac surrounding the heart. This condition may develop within days of an infarction, or it may not develop until several weeks later. A common symptom is chest pain that is described as sharp and severe; it often worsens with inspiration and may be relieved when the individual sits up and leans forward. A pericardial friction rub may be auscultated. ST-segment elevations may be seen on 12-lead ECG. Unlike the ST-segment elevations seen in STEMI that occur in the specific leads facing the area of infarct in the heart, in pericarditis, ST segments throughout all 12 leads may be elevated. Nonsteroidal anti-inflammatory drugs (NSAIDs) should not be used to treat pericarditis in the immediate post-infarction period.
When infarction damages the full thickness of the myocardium, the area of damage initially thins. The damaged area loses the ability to conduct electrical impulses or to contract. In the initial period following acute MI, this tissue is very weak and may rupture. As scar tissue forms in the area, the damaged tissue is strengthened but is still unable to conduct electrical impulses or contract. If the area is large enough, an aneurysm can result. This aneurysm is not at risk to rupture, but its presence severely impairs the ability of the left ventricle to contract and maintain cardiac output. Congestive heart failure can result. In some cases, the aneurysm can be surgically resected; removal of the inert, non-contractile tissue has been found to improve overall pumping of the left ventricle. Left ventricular aneurysm formation is associated with infarctions of the anterior and lateral walls of the left ventricular.
Some risk factors for CHD were established many years ago, and researchers continue to seek to identify other risk factors that add predictive value to traditional risk factors.
The Framingham Heart Study identified the first risk factors, and these factors were integrated into a risk-assessment tool, the Framingham Risk Score [49]. The factors in the Framingham Risk Score include age, total cholesterol level, HDL level, systolic blood pressure, treatment for hypertension, and cigarette smoking, and the score is used to determine the 10-year risk of so-called hard CHD (defined as MI or coronary-related death) among asymptomatic adults. The Framingham risk score is one of several scores that involve several traditional risk factors for assessing risk; other scores recommended include the Systematic Coronary Risk Evaluation (SCORE), PROCAM (men) and Reynolds (separate scores for men and women) [50]. The use of one of these risk calculators is a class IB recommendation from the American College of Cardiology Foundation and American Heart Association [50]. It is important to consider the populations on which these risk scores are based. For example, the Framingham Risk Score was developed on the basis of risk factors identified in the Framingham Heart Study, which involved a primarily White, middle-aged population. When the risk score has been evaluated in other populations, it has been found to underestimate the risk of CHD among older (mean age: 73.5 years) Black and White individuals, especially women [51]. ACC/AHA guidelines published in 2013 recommend that race- and sex-specific Pooled Cohort Equations be used to predict 10-year risk of a first hard atherosclerotic cardiovascular disease event in non-Hispanic Black and non-Hispanic White individuals (class IB) [52]. These equations were developed on the basis of data on participants from several large racially and geographically diverse studies [52]. The guidelines also note that the sex-specific pooled cohort equations for non-Hispanic White individuals may be considered to estimate risk for people other than Black and non-Hispanic White individuals (class IB) [52].
Primary care providers are also encouraged to routinely evaluate the presence of individual CHD risk factors, and the U.S. Preventive Services Task Force (USPSTF) has recommended routine screening for hypertension and dyslipidemia as well as counseling and pharmacologic interventions for smoking cessation [53,54,55].
Many nontraditional risk factors have been evaluated for their usefulness in enhancing the estimation of CHD risk, and the ACC/AHA has issued evidence-based recommendations according to individual risk (Table 5) [50,52]. The nontraditional risk factors that have been evaluated most often are inflammatory markers, lipid-related markers, other biochemical markers, testing for subclinical atherosclerosis, ECG, and imaging studies.
EVIDENCE-BASED RECOMMENDATIONS FOR USE OF NONTRADITIONAL RISK FACTORS TO EVALUATE CHD RISK IN ASYMPTOMATIC ADULTS
| Nontraditional Risk Factor | Recommendation (Class, Level of Evidence) | |||||
|---|---|---|---|---|---|---|
| Family history of CHD |
| |||||
| Family history of atherothrombotic CHD | Recommended for all asymptomatic adults (IB) | |||||
| Genomic testing | Not recommended (IIIB) | |||||
| Lipoprotein and apolipoprotein assessments | Not recommended (IIIC) | |||||
| Natriuretic peptides | Not recommended (IIIB) | |||||
| C-reactive protein |
| |||||
| Hemoglobin A1C |
| |||||
| Testing for microalbuminuria |
| |||||
| Lipoprotein-associated phospholipase A2 | Might be reasonable for asymptomatic adults at intermediate risk (IIbB) | |||||
| Resting electrocardiography (ECG) |
| |||||
| Transthoracic echocardiography (to detect left ventricular hypertrophy) |
| |||||
| Measurement of carotid intima-media thickness |
| |||||
| Brachial/peripheral flow-mediated dilation | Not recommended (IIIB) | |||||
| Measurement of arterial stiffness | Not recommended outside of research settings (IIIC) | |||||
| Measurement of ankle-brachial index |
| |||||
| Exercise ECG | May be considered for asymptomatic adults at intermediate risk (IIbB)c | |||||
| Stress echocardiography | Not indicated for asymptomatic adults at low or intermediate risk (IIIC) | |||||
| Stress myocardial perfusion imaging |
| |||||
| Coronary artery calcium scoring |
| |||||
| Coronary computed tomography angiography | Not recommended for asymptomatic adults (IIIC) | |||||
| Magnetic resonance imaging of plaque | Not recommended for asymptomatic adults (IIIC) | |||||
| ||||||
The recognition of the important role of inflammation in the development of CHD has led to increased research on the value of inflammatory markers in predicting risk. C-reactive protein (CRP) is the marker that has been most rigorously studied. The USPSTF found moderate, consistent evidence that adding a CRP level to a risk algorithm improves risk stratification for individuals at intermediate risk, and the 2010 ACCF/AHA guideline subsequently noted that measuring the CRP level may be reasonable for asymptomatic men (50 years of age or younger) or women (60 years of age or younger) who are at intermediate risk for cardiovascular disease [50,56]. The ACCF/AHA guideline does not recommend a CRP level for asymptomatic adults at high risk [50]. One study suggested improved 10-year risk prediction when a CRP or fibrinogen level was added to a traditional risk score [57]. A later ACCF/AHA guideline notes that a high-sensitivity CRP may be considered when a risk-based treatment decision is uncertain after quantitative risk assessment [52].
The USPSTF found no evidence that homocysteine levels or leukocyte counts were useful in further stratifying risk among individuals at intermediate risk [58].
The 2010 ACCF/AHA guideline for assessment of cardiovascular risk does not recommend assessment of lipoprotein or apolipoprotein levels [50]. Measurement of a lipoprotein-associated phospholipase A2 level "might be reasonable" for asymptomatic adults at intermediate risk [50]. In a study published after the ACCF/AHA guideline, the prediction of CHD improved slightly when information on apolipoprotein B and A-I, lipoprotein(a), or lipoprotein-associated phospholipase A2 mass was added to risk scores that included total cholesterol and HDL levels [59]. However, the 2013 ACCF/AHA guideline notes that the contribution of apolipoprotein B is uncertain [52].
According to the 2010 ACCF/AHA guideline, natriuretic peptide levels are not recommended for the evaluation of risk among asymptomatic adults [50]. A hemoglobin A1C "may be reasonable" for assessing risk in asymptomatic adults without diabetes and "may be considered" for asymptomatic adults with diabetes [50]. This guideline also notes that testing for microalbuminuria is reasonable for asymptomatic adults with hypertension or diabetes and "might be reasonable" for asymptomatic adults with hypertension or diabetes who are at intermediate risk [50]. However, in its 2013 guideline, the ACCF/AHA expert panel notes that the contribution of albuminuria is uncertain [52].
Historically, screening for atherosclerosis has been done through measurement of lipid levels as surrogate markers. Now, coronary artery calcium scoring has become a strong risk predictor, improving risk classification of asymptomatic adults when the score is combined with traditional risk factors [60,61]. The 2010 ACCF/AHA guideline notes that calcium scoring is reasonable for asymptomatic adults at intermediate risk (10-year risk of 10% to 20%), and for asymptomatic adults (40 years and older) who have diabetes and "may be reasonable" for individuals at low-to-intermediate risk (10-year risk of 6% to 10%) [50]. The test is not recommended for persons at low risk (10-year risk of less than 6%). Similarly, 2010 appropriate use criteria state that determination of a coronary calcium score with noncontrast computed tomography (CT) is appropriate for individuals with a family history of premature CHD and for asymptomatic individuals with no known CHD who are at intermediate risk [62]. Subsequent systematic reviews have confirmed that coronary artery calcium scoring has additional predictive value (in combination with traditional risk factors), primarily for asymptomatic individuals at intermediate risk [63,64]. The 2013 ACCF/AHA guideline notes that a coronary artery calcium (CAC) score may be considered if a risk-based treatment decision is uncertain after quantitative risk assessment [52].
The clinical utility of other tests for identifying subclinical disease is not as clear. In 2009, the USPSTF found no evidence that measurement of carotid intima-media thickness or ankle-brachial index were useful in further stratifying risk among individuals at intermediate risk [58]. However, the 2010 ACCF/AHA guideline notes that measurement of carotid intima-media thickness and ankle-brachial index is reasonable for asymptomatic adults at intermediate risk; however, the 2013 ACCF/AHA guideline does not recommend routine measurement of carotid intima-media thickness and states that ankle-brachial index may be considered if a risk-based treatment decision is uncertain after quantitative risk assessment [50,52]. The 2010 ACCF/AHA guideline does not recommend measurement of flow-mediated dilation or arterial stiffness as part of risk assessment [50]. Still more recently, systematic reviews have shown that measurement of flow-mediated dilation and carotid intima-media thickness had additional predictive value (in combination with traditional risk factors), primarily for asymptomatic individuals at intermediate risk [63,64]. Magnetic resonance imaging of plaque is not recommended [50].
The ACC/AHA, American College of Physicians (ACP), and USPSTF have all recommended against routine screening with resting ECG and exercise treadmill test for asymptomatic individuals at low risk [50,64,65,66]. The 2010 ACCF/AHA guideline notes that exercise ECG "may be considered" for asymptomatic adults at intermediate risk, but the USPSTF notes that there is insufficient evidence to assess the balance of benefits and harms of such screening among asymptomatic adults at intermediate or high risk [50,66].
The 2010 ACCF/AHA guideline and the ACP screening guideline note that stress echocardiography is not indicated for asymptomatic adults at low or intermediate risk [50,65]. Transthoracic echocardiography (to detect left ventricular hypertrophy) is not recommended for asymptomatic adults but "may be considered" for asymptomatic adults with hypertension. Coronary CT angiography is not recommended for asymptomatic adults. Stress myocardial perfusion imaging is not indicated for asymptomatic adults at low or intermediate risk but "may be considered" for assessment of advanced cardiovascular risk in asymptomatic adults with diabetes or with a strong family history of CHD [50,65].
Primary prevention interventions should be implemented when a patient has one or more risk factors. Recent guideline updates have created shifts away from established goals and thresholds for interventions, especially with regard to hypertension and dyslipidemia.
The 2017 Guideline for High Blood Pressure in Adults sets goals for systolic and diastolic blood pressure and provides evidence-based recommendations on treatment approaches [67]. This guideline replaces the report from the Eighth Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC8). One study showed that fewer adults in the United States would need antihypertension treatment according to the JNC8 recommendations, compared with the JNC7 recommendations, while another study indicated that more cardiology patients with hypertension would be treated [68,69]. The 2017 Guideline for High Blood Pressure in Adults consolidates the recommendations for most major organizations, including the American Society of Hypertension [70]. The authors of a meta-analysis found that, although antihypertension treatment provides similar benefit for individuals at all levels of baseline risk of CHD, the absolute risk reductions are progressively greater as baseline risk increases [71].
With regard to the treatment of cholesterol levels, ACC/AHA guidelines published in 2013 differ greatly from the National Cholesterol Education Program (NCEP) guideline in 2001, with a substantially greater number of people eligible for treatment with cholesterol-lowering drugs, especially within the population of individuals at moderate risk of CHD [72,73,74,75]. The new guideline matches statin assignment to total plaque burden better than the NCEP guideline, according to a study in which plaque burden was determined by CT angiography [76]. A clinician-patient risk discussion is recommended to ensure that patients understand the benefits of risk-reduction interventions, potential adverse effects, drug-drug interactions, and patient preferences [77]. This approach also has the potential to enhance patient adherence to medication.
Increased emphasis has been placed on better management of lifestyle habits as primary prevention of CHD. Lifestyle risk factors such as obesity, poor diet, and physical inactivity have a great influence on traditional risk factors such as blood pressure and cholesterol levels, as well as on novel risk factors, such as inflammation and endothelial function [78]. Lifestyle management is a key component of the new guidelines for the treatment of cholesterol levels and hypertension, and several other guidelines have addressed issues related to lifestyle behaviors, such as obesity, diet, and physical activity. The ACC/AHA/TOS (The Obesity Society) developed a guideline on the management of overweight and obesity, and some members of the Expert Panel authored a separate review on the evidence statements related to cardiovascular risk [79,80]. The AHA/ACC also published a guideline on lifestyle management to reduce cardiovascular risk in 2013 [81]. In its guideline of cardiac screening, the ACP notes that strategies to improvement lifestyle behaviors should be emphasized [65]. The USPSTF recommends counseling to promote a healthful diet and physical activity to prevent cardiovascular disease, and the AHA focuses on changing lifestyle behaviors in its guide for improving cardiovascular health at the community level [82,83,84]. The decision to offer or refer adults without cardiovascular risk factors to behavioral counseling should be individualized by the primary care provider [85].
Another aspect of prevention that warrants increased attention is the role of complementary and alternative medicine. Approximately 33% of adults use complementary and alternative medicine therapy (including dietary supplements), and 40% to 70% do not tell their doctors about the therapy [86,87,88]. Systematic reviews have shown that there is insufficient evidence to support the primary prevention of cardiovascular disease with multivitamins, co-enzyme Q10, selenium supplement, green or black tea, or tai chi [89,90,91,92,93]. Studies have shown that a Mediterranean diet has a beneficial effect on cardiovascular risk factors, although the evidence is limited [94]. The USPSTF recommends against vitamin E supplements and ß-carotene for the prevention of cardiovascular disease [90].
Adherence to guidelines for management of CHD risk and to prevent cardiovascular disease has been suboptimal, especially among patients at low risk for disease [35,95,96]. Clinicians have noted several barriers to adhering to CHD prevention guidelines, including [35,95]:
Cost of medications
Lack of reimbursement, especially for lifestyle interventions
Lack of adequate time for counseling
Lack of patient education tools
Existence of multiple guidelines
Lack of knowledge and skills to recommend dietary changes and facilitate patient adherence
Efforts should be directed at alleviating these barriers to enable healthcare professionals to evaluate patients' risk factors adequately and to develop ways to help patients understand their risk and the importance of prevention strategies. A multidisciplinary team approach is needed to provide expertise in all areas. In addition, initiatives should emphasize the risk of CHD among women.
Patient I walked into the triage area of the local emergency department. He stated that his primary care physician instructed him to come to the emergency department because his angina attacks were "getting worse." He stated that his physician instructed him to come in an ambulance, but he drove himself. The triage nurse noted that the patient was diaphoretic and in distress. When asked, the patient admitted that he was currently experiencing "some discomfort" in his chest that started when he walked into the hospital from the remote parking area. An ECG showed characteristic ST-segment elevation indicative of an anterior wall MI.
Patient Q was admitted to outpatient surgery for an elective procedure. Her preoperative work-up the day prior to admission showed normal laboratory values and ECG. Her admitting vital signs on the day of surgery were within normal limits. While Patient Q was in the preoperative holding area, she told the nurse that she was experiencing "some weirdness" in her chest. With questioning, she described the sensation as burning and the location as "my chest; no, I can't point to one place, but it hurts a lot." The nurse noted that Patient Q looked anxious and in distress; her respiratory rate increased to 24 breaths per minute, her blood pressure rose to 180/94 mm Hg, and her telemetry monitor showed that she was having isolated premature ventricular contractions (PVCs). Patient Q's initial ECG was negative for indications of ischemia, but her initial set of cardiac biomarkers came back positive for myocardial damage.
Patient J, a man 82 years of age, was admitted to an inpatient medical-surgical unit with a diagnosis of community-acquired pneumonia. He was treated with antibiotics and nebulizer treatments, but he developed a productive cough and complained intermittently about pain in his ribs from coughing. Three or four days after admission, Patient J told the nurse, "I think my pneumonia is getting worse. I have this terrible pain in my chest, and I'm not coughing anything up." When asked, Patient J described the pain as severe discomfort located on the left side of his chest. A check of vital signs showed that Patient J's heart rate was 110 beats per minute and his oxygen saturation on room air was 88%. He was diaphoretic but denied nausea. "I'm just tired, really tired," he reported. "I haven't felt this bad before. I thought I was getting better." An initial 12-lead ECG showed changes suspicious for myocardial ischemia.
When a patient complains of symptoms suspicious for ACS, ACCF/AHA guidelines recommend [2,3]:
Early risk stratification (for risk of death or re-infarct) should be done for any person who presents with chest discomfort or other ischemic symptoms.
Risk stratification includes patient history, assessment of chest pain, physical findings, ECG findings, and cardiac biomarkers.
Use of EMS transport is associated with substantial decreases in ischemia time and in treatment delays [97]. Unfortunately, studies have shown that 40% to 80% of patients with ACS symptoms do not use emergency medical services, with high rates of self-transport among minority populations [97,98,99]. If a person is not at a healthcare facility when he or she develops signs of ACS, the following actions should be taken:
911 should be called to transport the patient to the hospital via emergency medical services. Friends or family should not drive the patient to the hospital.
Persons out of the hospital setting who develop symptoms of ACS and who already have a prescription for sublingual nitroglycerin should take no more than 1 dose of nitroglycerin. If chest pain is not relieved within 5 minutes, the person should call emergency medical services before taking any more nitroglycerin.
During transport to the hospital, emergency medical services should give the patient 162–325 mg of aspirin (chewed or crushed, not swallowed whole).
When a patient presents with clinical signs suspicious for MI, immediate medical intervention is directed at confirming a diagnosis and stratifying the person's risk for adverse events such as cardiac arrest and severe/significant damage to the myocardium [3]. It is imperative to quickly identify patients with chest pain and other symptoms suggestive of ACS, and registration staff and triage nurses should be familiar with their institution's chest pain protocol. High priority should be given to patients with chest pain. Ideally, the emergency department will be notified that a patient with chest pain is arriving, as such patients should be transported by EMS.
The two primary goals of the initial evaluation in the emergency department are to determine the likelihood that an individual has ACS and to estimate the short-term risk of adverse outcome(s) [3]. The findings of the history, physical examination, ECG, and cardiac troponin levels have been integrated into risk assessment scores and clinical prediction algorithms to help identify patients at increased risk of adverse outcomes. Identifying patients at high risk is most important, as these patients will gain the greatest absolute benefit from appropriate therapy [2,3]. Because timely, appropriate treatment depends on results of the clinical findings and diagnostic testing, it is essential that this information is obtained as quickly as possible.
Although a large percentage of individuals with suspected ACS will be seen initially in emergency departments, patients in any healthcare setting, regardless of other diagnoses, may abruptly develop chest pain suspicious for ACS.
Consider these simulated clinical situations:
Patient I walked into the triage area of the local emergency department. He stated that his primary care physician instructed him to come to the emergency department because his angina attacks were "getting worse." He stated that his physician instructed him to come in an ambulance, but he drove himself. The triage nurse noted that the patient was diaphoretic and in distress. When asked, the patient admitted that he was currently experiencing "some discomfort" in his chest that started when he walked into the hospital from the remote parking area. An ECG showed characteristic ST-segment elevation indicative of an anterior wall MI.
Patient Q was admitted to outpatient surgery for an elective procedure. Her preoperative work-up the day prior to admission showed normal laboratory values and ECG. Her admitting vital signs on the day of surgery were within normal limits. While Patient Q was in the preoperative holding area, she told the nurse that she was experiencing "some weirdness" in her chest. With questioning, she described the sensation as burning and the location as "my chest; no, I can't point to one place, but it hurts a lot." The nurse noted that Patient Q looked anxious and in distress; her respiratory rate increased to 24 breaths per minute, her blood pressure rose to 180/94 mm Hg, and her telemetry monitor showed that she was having isolated premature ventricular contractions (PVCs). Patient Q's initial ECG was negative for indications of ischemia, but her initial set of cardiac biomarkers came back positive for myocardial damage.
Patient J, a man 82 years of age, was admitted to an inpatient medical-surgical unit with a diagnosis of community-acquired pneumonia. He was treated with antibiotics and nebulizer treatments, but he developed a productive cough and complained intermittently about pain in his ribs from coughing. Three or four days after admission, Patient J told the nurse, "I think my pneumonia is getting worse. I have this terrible pain in my chest, and I'm not coughing anything up." When asked, Patient J described the pain as severe discomfort located on the left side of his chest. A check of vital signs showed that Patient J's heart rate was 110 beats per minute and his oxygen saturation on room air was 88%. He was diaphoretic but denied nausea. "I'm just tired, really tired," he reported. "I haven't felt this bad before. I thought I was getting better." An initial 12-lead ECG showed changes suspicious for myocardial ischemia.
When a patient complains of symptoms suspicious for ACS, ACCF/AHA guidelines recommend [2,3]:
Early risk stratification (for risk of death or re-infarct) should be done for any person who presents with chest discomfort or other ischemic symptoms.
Risk stratification includes patient history, assessment of chest pain, physical findings, ECG findings, and cardiac biomarkers.
The integration of the clinical presentation and history with ECG findings, cardiac biomarker levels, and results of cardiac imaging is essential for determining an accurate diagnosis, assessing risk, and guiding subsequent therapy. A carefully taken patient history is essential to elicit the details needed to make an accurate diagnosis. The medical history should focus not only on the type of pain the individual is having but also on risk factors that may predispose the patient to ACS. Information to obtain includes [2,3,34,100]:
Time symptoms began
Identification of contraindications to potential treatment measures
Medications the patient is currently taking
Allergies
Risk factors for CHD
History of previous admissions for chest pain or ACS
Past history of intervention for CHD/ACS, including PCI and coronary artery bypass graft (CABG) surgery
Known cerebral vascular or peripheral vascular disease
Research has shown that a history of traditional cardiac risk factors varies among some subgroups. Women with ACS are more likely than men to have a history of diabetes, hypertension, or hyperlipidemia [11,101,102,103,104,105,106]. (It has been suggested that this is due to the fact that women tend to develop ACS at an older age) [103,106]. Women are less likely to be smokers, to have a history of angina or MI, and to have had PCI or CABG, regardless of the cardiac history [104,107,108]. Data on the prevalence of risk factors across racial/ethnic subgroups with ACS was reported in 2008 (Table 6) [109].
RISK FACTORS FOR CHD ACCORDING TO RACE/ETHNICITY AMONG PATIENTS WITH ACS
| Patient Characteristics | White | Black | Hispanic | Native American | Asian |
|---|---|---|---|---|---|
| Age | 63.9 years ±13 | 59.4 years ±13 | 61.3 years ±13 | 58.7 years ±12 | 63.7 years ±12 |
| Male gender | 62% | 50% | 61% | 62% | 61% |
| Risk Factors | |||||
| Family history of CHD | 42% | 38% | 37% | 42% | 28% |
| Hypertension | 69% | 81% | 71% | 70% | 75% |
| Diabetes | 28% | 40% | 44% | 54% | 37% |
| Current smoker | 26% | 31% | 22% | 38% | 16% |
| ACS = acute coronary syndrome; CHD = coronary heart disease. | |||||
The five most important history-related factors that relate to the likelihood of ischemia due to CHD are (in order of importance) [110]:
Nature of the chest pain
History of CHD
Sex/gender
Age
Number of traditional risk factors
Among patients who have no pre-existing CHD, older age seems to be the most important factor related to a diagnosis of ACS. An age of older than 55 years for men or older than 65 years for women has been shown to be more important than all other factors [111,112,113].
Most often, the physical examination is normal for patients being evaluated for possible ACS. Thus, for these patients the physical examination is important not to establish a diagnosis of ACS but rather to rule out an alternate diagnosis, identify any comorbidities that may have an impact on treatment decisions, and add prognostic information [2,3]. Ruling out a noncardiac cause of chest pain is especially important given the severity of other possible causes of chest pain [3,114].
The physical examination should include [3]:
Evaluation of vital signs
Determination of the presence of stroke, pulses, and jugular venous distention
Pulmonary auscultation for rales
Cardiac auscultation for murmurs and gallops
Neurologic evaluation
Evaluation for signs of cardiogenic shock (hypotension and organ hypoperfusion)
Identification of contraindications to antiplatelet or fibrinolytic therapy
The presence of bruits or pulse deficits (which would suggest extracardiac vascular disease) is associated with a higher likelihood of significant CHD [3]. Similarly, significant CHD is more likely in a patient who has an S3 or S4 gallop, a new mitral insufficiency murmur, or signs of congestive heart failure (pulmonary rales and elevated jugular venous pressures) [115]. Cardiogenic shock is associated more often with STEMI than NSTEMI, and mortality rates are high [3]. Contraindications to antiplatelet or fibrinolytic therapy include any prior intracranial hemorrhage, known malignant intracranial neoplasm, suspected aortic dissection, active bleeding or bleeding diathesis (excluding menses), or significant closed-head or facial trauma within the previous three months [2].
Chest pain is the most commonly reported symptom in all patients with ACS, regardless of age, gender, race/ethnicity, or the presence of comorbid conditions [14,116,117]. So-called "classic" ACS-related chest pain has been described as diffuse pain or pressure in the substernal or epigastric area that frequently radiates to the neck, jaw, and left arm [22,101,118,119]. Chest pain related to ACS usually begins abruptly and lasts at least 15 to 20 minutes; however, the duration of pain varies among patients [101,120]. Pain that lasts for longer than 20 minutes is associated with increased short-term risk of MI (nonfatal or fatal) [121]. The intensity of "classic" ACS chest pain increases over time, reaching maximal intensity after a few minutes [101,122]. Pain is usually worse with activity and improves with rest [101].
The first step in evaluating chest pain is to determine whether the pain is cardiac or noncardiac. Many other conditions can cause chest pain that is similar to cardiac pain, and the physical examination and imaging tests can aid in the differential diagnosis. Chest pain assessment should include time of onset of the pain, description of the pain or discomfort, location of the pain, intensity/severity of the pain, radiation to any other body part, any associated symptoms, how long the pain lasts, and what relieves the pain (Table 7) [3,114].
When medications such as nitroglycerin or morphine are administered, their effectiveness in reducing or relieving chest pain should be noted. In the past, it was thought that cardiac pain could be distinguished from some types of noncardiac pain by assessing the relief of chest pain with use of specific drugs, such as nitroglycerin or antacids. However, relief of chest pain after administration of either of these drugs should not be used to distinguish pain as cardiac or noncardiac in nature. Studies have shown that nitroglycerin may relieve both cardiac and noncardiac chest pain [3]. In one study, nitroglycerin relieved chest pain in 35% of patients with ACS and 41% of patients without ACS [3]. Similarly, a gastrointestinal cause of pain should not be assumed if the chest pain is relieved by antacids, as some patients with ACS have reported relief after use of such a drug [3,123].
Typical ACS Symptoms
Typical or classic ACS-related chest pain is often described as tightness, sensation of pressure, heaviness, crushing, vise-like, aching, and/or squeezing [101,124]. Pain features that are not generally characteristic of ACS-related pain include sharp, stabbing pain; pain reproduced with movement or palpation of the chest wall or arms; pain lasting several hours; fleeting pain (episodes lasting for a few seconds or less); burning pain or heartburn; knot in the chest; lump in the throat; or band-like sensation [3,101,115,122,123]. The classic presentation of ACS includes some symptoms in addition to chest pain, primarily dyspnea, diaphoresis, nausea, or syncope [14,22,125,126]. Again, there is wide variation in the symptoms reported by patients with ACS, as well as differences in subgroups of patients. Patients with STEMI more commonly report nausea, cold sweats, and vomiting [127]. Several studies have demonstrated an increased prevalence of diaphoresis among men with ACS compared with women [107,116,128,129,130,131].
An important distinction between stable angina and UA is that the former is exacerbated by activity or emotional stress and relieved by rest and/or nitroglycerin; in contrast, UA occurs at rest [3]. Pain associated with UA may also be pain previously diagnosed as angina that has increased in frequency, duration, or severity or that is prompted by less exertion than in the past [3].
Atypical ACS Symptoms
An increasing number of studies have demonstrated that atypical chest pain occurs more often in several subgroups of patients, especially women, older individuals, and people with diabetes [14,102,117,126,131,132,133,134]. In addition, the findings of several studies and literature reviews have demonstrated that women with ACS are more likely to have pain or discomfort in the jaw, neck, throat, arm/shoulder, and back [102,127,131]. Failure to recognize atypical symptoms of ACS has been found to delay diagnosis and/or result in the use of less aggressive treatment. It has been estimated that more than 40% of patients with angina have one or more "atypical" elements in their chest pain description [135,136]. Atypical symptoms that have been found to be associated with ACS include shortness of breath, fatigue, lethargy, indigestion, anxiety, tingling in upper extremities, palpitations, loss of appetite, and flushing. Words commonly used to describe "atypical" chest pain associated with ACS include numbness, tingling, burning, stabbing, or pricking. Atypical chest pain location includes any area other than substernal or left sided, such as the back, area between shoulder blades, upper abdomen, shoulders, elbows, axillae, and ears [135,136].
Clinical presentation may also differ for older patients. Research has shown that the absence of chest pain is more likely in older patients compared with younger patients. According to study data, 40% of ACS patients 85 years of age or older had chest pain compared with 77% of ACS patients younger than 65 years of age [14]. Older patients with ACS have also been less likely to report arm pain [129].
Few studies have been done to compare reports of chest pain across racial/ethnic groups or according to comorbid conditions. However, studies have demonstrated chest pain of greater intensity and over a greater area in Asian patients (compared with non-Asian patients) and more frequent atypical chest pain (described as stabbing, numbness, or burning) among patients with ACS and diabetes (compared with no diabetes) [110,111].
Despite this fact, up to one-third of patients with ACS have no chest pain or discomfort [117,137]. This so-called "silent ischemia" is more likely to occur in persons with diabetes, women, older adults, and persons with heart failure [1,34]. Thus, the lack of chest pain should not rule out ACS as a diagnosis, especially in the presence of other indicators.
Electrocardiography has historically been used to assess myocardial ischemia, and it continues to be an essential diagnostic tool [138]. A 12-lead ECG can be used to [1,33,34,47]:
Confirm the diagnosis of acute STEMI
Differentiate between UA/NSTEMI and STEMI
Identify the affected part of the myocardium
Diagnose arrhythmias and conduction abnormalities that may occur during ischemia and infarct
To understand how 12-lead ECGs can provide information about myocardial ischemia, injury, or infarct, an understanding of the basic electrocardiography principles is necessary. A thorough discussion of 12-lead ECG interpretation in the diagnosis, evaluation, and management of MI exceeds the scope of this course; the information presented below is intended as an introduction and overview only.
The standard 12-lead ECG is a representation of the heart's electrical activity recorded from electrodes on the body surface. In a traditional 12-lead ECG, 10 recording electrodes are placed in designated positions on the patient's arms, left leg, and the left side of the chest. Twelve different recordings of the patient's heart rhythm are taken simultaneously; each records the electrical signals from the heart using a particular combination of the recording electrodes. Each combination of electrodes is referred to as a "lead." Each lead is given a designation that reflects its location and its view of the heart [47].
Some leads look at the bottom (inferior) section of the heart, others monitor what occurs in the anterior wall, and still others monitor the lateral wall. Because of the way the heart is positioned in the thorax, none of the surface leads in a standard ECG directly look at the back of the heart. However, the placement of some leads can be modified to provide more direct information [47].
In normal conduction, the ST segment begins at the end of the QRS complex and stops at the beginning of the T wave. In the cardiac cycle, this segment corresponds to mechanical systole. On ECG, the ST segment normally appears flat and lies along the baseline.
The T wave represents the period of ventricular repolarization. In appearance, the T wave looks asymmetrically rounded. Normally, the T wave is upright in leads I, II, and V [47]. Changes in the ST segment and the T wave can indicate the presence of acute myocardial ischemia and acute MI. The ECG leads in which these changes occur provide information about the part of the heart involved.
The ACC/AHA guidelines recommend that a 12-lead ECG be done and interpreted by an experienced physician within 10 minutes after arrival for patients who have chest pain or other signs suggestive of ACS [2,3]. The diagnostic accuracy of ECG is improved if it is done while the patient is symptomatic, as acute ischemia (and underlying CHD) is strongly suggested by the transient ST-segment changes that occur during symptoms at rest and resolve when symptoms disappear [3]. A 12-lead ECG performed by EMS personnel is recommended for patients who have symptoms consistent with STEMI [2].
A single ECG cannot capture the entire dynamic process of ischemia. As a result, the initial ECG for patients with acute MI can be normal or nondiagnostic in 20% to 55% of cases [82]. Among patients with chest pain and a normal ECG, approximately 1% to 6% will subsequently be found to have MI and about 4% will be found to have UA [3]. Nondiagnostic ECGs are more likely in older patients; according to trial data, the rate of nondiagnostic ECGs was 23% for patients younger than 65 years of age and was 43% for patients 85 years of age and older [14]. In addition, ST-segment elevation on the ECG at presentation has been shown to decrease with age, from 96.3% for patients younger than 65 years of age to 69.9% for patients 85 years of age or older [14]. Thus, the ACC/AHA guidelines state that if the initial ECG is not diagnostic or if the patient remains symptomatic and ACS is suspected, serial ECGs should be done at intervals of 15 to 30 minutes during the first hour [3].
Adherence to the ACC/AHA guidelines for obtaining ECG has been suboptimal, with ECG being performed up to 73% of the time [139,140]. Delay in obtaining the first ECG has been associated with female gender and older age [14,141,142]. This delay may be related to the high rate of atypical presentation of ACS in these populations [14,143]. Increasing the number of nurses or ECG technicians during peak hours and training additional staff to perform ECGs may help to improve timeliness [144,145].
Three classic ECG characteristics are used in the diagnosis of STEMI: ST-segment elevation, T-wave inversion, and Q-wave formation. During MI, these ECG changes can evolve over minutes to hours. They reflect the impact of the infarction on the functioning of affected myocardial tissue. In STEMI, the damage generally involves the full width of the myocardial wall (from the inner endocardium through the upper epicardium); the term "transmural" is used to designate this type of full-wall thickness damage. The associated ECG changes in STEMI mirror the spread of the damage as it begins in the endocardium and travels outward through the heart wall until the epicardium of the wall is also damaged [1,34,47].
The earliest ECG hint of an acute STEMI is an increase in the height of the T wave. Referred to as "hyperacute," these T-wave changes are transient. They are not considered a definitive diagnostic sign but should be taken as highly suspicious for possible acute MI in a patient with clinical symptoms of ACS [1,34,47].
The first of the three classic signs is ST-segment elevation. It may be followed by T-wave inversion and pathologic Q-wave formation. This sequence of changes is called the electrocardiographic evolution of an infarction. Because these changes happen over a period of time, a series of 12-lead ECG tracings may be required for accurate diagnosis. In the very early stages of infarct, clear patterns may not be immediately revealed on ECG. As always, ECG findings should be correlated with clinical signs and symptoms. Over a period of months to days, ST-segment elevation and T-wave changes will resolve and no longer be present on 12-lead ECG recordings. Pathologic Q waves, on the other hand, frequently remain permanently. Presence of a pathologic Q wave on 12-lead ECG with no evidence of ST-segment elevation or T-wave changes usually indicates that the person has had an infarct in the past [1,34,47]. It is important to note that ST-segment and T-wave changes are not specific for ACS and may be the result of another disease or condition. Left ventricular aneurysm, pericarditis, myocarditis, Prinzmetal angina, Takotsubo cardiomyopathy, early repolarization, and Wolff-Parkinson-White syndrome may cause ST-segment elevation [3]. T-wave inversion can be caused by central nervous system events and treatment with tricyclic antidepressants or phenothiazines.
The ST segment in a normal ECG complex runs along the baseline of ECG. In STEMI, the ST segment lifts upward off the baseline on the ECG tracing, reflecting the movement of injury in the myocardium. ST-segment elevation will be noted in the ECG leads that are facing the affected area of the heart wall. These changes are referred to as changes indicative of infarct. To confirm a diagnosis of STEMI, characteristic ECG changes must be present in two adjacent (contiguous) leads [1,34,47,146].
As an acute MI continues to evolve, the elevated ST-segment will begin to drop. As it drops, the T wave begins to come down to baseline and eventually inverts. When a 12-lead ECG shows evidence of the ST-segment elevation resolving and the T wave inverting, it indicates that the infarction is well along in evolution [47].
When an infarct damages the full thickness of the affected wall, the myocardial tissue loses its ability to depolarize and conduct electrical impulses. The tissue becomes electrically inert and generates no electrical activity. When a 12-lead ECG is performed, the area of infarction acts like a "window" that allows ECG monitoring leads to look through the infarct to the opposite wall of the heart. This results in characteristic changes in the recorded ECG pattern. One of these changes is referred to as a pathologic Q wave. Pathologic Q waves are seen in the leads that reflect the infarction. In a normal ECG recording, a Q wave may be present as the first negative deflection of the QRS complex. However, when the Q wave is significantly over-sized, it reflects a change in depolarization due to the presence of necrotic tissue. Although a pathologic Q wave can be seen in either STEMI or NTSEMI, it is more common in STEMI. Unlike ST-segment elevation and T-wave inversion, formation of a pathologic Q wave is permanent [34,47].
It is possible for an acute infarction to occur that causes ST-segment elevation but does not extend damage through the full thickness of the myocardial wall. This type of infarction is sometimes referred to as a subendocardial infarction. It will cause ST-segment changes (elevation initially, then resolving) and T-wave inversion but will not have a Q wave during the acute episode or afterwards. The diagnosis of non-Q wave MI is based on ST-wave changes and T-wave changes. The leads in which the classic signs of STEMI are seen give an indication of what vessel and what wall of the heart are involved (Table 8).
ECG CHANGES AND DIAGNOSIS OF STEMI
| Leads Showing Changes | Location of Infarction | Location of Occlusion |
|---|---|---|
| II, III, aVF | Inferior wall | Right coronary artery |
| I, aVL, V5–6 | Lateral wall | Circumflex artery |
| V1–V4 | Anterior wall | Left anterior descending |
| Reciprocal changes only in V1–V2, sometimes V4 | Suspect posterior wall of the heart | Right coronary artery |
| ST elevation in inferior leads and lead V1 | Suspect right ventricular wall | Right coronary artery |
Identification of right ventricular acute MI can be difficult because standard ECG lead placement does not provide a good direct view of the right ventricle. If a right ventricular acute MI is suspected, a modified 12-lead ECG may be done in which V leads are placed on the right side of the chest (instead of the left) in corresponding positions. An "R" is added to the lead designation to indicate the change in position [1,34,47].
True posterior acute MI may be caused by damage to the posterior wall of the left ventricle. The traditional 12-lead ECG may also be modified to provide additional diagnostic information through use of additional leads (V7–V9) positioned at set points on the patient's back [1,34,47].
An NSTEMI may be characterized by ST-segment depression and T-wave abnormalities. ST-segment elevation does not occur [47]. Both UA and NSTEMI are characterized by a lack of ST-segment elevation on ECG, so the distinction between the two conditions relies on troponin levels.
During myocardial ischemia, blood flow to the endocardium is reduced first; blood flow to the outer layer of heart (epicardium) remains adequate. As a result, the endocardium experiences significant metabolic changes associated with ischemia while the epicardium does not. These changes alter the electrical potential and current flow through the myocardium. A 12-lead ECG records these changes as ST-segment depression. Measured from the isoelectric line, an ST depression of 1 mm or more below baseline can indicate ischemia. It is important to note, however, that when ST-segment depression is seen in some leads along with ST-segment elevation in other leads, the ST-depression is a reciprocal ECG change associated with STEMI. As always, it is important to place ECG findings within the full context of the patient's symptoms. Because it reflects the changing balance of oxygen supply and demand in the affected coronary artery, ST-segment depression may be present during the period of ischemia only to disappear when the ischemia is relieved. Ischemia can also cause T-wave abnormalities such as T-wave inversion. In NSTEMI, these changes can be difficult to interpret [47].
Imaging studies are an important component of evaluation of patients with chest pain.
Chest x-ray is used primarily to rule out other causes of chest pain, such as pulmonary embolus, aortic dissection, and cardiomyopathy [22,122,125]. Radiography findings are rarely abnormal in patients with ACS [148].
In the ACCF/AHA/American Society of Echocardiography guidelines, echocardiography is a class I recommendation for patients with chest pain and suspected ACS when the baseline ECG and biomarkers are nondiagnostic [149,150]. The guidelines suggest that the test be done while the patient is having pain or within minutes after pain has subsided. The strengths of echocardiography are its ability to assess myocardial thickness, thickening, and motion at rest, and it can aid in risk stratification of patients with suspected UA/NSTEMI [22,125]. Transient segmental wall motion abnormalities that normalize with treatment support a diagnosis of UA [149,150]. Persistent wall motion abnormalities indicate more severe, chronic ischemia and a higher risk of adverse events [151]. Echocardiography is also useful for assessing left ventricular function before angiography [151]. The ACCF/AHA guidelines for STEMI note that it is reasonable to use portable echocardiography to clarify a diagnosis of STEMI and to aid in risk stratification [2]. The disadvantages of echocardiography are its inability to distinguish between acute and chronic abnormalities and the need for skilled technicians and interpreters of results [122].
Cardiac MRI has been validated for assessing myocardial function and has a similar capability to echocardiography in the diagnosis of MI [122,152]. The usefulness of MRI in this setting was studied in 161 consecutive patients who had 30 minutes of chest pain and ECG findings that were nondiagnostic of acute MI. MRI that included perfusion, left ventricular function, and gadolinium-enhanced MI detection was shown to have a sensitivity and specificity of 84% and 85%, respectively, for diagnosing ACS [153]. MRI is not generally used in the acute setting because of the inconvenience of its use [22,125].
Factors to consider when selecting a stress test are the patient's resting ECG and ability to exercise, as well as local resources. An exercise stress test is the easiest, most cost-effective test and should be the choice unless the patient is unable to exercise or has ST changes on resting ECG (class IC) [3]. ST changes on the resting ECG may interfere with interpretation of the stress test findings, and for patients with ST changes, stress testing with an imaging modality (such as cardiac radionuclide imaging or stress echocardiography) is recommended (class IB). Pharmacologic stress testing with imaging should be done for patients who have limited ability to exercise (class IC). Exercise stress testing should be done and interpreted according to the ACC/AHA guidelines, and the results will dictate the need for further therapy [154].
Used to evaluate the effects of stress on the heart muscle and coronary blood flow, an exercise stress test involves some type of physical exercise. Walking on a treadmill is a common method. Following a predetermined protocol, the speed of the treadmill and its angle are increased at set intervals. The patient's ECG and blood pressure are monitored. The test is terminated when a target heart rate is achieved or the patient develops symptoms such as chest pain, hypotension, bradycardia, severe hypertension, or ST-segment changes on ECG. Because patients must be physically able to walk on the treadmill, this test is contraindicated for anyone who cannot do so. Chemical stress tests may be used instead. Consumption of caffeine or cigarette smoking is contraindicated for several hours prior to the test. Patients should be instructed to wear comfortable clothes and shoes appropriate for walking on a treadmill; female patients should be directed to wear a bra that provides adequate support. Echocardiogram imaging may be added to an exercise stress test to provide information about the presence or absence of heart wall abnormalities. If echocardiography is included, a baseline test will be performed prior to the exercise part of the test. Immediately following the conclusion of the treadmill portion, the echocardiogram will be repeated [34,147,155].
Diagnostic findings from an exercise stress test include [34,147,155]:
Negative: The patient achieves the target heart rate with no symptoms of ischemia. No evidence of new heart wall motion abnormalities are noted on echocardiogram.
Positive: The patient develops symptoms of ischemia during the test. New heart wall motion abnormalities are evident in the echocardiogram completed after the treadmill portion of the test. Follow-up testing, usually cardiac catheterization, is indicated.
Equivocal: The patient develops symptoms during the test that are not directly linked to myocardial ischemia, or the patient is unable to achieve the target heart rate but has no symptoms of ischemia. Additional testing is indicated.
Combining a chemical stress test with radionuclide imaging, an adenosine thallium test evaluates the blood supply to the myocardium. This test may be performed in two parts. The patient is kept NPO for 4 to 6 hours prior to the start of the test. Adenosine is injected to increase heart rate, myocardial contractility, and myocardial oxygen demand. Radioactive thallium is injected, and a series of images are taken to assess the adequacy of blood flow to the myocardium. Several hours later, the patient is again scanned to evaluate blood flow to the myocardium at rest. Adenosine thallium scans may identify site(s) of old infarctions, areas of partial obstruction of blood flow to the myocardium, and areas where blood flow (perfusion) decreases during exercise [34,147,155]. In 2013, the FDA issued a warning of a rare but serious risk of myocardial infarction and death associated with adenosine [156]. Adenosine should be avoided in patients with evidence of unstable angina or cardiovascular instability.
A DSE test may be used to evaluate the heart's response to stress in patients who are unable to physically perform a treadmill exercise test. This test uses IV dobutamine to "stress" the heart by increasing myocardial contractility and heart rate, which in turn increases myocardial oxygen demands. Echocardiogram imaging is done when the patient is at rest and after the dobutamine has been injected to look for wall motion abnormalities [34,147,155].
Results may be:
Negative: The patient's heart rate reaches the target rate, and the patient shows no symptoms of ischemia. Echocardiogram imaging shows no new heart wall motion abnormalities.
Positive: The patient develops symptoms before reaching the target heart rate and/or new heart wall motion abnormalities are seen on Echocardiogram. Follow-up testing, usually a cardiac catheterization, is indicated.
Cardiac biomarkers are detectable intracellular macromolecules released into the circulation after cardiomyocyte injury and death. The biomarkers once used—creatinine kinase (CK)-MB and myoglobin—have been replaced by cardiac-specific troponin (troponin I or T) because of the latter's high concentration in myocardium, near-absolute specificity for myocardial tissue, their absence in the blood of healthy individuals, and their high clinical sensitivity [2,3,22]. Measurement of CK-MB or myoglobin levels was not useful or cost-effective [157].
As noted, cardiac troponin I and T are sensitive and specific biomarkers of myocardial injury, and serum measurements are used to identify whether patients with ACS have had an MI. A variety of troponin assays are in use. Contemporary ("sensitive") troponin assays have been in use for many years, while "highly sensitive" assays were only approved in 2017 for use in the United States. The Fourth Universal Definition of MI recommends using highly sensitive troponin assays when available [22].
The time to initial elevation of cardiac troponin levels following MI is 2 to 12 hours when measured by sensitive assays, with peak elevation at 24 hours (troponin I) and 12 to 48 hours (troponin T) [3,158]. Levels may remain elevated for 5 to 10 days (troponin I) or up to 14 days (troponin T) after an MI [158]. Highly sensitive assays detect significant elevations of cardiac troponin within one hour, which has the advantage of more rapid diagnosis and triage. The sensitivity of cardiac troponin for the diagnosis of MI is relatively low during the first six hours, especially in patients who present shortly after symptom onset [158]. However, for most patients with ACS, MI can be ruled out or confirmed within six hours, in part because of the high rate of delayed presentation associated with chest pain [3].
For the diagnosis of MI, the fourth universal definition of MI defines myocardial injury as a rise and/or fall in cardiac troponin of at least one value above the 99th percentile of the URL for normal values, including evidence of serial increases or decreases of troponin levels [22]. Similarly, the recommendations based on the findings of a Laboratory Medicine Best Practices systematic review are the use of cardiac troponin assays only (no additional biomarkers), with the 99th percentile URL used as the clinical diagnostic threshold for a diagnosis of NSTEMI [159].
It is important to bear in mind that chronic elevations of troponin are present in some patients unrelated to acute events, which is why a rise or fall of troponin is required to establish the diagnosis of MI. Baseline troponin levels are often higher in the elderly than in younger adults; 20% of adults older than 70 years of age have, as baseline, a cardiac troponin level above the 99th percentile URL [160]. Troponin assays are not standardized; the value reported will vary depending on the assay used, and comparison of reported results across different laboratories may not be reliable for diagnostic purposes [22]. Clinicians should familiarize themselves with the specific assay used in their own facility.
The ACC/AHA guideline for UA/NSTEMI states that troponin levels should be measured at the time of presentation and three to six hours after the onset of symptoms in all patients suspected of having ACS [3]. If the time of symptom onset is unclear, the time of presentation should be used instead. When initial serial troponin levels are normal but ECG changes and/or clinical features increase the suspicion for ACS, additional troponin levels should be measured beyond six hours [3]. The lack of elevated troponin levels at the time of presentation should not rule out an MI, as the initial level is normal in as many as 23% of patients with MI [161]. The lack of elevated troponin levels at the time of presentation should not rule out an MI, as the initial level is normal in as many as 23% of patients with MI [161]. Troponin levels appear to have value in ruling out an MI; the negative predictive value of undetectable troponin levels has been reported to be 99% to 100%.
A diagnosis of MI should not be made on the basis of a single elevated troponin level, as elevated levels may be associated with other cardiac conditions, including tachyarrhythmia, high or low blood pressure, cardiac trauma, heart failure, myocarditis, and pericarditis [3].
As noted earlier, CK-MB, myoglobin, and other biomarkers are no longer useful in diagnosing ACS. B-type natriuretic peptide (BNP) and N-terminal proBNP are also not useful as an aid to diagnosing ACS, but they have demonstrated strong predictive value for short- and long-term mortality for patients with ACS, and the ACC/AHA guideline notes that these biomarkers may be considered to assess risk in patients in whom ACS is suspected (class IIbB) [3,162,163].
Risk stratification is an integral component of diagnosis, especially for patients with UA/NSTEMI. The risk of cardiac death and ischemic events varies widely in the UA/NSTEMI population, and the prognosis can help inform decision making regarding treatment [2]. The ACC/AHA guidelines for UA/NSTEMI and STEMI recommend risk assessment with either the Thrombolysis in Myocardial Infarction (TIMI) risk score or the GRACE risk model [2,3]. The TIMI risk score predicts 30-day and one-year mortality and was developed in a population of patients with STEMI; the GRACE model predicts in-hospital and six-month mortality for all patients with ACS [2,3].
The TIMI risk score is based on seven independent risk factors [164]:
Advanced age (65 years or older)
At least three risk factors for CHD
Previous coronary artery stenosis of 50% or more
ST-segment deviation on initial ECG
At least two episodes of angina in the past 24 hours
Use of aspirin in the past 7 days
Elevated levels of cardiac biomarkers
One point is given for each factor, and the total score corresponds to the risk of all-cause mortality, new or recurrent MI, or severe recurrent ischemia requiring urgent revascularization through 14 days [164]. That risk ranges from 4.7% for a TIMI risk score of 0 or 1 to 40.9% for a score of 6 or 7. Patients with a higher TIMI score will derive greater benefit from an invasive strategy [3]. The TIMI risk calculator can be accessed online at http://www.timi.org.
The GRACE risk model includes eight variables [165]:
Age
Killip class
Systolic blood pressure
ST-segment deviation
Cardiac arrest during presentation
Serum creatinine level
Elevated cardiac biomarkers
Heart rate
Points are assigned to each factor, and the sum total corresponds to a probability of in-hospital death, ranging from 0.2% or less for up to 60 points to more than 52% for a sum of 250 points or more [165]. As with the TIMI score, patients with a higher score gain greater benefit from an invasive strategy [3]. The GRACE risk tool is also available online (https://www.outcomes-umassmed.org/grace).
Clinical features, ECG findings, and troponin levels also may be used to determine both early- and long-term prognosis and direct treatment. For example, patients with elevated troponin levels will benefit from intensive management and early revascularization [3]. In addition, elevated troponin levels have been associated with an estimation of infarct size and the risk of death [3]. With regard to ECG findings, after confounding ECG patterns (i.e., bundle-branch block, paced rhythm, left ventricular hypertrophy), the highest risk for death has been associated with ST-segment deviation (elevation or depression) [3]. Isolated T-wave inversion or normal ECG findings were associated with intermediate and low risk, respectively [3]. In another study, the incidence of death or MI at 1 year was significantly higher for patients who had ST-segment deviation of at least 1 mm and an elevated troponin level (18%) compared with patients who had deviation of less than 1 mm (11%) [166].
Four diagnoses are possible after complete evaluation for possible ACS: a noncardiac diagnosis, chronic stable angina, possible ACS, and definite ACS.
Risk assessment factors are used to help identify people who are at low risk of ACS and can thus be discharged safely. In one study, short-term clinically relevant adverse cardiac events were rare among patients who had "nonconcerning" vital signs, nonischemic findings on ECG, and no elevated troponin levels on serial testing [167]. Accelerated diagnostic protocols have been developed to help identify patients who can be safely discharged. According to one such protocol, a TIMI score of 0, no new ECG changes, and nonelevated troponin levels at 0 and 2 hours after the time of presentation indicates a low risk of ACS, with no major adverse cardiac events occurring within 30 days after discharge [168,169]. Another risk stratification tool, the HEART score (consisting of history, ECG findings, age, risk factors, and troponin levels) has been validated in the Netherlands [170]. The HEART score has been shown to identify patients at low risk for ACS and major adverse cardiac events [170]. When compared with care according to ACC/AHA guidelines, a protocol consisting of the HEART score and troponin levels at 0 and 3 hours, led to an increased number of early discharges, with no major adverse cardiac events at 30 days; shorter lengths of stay, and a decrease in objective cardiac testing over 30 days [171].
The ACC/AHA guideline for UA/NSTEMI includes no class I recommendations for discharge from the emergency department. For patients with possible ACS but normal ECG and troponin levels, the guideline notes that it is reasonable to [3]:
Observe in a chest pain unit or telemetry unit and perform serial ECGs and cardiac troponin levels at intervals of three and six hours (class IIaB)
Order a treadmill ECG (class IIaA), stress myocardial perfusion imaging, or stress echocardiography (class IIaB) before discharge or within 72 hours after discharge
Perform coronary CT angiography to assess coronary artery anatomy (class IIaA) or rest myocardial perfusion imaging with a technetium-99m radiopharmaceutical to exclude myocardial ischemia (class IIaB)
Patients with chronic stable angina should be treated according to the ACC/AHA guidelines [172]. Patients who are discharged from the emergency department should be told to see their primary care physician as soon as possible, preferably within 72 hours [3]. The results of all diagnostic testing in the emergency department should be sent to the primary care physician to ensure continuity of care. Patients with definite ACS should be treated according to the type of MI.
According to data from several studies and quality improvement initiatives, adherence to ACC/AHA guidelines has improved since the early 2000s, but is still not optimal. In addition, time is needed for clinicians to become familiar with updates to clinical practice guidelines; the ACC/AHA guideline for UA/NSTEMI was revised in 2014.
The ACC/AHA guideline reflects the research advances made in ACS. Many more treatment options are available, and clinicians should be familiar with the choices in order to select a strategy on the basis of an individual's status and preference. The most substantial changes in the updated 2014 guideline relate to the following issues [3]:
More potent antiplatelet and anticoagulant therapy
Benefit of guideline-directed medical therapy for low-risk patients
Proper selection of older individuals and women for interventional therapy
Expanded recommendations on discharge, including patient education, dual antiplatelet therapy, and referral to cardiac rehabilitation
The general care of patients with UA/NSTEMI is directed at the severity of symptoms. Bed rest is recommended while patients have ischemic pain. After symptoms have subsided, patients may move to a chair. The ACC/AHA guideline notes that there is no benefit to the routine use of supplemental oxygen, and it may, in fact, even be harmful [3]. Instead, supplemental oxygen should be given only to patients who have an arterial oxygen saturation of less than 90%, respiratory distress, or other high-risk features of hypoxemia. Continuous ECG monitoring should also be carried out, not only to detect ECG changes that may provide additional diagnostic and prognostic information but also because sudden ventricular fibrillation is the primary preventable cause of death during this initial period [3].
The goal of immediate treatment for patients with UA/NSTEMI is to provide relief of ischemia and to prevent recurrent adverse ischemic events [3]. This is initially achieved through anti-ischemic, antiplatelet, and anticoagulant therapies (Table 9).
ADJUNCTIVE TREATMENT INDICATIONS FOR PATIENTS WITH UA/NSTEMI OR STEMI
| Adjunctive Therapy | UA/NSTEMI | STEMI | Comments | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Analgesia | |||||||||||
| Nitroglycerin | All patients, unless contraindicated (class IC) | No recommendation | Contraindicated for patients with hypotension or who have used sildenafil or vardenafil within previous 24 hrs or tadalafil within previous 48 hrs (class IIIB). | ||||||||
| All patients, unless contraindicated (class IB) | No recommendation | ||||||||||
| Morphine | Reasonable for patients who have chest pain unrelieved by maximally tolerated anti-ischemic medications (class IIbB) |
| — | ||||||||
| Anti-Ischemia Therapy | |||||||||||
| Beta blocker |
|
|
| ||||||||
| ACE inhibitor | Started and continued in all patients with left ventricular ejection fraction less than 40% and in patients with hypertension, diabetes, or stable CKD, unless contraindicated (class IA) | All patients (within the first 24 hours) with anterior location, HF, or ejection fraction less than or equal to 0.40, unless contraindicated (class IA) |
| ||||||||
| Calcium-channel blocker | Patients with continued or recurrent ischemia or with contraindications to beta blockers (class IB) | No recommendation | — | ||||||||
| Antiplatelet Therapy | |||||||||||
| Aspirin (non-enteric coated, chewable) |
|
|
| ||||||||
| Clopidogrel |
|
| Loading dose not recommended for older (>75 years of age) patients with STEMI. Should be withheld for 5 days in patients to have CABG (class IB). Monitor closely when used in conjunction with warfarin. | ||||||||
| Prasugrel |
|
|
| ||||||||
| Ticagrelor | All patients undergoing PCI with stenting should be given a loading dose and at least 1 year of maintenance therapy with this or other P2Y inhibitor if not given clopidogrel (class IB). | All patients (in addition to aspirin) undergoing PCI with stenting should be given a loading dose and at least 1 year of maintenance therapy with this or other P2Y inhibitor if not given clopidogrel (class IB). |
| ||||||||
| Glycoprotein IIb/IIIa inhibitor | Patients selected for early invasive treatment, along with dual-antiplatelet therapy, who are at intermediate or high risk (high troponin levels) (class IIbB) |
|
| ||||||||
| Anticoagulant Therapy | |||||||||||
| Unfractionated heparin (UFH) |
| Option for patients selected for primary PCI (class IC) or fibrinolytic therapy (class IC); administer for at least 48 hrs or until revascularization | The UFH dose should be reduced when a glycoprotein IIb/IIIa inhibitor is also given (class IC).For patients undergoing PCI after receiving anticoagulant regimen, administer additional boluses of UFH as needed to support procedure (class IC). | ||||||||
| Enoxaparin | Option for patients selected for early invasive treatment (class IA) and early conservative treatment (class IA) | Option for patients selected for fibrinolytic therapy (class IA); administer for at least 48 hours; for use up to 8 days or until revascularization |
| ||||||||
| Bivalirudin | Option for patients selected for early invasive treatment (class IB) |
|
| ||||||||
| Fondaparinux | Option for patients selected for early invasive treatment (class IB) and early conservative treatment (IB) | Option for patients selected for fibrinolytic therapy (class IB) |
| ||||||||
| ACE = angiotensin-converting enzyme; CABG = coronary artery bypass graft; CKD = chronic kidney disease; HF = heart failure; PCI = percutaneous coronary intervention. | |||||||||||
SIZE OF TREATMENT EFFECT FOR RECOMMENDED INTERVENTIONS
| Class | Predicted Treatment Effect | ||
|---|---|---|---|
| I |
| ||
| IIa |
| ||
| IIb |
| ||
| III |
|
Analgesic and anti-ischemic therapy for UA/NSTEMI involves the use of nitroglycerin, morphine, beta blockers, calcium-channel blockers, and angiotensin-converting enzyme (ACE) inhibitors. These agents will help alleviate pain through their mechanisms of action. No NSAIDs should be given because of the documented increased risk of major adverse cardiovascular events [3].
Nitroglycerin is a vasodilator that relieves ischemia-related pain by reducing myocardial oxygen demand and enhancing oxygen delivery. Nitroglycerin can be given as sublingual tablets every five minutes for up to three doses. Nitroglycerin (and all nitrates) is contraindicated when a phosphodiesterase inhibitor has been used recently [3]. Nitrates are used with caution in patients with right ventricular infarction.
Patient A was admitted from the emergency department to an inpatient telemetry/stepdown unit with a diagnosis of ACS. Both the patient's initial cardiac biomarkers and initial ECGs were negative for indications of MI. However, because his initial symptoms (increased severity of chest pain, chest pain at rest) coupled with his history of PCI six months ago for an occlusion in his right coronary artery are highly suspicious for ACS, the physician admitted him for on-going observation and monitoring. A few hours after admission to the inpatient unit, Patient A experienced a chest pain attack at rest. He described the pain simply as "bad," 10/10 on the pain scale, and located in the left substernal area of his chest. His admitting medical orders included nitroglycerin, one tab sublingually every five minutes for chest pain, which may be repeated every five minutes to a maximum of three doses as needed. The nurse obtained an ECG and notified the physician.
In this case example, the patient's chest pain is characteristic of ischemic chest pain: its intensity is "severe," it is located in the left substernal area of his chest, and it occurred at rest. The immediate response should be to check Patient A's vital signs and to administer sublingual nitroglycerin as ordered.
Prior to administering sublingual nitroglycerin, the patient's blood pressure should be checked. If the patient is hypotensive, sublingual nitroglycerin should not be administered and the physician should be notified. Intravenous morphine may be ordered for pain relief instead. If the patient's blood pressure is normal or elevated, sublingual nitroglycerin may be administered as follows [1,34,173]:
Obtain an initial pain rating for the patient's chest pain.
Administer one sublingual nitroglycerin tablet. The tablet should produce a mild burning sensation under the tongue.
Wait five minutes, then recheck the patient's vital signs and chest pain intensity.
Carefully document the episode, including pain ratings, vital signs, and medications administered, in the appropriate part of the patient's medical record.
After a single nitroglycerin tablet, Patient A reported that his chest pain dropped to 4 on a scale of 10, and his blood pressure remained slightly elevated.
Ongoing chest pain indicates continuing ischemia. If the patient's blood pressure has not dropped significantly, a second nitroglycerin tablet should be given. If the patient becomes hypotensive from the first dose, no additional doses should be given and the physician should be notified. Morphine, if ordered, may be given as another drug of choice to relieve chest pain. If the patient's chest pain drops to 0 after the second nitroglycerin tablet, no additional tablets are indicated. However, if the patient's pain persists (even at a low level) and blood pressure remains stable, a third tablet should be given.
Per physician orders, an ECG should be obtained if Patient A has chest pain. Ideally, the ECG would be taken while the patient is still having chest pain. Clinically significant signs of myocardial ischemia, such as ST depression and T-wave inversion, may be seen on 12-lead ECG during chest pain episodes.
A major side effect of nitroglycerin is severe headache. Orders for acetaminophen may be effective in reducing the patient's headache. However, some patients will decline further nitroglycerin therapy due to the discomfort of the associated headache. The patient's physician should be notified if the patient is having chest pain and refusing nitroglycerin.
After administration of two sublingual nitroglycerin tablets, Patient A's chest pain was relieved. He reported that he was chest pain free. One hour later, he again developed chest pain and required a third sublingual nitroglycerin tablet for relief. His blood pressure was elevated during this attack; when his pain was relieved, his blood pressure returned to his baseline normal. Less than one hour later, Patient A developed a third bout of chest pain. He rated the pain as 10/10, and his blood pressure increased to 190/120 mm Hg. Three sublingual nitroglycerin tablets again reduced his chest pain to 0 and his blood pressure decreased to baseline. Because the chest pain episodes are increasing in frequency and intensity, the physician decided to initiate a continuous nitroglycerin drip.
The ACCF/AHA guidelines note that if pain is not relieved, continuous intravenous nitroglycerin may be started; the indications for intravenous nitroglycerin are persistent ischemia, hypertension, or heart failure, following administration of sublingual nitroglycerin and a beta blocker [3]. If ischemia recurs, the rate of infusion may be increased until symptoms are relieved. The administration of intravenous nitroglycerin should be discontinued within 24 hours after the patient's condition has stabilized, at which point oral nitroglycerin can be given. Discontinuation of intravenous nitroglycerin should be gradual, as the abrupt cessation has been associated with exacerbation of ischemic changes on ECG [3].
Depending on the hospital's policy and procedure, nitroglycerin may be ordered in micrograms per minute or as a weight-based calculation (i.e., micrograms per kg per minute). The physician's order should specify the starting dose and rate, the maximum dose and rate, and whether or not the infusion can be increased until the patient is free of chest pain, the maximum dose has been achieved, or the patient becomes hypotensive. Nursing responsibilities include [1,34,173]:
Monitoring the patient's blood pressure frequently while increasing/titrating the infusion
Maintaining the patient on continuous ECG monitoring
Monitoring the effect of the nitroglycerin on the patient's chest pain
Notifying the physician if the patient becomes hypotensive
Notifying the physician if the maximum specified dose is reached and the patient continues to have chest pain
The 2014 ACCF/AHA guideline states that morphine is an option for patients who do not have relief of ischemia-related symptoms during treatment with intravenous nitroglycerin or for patients who have recurrence of symptoms during anti-ischemic therapy [3]. If morphine is used in conjunction with intravenous nitroglycerin, the patient's blood pressure should be closely monitored, as hypotension is a potential adverse effect.
The inhibition of beta-1 adrenergic receptors by beta blockers acts to decrease cardiac work and myocardial oxygen demand. Beta blockers also slow the heart rate, which helps enhance coronary blood flow. A beta blocker should be given orally to all ACS patients (unless contraindicated) within 24 hours of presentation [3]. This use of beta blocker therapy has been associated with significantly lower in-hospital mortality [174]. Contraindications include signs of heart failure, low-output state, increased risk of cardiogenic shock, or other relative contraindications to beta blockade.
Patient A continued to experience severe chest pain; initiation and titration of the nitroglycerin infusion to higher doses did not relieve his pain. ECG showed ST depression in the inferior leads, and his most recent cardiac biomarkers indicated that his troponin levels were positive for myocardial damage. The physician was notified and ordered morphine 2 mg. Patient A remained hypertensive, and his chest pain persisted at a lower intensity (5/10). The physician ordered 5 mg IV of metoprolol to be administered immediately and 25 mg metoprolol to be taken by mouth twice a day.
Nursing responsibilities in the administration of IV metoprolol include maintaining the patient on continuous ECG monitoring; monitoring blood pressure before, during, and after administration; and monitoring heart rate and rhythm before, during, and after administration. Contraindications to metoprolol (or other beta blocker) administration include bradycardia and hypotension [173].
Calcium-channel blockers act to inhibit contraction of myocardial and smooth muscle and cause vasodilation, although the agents in this drug class vary in the degree of vasodilation and myocardial contractility they produce [3]. They also relieve (or prevent) signs and symptoms of ischemia by decreasing heart rate and blood pressure.
The strongest evidence for a benefit of calcium-channel blockers in the setting of UA/NSTEMI primarily relates to symptom control. Calcium-channel blockers are indicated for patients who have UA/NSTEMI and [3]:
Ongoing or recurring ischemia-related symptoms despite adequate doses of nitroglycerin and beta blockers
Intolerance of adequate doses of nitroglycerin or beta blockers
The four agents used most commonly are nifedipine, amlodipine, verapamil, and diltiazem. Although data on comparisons of these four drugs are limited, verapamil and diltiazem are recommended because of their negative inotropic actions and negative chronotropic and dromotropic effects [3]. The ACC/AHA guideline recommends that a nondihydropyridine calcium channel blocker (verapamil or diltiazem) be given to patients with UA/NSTEMI who have continuing or frequently recurring ischemia and a contraindication to beta blockers, provided that clinically significant left ventricular dysfunction, increased risk for cardiogenic shock, a PR interval greater than 0.24 second, or second- or third-degree atrioventricular block without a cardiac pacemaker are not present [3]. In addition, oral nondihydropyridine calcium antagonists are recommended (unless contraindicated) for patients who have recurrent ischemia after appropriate use of beta blockers and nitrates. Immediate-release nifedipine is not recommended for routine use because of a dose-related increase in mortality [3].
Nursing responsibilities when administering calcium-channel blockers include monitoring heart rate and blood pressure prior to administering the medication. In some patients, calcium-channel blockers may cause hypotension and bradycardia. Special caution should be taken if the patient is taking other medications, such as ACE inhibitors, that can lower blood pressure. Especially in the elderly, use of multiple medications will have an additive effect and will be more likely to cause hypotension, orthostatic hypotension, and an increased risk of falls [173].
An ACE inhibitor should be administered orally within the first 24 hours (unless contraindicated) to patients who have pulmonary congestion or a left ventricular ejection fraction (LVEF) less than 40%, and to patients who have hypertension, diabetes mellitus, or stable chronic kidney disease [3]. The guidelines also note that an angiotensin-receptor blocker (ARB) should be given to patients who cannot tolerate an ACE inhibitor and have signs of heart failure or LVEF of less than 40%. The benefits of ACE inhibitors have been demonstrated primarily in the long-term setting after MI, with significant reductions in adverse outcomes, including survival at 30 days [3,175,176].
When administering ACE inhibitors, the following nursing actions should be taken [173]:
Monitor blood pressure for hypotension. Be alert for orthostatic hypotension and syncope.
Implement fall precautions as indicated by patient status.
Monitor serum potassium levels and renal function studies; elevated serum potassium levels or increasing signs of renal insufficiency/failure can be an indication that the medication should be discontinued.
Monitor for the development of intolerable side effects. A common and often fatiguing side effect is a dry, nagging cough.
ARBs such as valsartan and candesartan may be prescribed for persons who cannot tolerate ACE inhibitors [177]. When administering ARBs, the nurse should monitor serum electrolytes, renal function studies, and vital signs, especially blood pressure [173]. Hypotension and orthostatic hypotension may result.
Among patients with UA/NSTEMI, treatment with statins has been shown to be associated with lower rates of recurrent MI, CHD-related mortality, need for myocardial revascularization, and stroke [3]. These benefits have been greater with a high-intensity statin (such as atorvastatin) than with low- or moderate-intensity statins. Thus, the 2014 ACC/AHA guideline recommends that all patients receive high-intensity statin therapy, unless contraindicated [3].
Aspirin continues to be a key element in the treatment of patients with UA/NSTEMI as part of overall antiplatelet therapy and reduces rates of recurrent MI and death [3]. Antiplatelet therapy reduces platelet formation and aggregation, integral components in the formation of a thrombus after plaque disruption.
The ACC/AHA guideline recommends that aspirin be given as soon as possible after a patient arrives in the emergency department and continued indefinitely in patients who tolerate it [3]. However, adherence by emergency medical personnel to guidelines recommending prompt prehospital aspirin administration is only 45% [178]. Aspirin is contraindicated for patients who are allergic to the drug or who have active bleeding; clopidogrel is recommended for patients who cannot tolerate aspirin [3]. Aspirin should be nonenteric-coated and chewable, and the recommended dose is 162–325 mg. A maintenance dose of aspirin should be continued indefinitely, at a daily dose of 81–325 mg. Adherence to the recommended use of aspirin has been better than for other drug therapies for patients with UA/NSTEMI, with rates of 97% to 99% [10,140]. Rates of aspirin use have been reported to be lower for older individuals and women, especially women younger than 55 years of age [18,179].
P2Y12 inhibitors are added to aspirin as dual-antiplatelet therapy for patients who are managed medically as well as patients treated with PCI. Three inhibitors have been approved by the U.S. Food and Drug Administration (FDA) for use in UA/NSTEMI: clopidogrel, prasugrel, and ticagrelor.
Clopidogrel
Clopidogrel was the first antiplatelet agent to become standard therapy in the ACS setting. The drug was approved by the FDA in 2002 on the basis of the findings of the Clopidogrel in Unstable Angina to Prevent Recurrent Events (CURE) trial, in which 12,562 patients with UA/NSTEMI were randomly assigned to treatment with aspirin with or without clopidogrel (loading dose of 300 mg followed by 75 mg daily) and followed up for 3 to 12 months, regardless of the treatment strategy used (conservative or invasive) [180]. The risk of cardiovascular-related death, MI, or stroke was significantly lower for patients who received clopidogrel. The results were similar in many subgroups of patients.
The ACC/AHA guideline recommends clopidogrel as one of two P2Y12 inhibitors to be given in addition to aspirin to all patients (unless contraindicated) with UA/NSTEMI who are to be treated with either an early invasive or ischemia-guided strategy [3]. The recommended dose of clopidogrel is a loading dose of 300 mg or 600 mg, followed by 75 mg daily for up to 12 months. Clopidogrel is also recommended for patients who are unable to take aspirin [3].
Patient D was scheduled to go to the cardiac catheterization laboratory for a left heart catheterization and probable PCI with stent to treat an obstruction in the circumflex branch of his left coronary artery. The cardiac catheterization laboratory physician's orders specified that Patient D should receive a loading dose of 300 mg of clopidogrel on call to the catheterization laboratory. When the nurse brought the patient the medication as ordered, he commented, "I know that one. They wanted me to take it last year after my last heart attack and stent. But I couldn't afford it. That stuff is expensive!"
In today's economic climate, the cost of medications can pose a serious problem for the patient. Patients who are uninsured or underinsured can find it difficult to afford medications such as clopidogrel. Even patients with "good" insurance can find co-pay charges too high to manage on their current budget. Variations in Medicare Part D plans can create confusion and obstacles. Some drug companies may offer assistance; local hospitals may also provide assistance through resources such as charity pharmacies. Nurses are in a position to initiate discussion with the patient and family about how they plan to obtain medications after discharge and can tactfully ask if the patient has any financial issues related to obtaining prescribed medications. If the patient or family indicates a need, a case manager, discharge planner, or social worker can assess financial issues and assist patients/families to identify available resources. If a patient is unable to afford (or is unlikely to adhere to) taking clopidogrel following PCI with stent placement, the physician may choose to implant bare-metal stents (as opposed to drug-eluting stents). The different types of stents will be discussed in detail in a later section of this course.
Prasugrel
Prasugrel has been shown to be more effective than clopidogrel for patients treated with PCI with stenting. In a comparison of the two drugs in patients with moderate-to-high-risk ACS who were scheduled for PCI, prasugrel was given as a 60-mg loading dose, followed by 10 mg daily, and clopidogrel was given as a 300-mg loading dose, followed by 75 mg daily. Both drugs were given for 6 to 15 months. Prasugrel was associated with a significantly lower rate of the primary composite endpoint of cardiovascular-related death, nonfatal MI, or nonfatal stroke (9.9% vs. 12.1%) [181]. However, the risk of major bleeding was increased with prasugrel (2.4% vs. 1.8%). Overall mortality did not differ significantly between the two drugs [181].
Prasugrel has also been compared with clopidogrel in patients with UA/NSTEMI who are managed medically. In this study, prasugrel was not associated with a decrease in the primary composite endpoint of cardiovascular-related death, MI, or stroke (13.9% vs. 16%) [182]. The rates of major bleeding were similar.
The ACC/AHA guideline recommends prasugrel as one of three options for maintenance antiplatelet therapy (with aspirin) for patients who have PCI and coronary stenting. Prasugrel is not recommended for patients treated with an early-invasive or ischemia-guided strategy [3].
Monitor patients for enhanced bleeding effects if used concurrently with warfarin. Instruct patients on increased risk of bruising and bleeding with prasugrel. Due to the increased risk of bleeding, the drug should be withheld 5 to 10 days prior to any surgery or dental procedure [183].
Ticagrelor
Ticagrelor, the first in a new class of antiplatelets known as cyclopentyl-triazolo-pyrimidines, was approved by the FDA in 2011 [184]. Its mechanism of action differs from that of clopidogrel and prasugrel in that it does not require hepatic metabolism for activation and its action is reversible. Ticagrelor achieves greater and more consistent platelet inhibition than clopidogrel [184].
Ticagrelor was compared with clopidogrel in the Study of Platelet Inhibition and Patient Outcomes (PLATO), a randomized, controlled trial involving 18,624 patients, most of whom had UA/NSTEMI [185]. After 12 months, the rate of the primary composite endpoint (i.e., cardiovascular-related death, MI, or stroke) was lower in the ticagrelor and aspirin group than in the clopidogrel and aspirin group (9.8% vs. 11.7%) [185]. In addition, the all-cause death rate was lower in the ticagrelor group than in the clopidogrel group. Although the overall rates of major bleeding did not differ between the two groups, ticagrelor was associated with a higher rate of major bleeding in a subgroup of patients who did not have CABG.
The ACC/AHA guideline recommends ticagrelor as an option (with aspirin) as maintenance antiplatelet therapy for up to 12 months after initial treatment with either an early invasive or ischemia-guided strategy [3]. As a class IIaB recommendation, the ACC/AHA note a preference for ticagrelor over clopidogrel. The recommended dose is 180 mg as a loading dose, followed by 90 mg twice daily. The benefit of ticagrelor compared with clopidogrel is limited to an aspirin dose of 75–100 mg [186].
Adherence to guidelines on the use of a P2Y12 inhibitor has been low, especially for patients with UA/NSTEMI, with rates of 10% to 57% [8]. Rates of use have been lower among women [11]. In addition, some inhibitors have been used inappropriately; for example, in one study, 3% of patients with prior stroke received prasugrel despite its contraindication in that setting [8].
Glycoprotein IIb/IIIa inhibitors are potent inhibitors of platelet aggregation. Three intravenous glycoprotein IIb/IIIa inhibitors have been approved for clinical use: abciximab, eptifibatide, and tirofiban. Intravenous glycoprotein IIb/IIIa inhibitors are recommended, as oral agents in this class have been associated with increased risk for bleeding and mortality [3]. A meta-analysis (48 trials, 33,513 patients) demonstrated that glycoprotein IIb/IIIa inhibitors were associated with a lower all-cause mortality at 30 days after PCI but not at six months, compared with placebo or usual care [187]. The rate of severe bleeding was increased with glycoprotein IIb/IIIa inhibitors. Less benefit was found when clopidogrel was used. When glycoprotein IIb/IIIa inhibitors were used as part of initial medical treatment of UA/NSTEMI (12 trials, 33,176 patients), there was no decrease in mortality at 30 days, although the rate of death or MI was slightly lower at 30 days and six months [187]. Again, the risk of severe bleeding was higher with glycoprotein IIb/IIIa inhibitors.
The ACC/AHA guideline recommends a glycoprotein IIb/IIIa inhibitor for patients at intermediate-to-high risk (i.e., elevated troponin levels) who are to be treated with an early invasive strategy and dual-antiplatelet therapy. Eptifibatide and tirofiban are the preferred inhibitors (class IIbB) [3]. The recommended use of glycoprotein IIb/IIIa inhibitors is suboptimal in two ways. First, guideline-recommended use is low, especially among women [11,188,189]. Despite the clear benefit of glycoprotein IIb/IIIa inhibitors for high-risk patients, studies have shown that treatment with the drugs are directed toward patients at lower risk, with its use in high-risk patients ranging from 18% to 35% [190,191]. Use of glycoprotein IIb/IIIa inhibitors has also been suboptimal with respect to dosing; in one study, an excess dose was given to 26.8% of patients [192]. Excess dosing was more likely among older individuals, women, and patients with renal insufficiency, diabetes, heart failure, or low body weight [192]. Increased risk of major bleeding and mortality were associated with an excess dose.
Parenteral anticoagulant therapy (in addition to antiplatelet therapy) is recommended for patients with definite or likely UA/NSTEMI, regardless of the initial treatment strategy (early invasive or ischemia-guided) [3].
The anticoagulants used in the UA/NSTEMI setting are enoxaparin, bivalirudin, fondaparinux, and unfractionated heparin [3].
Enoxaparin is a low-molecular-weight heparin that offers many pharmacologic advantages compared with unfractionated heparin [193]:
More predictable anticoagulant effect
Greater bioavailability
Lower incidence of heparin-induced thrombocytopenia
Routine monitoring not required
Given as a fixed-weight based dose
Compared with unfractionated heparin, enoxaparin has been associated with lower rates of recurrent ischemic events and of invasive procedures in the short term, as well as at 1 year among patients with UA [194]. Among high-risk patients with UA/NSTEMI treated with an early invasive strategy, the rate of death or MI at 30 days did not differ significantly between enoxaparin and unfractionated heparin, and enoxaparin was associated with an increased risk of major bleeding [152,195]. A 2018 systematic review and meta-analysis found similar death rates and major bleeding between enoxaparin and unfractionated heparin [196].
The ACC/AHA guideline recommends enoxaparin as an option for all patients with NSTE-ACS [3]. The recommended dose is 1 mg/kg, given subcutaneously, every 12 hours, and the drug is continued throughout the hospitalization or until PCI is done [3]. The dose should be decreased to 1 mg/kg daily for patients with a creatinine clearance less than 30 mL/min.
Studies have shown that 14% to 19% of patients with UA/NSTEMI have received an excess dose of low-molecular-weight heparin [192,197]. A higher dose was significantly associated with major bleeding and death [197]. The patients who received excess doses were more likely to be older, smaller, and female [192,197].
Bivalirudin is a direct thrombin inhibitor, and it has shown little benefit in lowering the risk of adverse outcomes compared with unfractionated heparin. Bivalirudin has been evaluated only in patients being considered for an early invasive strategy. In a study of 13,819 moderate- and high-risk patients, bivalirudin alone was compared with two other regimens: bivalirudin plus a glycoprotein IIb/IIIa inhibitor, and heparin (unfractionated heparin or enoxaparin) plus a glycoprotein IIb/IIIa inhibitor. Bivalirudin plus a glycoprotein IIb/IIIa inhibitor was noninferior to heparin plus a glycoprotein IIb/IIIa inhibitor with respect to composite endpoint (death, MI, or unplanned revascularization) at 30 days [198]. Bivalirudin alone was also noninferior to heparin plus a glycoprotein IIb/IIIa inhibitor, but it offered a significant benefit in terms of major bleeding [198]. At one year, there was no significant difference in the composite endpoint among the three groups [199]. A meta-analysis of 15 trials that included more than 25,000 patients undergoing PCI found that bivalirudin was associated with an increased risk of stent thrombosis, MI, all-cause mortality, and major adverse cardiac events and a reduced risk of major bleeding. When the dose of heparin in the control arm was more than 100 units/kg, bivalirudin was associated with a reduction in major bleeding; when the dose of heparin was less than 75 units/kg, bivalirudin was not associated with reduced major bleeding [200].
The ACC/AHA guideline recommends bivalirudin only for patients who are to have an early invasive strategy [3]. The recommended dose is 0.10 mg/kg as a loading dose, followed by 0.25 mg/kg/hour, to be continued until diagnostic angiography or PCI is performed [3].
Fondaparinux is a synthetic polysaccharide molecule that is a selective inhibitor of activated Factor X. It has been compared with enoxaparin in patients with NSTE-ACS and found to have similar efficacy in terms of a primary endpoint of ischemic events, but offering benefit in terms of a significantly lower rate of major bleeding [201,202,203]. The ACC/AHA guideline recommends fondaparinux, 2.5 mg subcutaneously daily, for the duration of hospitalization or until PCI is done [3]. When fondaparinux is used alone in this setting, an additional anticoagulant with anti-IIa activity should be given to help prevent catheter thrombosis [3].
Unfractionated heparin has been used in the ACS setting since the early 1960s. Heparin prevents the formation of thrombi by accelerating the action of the proteolytic enzyme antithrombin that inactivates Factors IIa, IXa, and Xa [193]. An early meta-analysis (six trials, 1,353 patients) showed that unfractionated heparin plus aspirin reduced the risk for death or MI by 33% compared with aspirin alone among patients with UA [204]. These studies preceded the era of dual-antiplatelet therapy and early catheterization and revascularization.
The ACC/AHA guideline recommends giving unfractionated heparin for 48 hours or until PCI is performed [3]. A weight-adjusted dose is preferred to a fixed initial dose, as anticoagulation is more predictable with such dosing [3]. The recommended dose in the ACC/AHA guideline is an initial loading dose of 60 IU/kg (to a maximum of 4,000 IU) and an initial infusion of 12 IU/kg/hour (to a maximum of 1,000 IU/hour), which is adjusted to a therapeutic aPTT range [3].
As stated earlier, risk stratification is essential to determine the level of treatment: an early invasive or an ischemia-guided strategy. An early invasive approach involves diagnostic angiography, with revascularization performed if appropriate based on coronary anatomy [3]. The procedure is typically done within 24 hours (early invasive) or 25 to 72 hours (delayed invasive). The optimal timing of angiography has not been established [3]. With an ischemia-guided strategy (previously referred to as a conservative approach or medical management), noninvasive testing is done and angiography is performed only when testing demonstrates evidence of ischemia. The ACC/AHA guideline provides direction for appropriately selecting an early invasive or ischemia-guided strategy (Table 10) [3].
FACTORS Associated With Appropriate Selection of Early Invasive Strategy or Ischemia-Guided Strategy in Patients With NSTE-ACS
| Treatment Strategy | Factors Guiding Selection | |||||||
|---|---|---|---|---|---|---|---|---|
| Immediate invasive (within two hours) |
| |||||||
| Ischemia-guided strategy |
| |||||||
| Early invasive (within 24 hours) |
| |||||||
| Delayed invasive (within 25 to 72 hours) |
| |||||||
| CABG = coronary artery bypass graft; EF = ejection fraction; GFR = glomerular filtration rate; GRACE = Global Registry of Acute Coronary Events; HF = heart failure; LV = left ventricular; NSTE-ACS = non-ST-elevation acute coronary syndrome; PCI = percutaneous coronary intervention; TIMI = Thrombolysis In Myocardial Infarction; Tn = troponin; VF = ventricular fibrillation; VT = ventricular tachycardia. | ||||||||
The findings of most studies have indicated that a routine early invasive strategy is superior to an ischemia-guided strategy in terms of reducing the rate of cardiovascular-related death or MI, as well as of angina and rehospitalization [17,205,206]. However, a follow-up Cochrane review concluded that there was no evidence of appreciable benefit with routine invasive strategies and that a selectively invasive (conservative) strategy based on clinical risk for recurrent events is the preferred management strategy [207]. Additionally, a meta-analysis found insufficient evidence to support either approach as having a survival benefit for patients with NSTE-ACS [208]. The greatest advantage of an early invasive strategy has been found among patients at high risk.
An urgent or immediate invasive strategy is recommended for patients with NSTE-ACS with refractory angina or hemodynamic or electrical instability who do not have serious comorbidities or contraindications [3]. An early invasive strategy is recommended for patients with NSTE-ACS who are initially stabilized and at elevated risk for clinical events [3]. The guideline recommends against an early invasive strategy for patients with acute chest pain and a low likelihood of ACS (normal troponin levels) as well as for patients with extensive comorbidities (class III: no benefit).
The objective of an ischemia-guided strategy is to avoid unnecessary treatment (and associated costs) for patients at low risk for significant CHD. The ACC/AHA guideline notes that an ischemia-guided strategy may be considered for patients with NSTE-ACS who are initially stabilized and at elevated risk for clinical events (class IIbB) [3]. It is also reasonable to consider clinician and patient preference in decision making about an ischemia-guided strategy (class IIbC). Patients at low or intermediate risk who have had no ischemia at rest or with low-level activity for at least 12 to 24 hours should have noninvasive stress testing (class IB) [3].
Many factors other than risk influence the use of an early invasive strategy. Such a strategy has been used more often, regardless of patients' risk, when a cardiac catheterization laboratory is available or the treating physician is a cardiologist [190,209,210]. Patient demographic characteristics, such as age, race, and gender, are also factors. Data from trials indicate that an early invasive strategy is used less frequently for older patients, Black patients, and women [9,14,109,206,209,211].
The benefit of an early invasive strategy for women is unclear [17,206]. However, when women have high-risk features, such as elevated troponin levels, an early invasive approach does lead to better outcomes; women at low-risk have better outcomes from an ischemia-guided approach [212,213]. These findings led the ACC/AHA to emphasize that an immediate invasive strategy should be used for women who are eligible for that approach and that an early invasive strategy should not be used for women at low risk for ACS [3].
CABG was once the primary revascularization procedure, but advances in less invasive techniques have contributed to a decline in CABG rates and an increase in the use of PCI for NSTE-ACS [9,214].
A comprehensive comparison of CABG and PCI was carried out in the Synergy between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery (SYNTAX) study, and the findings were considered in the formulation of the 2011 ACC/AHA/Society for Cardiac Angiography and Interventions (SCAI) guideline recommendations for PCI [5]. In a meta-analysis (31 trials, 15,004 patients) published after the guideline, among patients eligible for either PCI or CABG, the latter procedure was associated with lower rates of repeat revascularization, and death; the rate of MI was similar, and the rate of stroke was higher with CABG [215].
Class I recommendations for the use of PCI include patients who have refractory angina or hemodynamic or electrical instability (without comorbidities or contraindications), and initially stabilized patients who have an elevated risk for clinical events [5]. PCI is preferred for patients with discrete lesions, in large-caliber vessels, or one or two vessels, whereas CABG is recommended for more extensive CHD, including left main disease, three-vessel disease, or two-vessel disease with severe involvement of the proximal left anterior descending coronary artery [6]. For patients with multivessel disease, CABG has been associated with higher adjusted rates of long-term survival and lower rates of MI and repeat vascularization compared with PCI with stenting [216,217]. CABG is also recommended for patients with left ventricular systolic dysfunction [6].
Patient V, a woman 45 years of age, was admitted to a general medical-surgical unit with a diagnosis of possible upper gastrointestinal bleeding. She stated that she had no known cardiac history; however, she had risk factors for CHD, including a current history of 1 to 2 packs per day smoking history and dyslipidemia for which she takes simvastatin.
Two days following admission, Patient V called the nurse complaining of extreme, severe chest pain that started while she was in the bathroom. The physician was notified and ordered cardiac biomarkers and a 12-lead ECG. Sublingual nitroglycerin tablets were administered and effectively relieved the acute chest pain. The patient's biomarkers returned negative for MI; however, her ECG during the chest pain episode showed ST-segment elevation. A follow-up ECG, taken when the pain had resolved, showed resolution of ST-segment elevation and no electrocardiographic indications of an evolving or resolving MI.
After careful assessment and evaluation of serial laboratory test, serial ECGs, physical exam findings, and other diagnostic tests, the physician determined that Patient V had variant (Prinzmetal or vasospastic) angina. Diltiazem was ordered to prevent coronary vasospasm and recurrent chest pain attacks.
The primary medical therapy for management of variant or vasospastic angina involves nitrates and calcium-channel blockers. Within minutes of administration, nitroglycerin has been found to effectively treat episodes of angina and myocardial ischemia caused by vasospasm. Long-acting nitrates can reduce the frequency of recurrent episodes of chest pain. Calcium-channel blockers, specifically nifedipine, amlodipine, verapamil, and diltiazem, are prescribed to prevent coronary vasospasm and the subsequent ischemia that can result. In this patient population, calcium-channel blockers are preferred over beta blockers [218,219].
Patient C presented to the emergency department with a complaint of severe substernal chest pain, radiating from the left side of his chest down his left arm. He stated that he was "very nauseated" and that his symptoms came on suddenly. The patient is 19 years of age; when questioned, he admitted that he smoked 1 to 2 packs per day but denied all other risk factors for CHD. He had no previous history of ACS or interventions for CHD, such as PCI. He appeared "jittery" and anxious and asked to leave the emergency department to smoke. His initial 12-lead ECG showed sinus tachycardia but no evidence of myocardial ischemia or infarct. His initial biomarkers showed troponin I within normal limits. Upon careful questioning by the emergency department physician, Patient C admitted that he used cocaine approximately one hour before the development of his symptoms.
The 2008 AHA statement contains several recommendations for the management of patients with cocaine-associated chest pain and MI [48]. Because cocaine use may impact treatment, patients (especially younger patients) who present with signs of possible ACS should be asked about cocaine use. Establishing that a patient does use cocaine should depend primarily upon self-reporting. However, a urine toxicology screen that measures cocaine metabolites (as well as other drug metabolites) may be indicated in patients who are young, have a history of illicit drug use, or who are unable to communicate with the healthcare team [48].
Evaluation of possible cocaine-induced chest pain in the emergency department should follow the same guidelines as the evaluation for ACS without cocaine use. Troponin levels should be monitored. Because cocaine can cause a breakdown of muscle fibers resulting in the release of myoglobin into the bloodstream, elevated myoglobin and total creatine kinase levels may be present that are not indicative of myocardial ischemia or infarct. Cardiac troponins are the biomarkers of choice to assess for a diagnosis of infarction [3,48,220].
Patients with cocaine-induced chest pain who show ECG and biomarker evidence of ischemia or infarct should be admitted for monitoring, observation, and further treatment as indicated. General medical therapies, similar to those used in management of non-cocaine related ACS, should be employed. In addition, the use of IV benzodiazepines as part of the early management of these patients may be indicated. In patients who use cocaine, benzodiazepines help to relieve chest pain and manage neuropsychiatric manifestations. Aspirin, calcium-channel blockers, and nitroglycerin are also recommended; beta blockers are not recommended with acute cocaine intoxication [3,48,220].
Patient K, a man 59 years of age, was admitted to the hospital with a diagnosis of possible H1N1 flu. He was treated with appropriate medical therapy, and his condition improved. On the day before his expected discharge, he called the nurse and complained of a severe, stabbing pain in his chest. He was diaphoretic and complained of feeling nauseated. His blood pressure was elevated to 170/90 mm Hg, and his heart rate was 100-110 beats per minute. He rated his pain 10 out of 10 and stated the pain was located in his left chest, left arm, and back. An ECG was completed, and blood for cardiac biomarkers was obtained. The 12-lead ECG showed non-specific ST-wave changes. A serial 12-lead ECG taken 30 minutes later, however, showed ST elevation in the anterior leads. Cardiology confirmed a diagnosis of STEMI.
When an ECG demonstrates ST-segment elevation, the goal of treatment is to immediately restore normal coronary perfusion through the occluded infarct-related artery, thus decreasing ischemic time [2]. Re-establishing blood flow through the occluded artery is crucial for limiting the size of the infarct, minimizing myocardial damage, preserving left ventricular function, decreasing morbidity, and improving survival [2,221]. Options for re-establishing normal coronary blood flow through an occluded artery include:
PCI with or without placement of intracoronary stents
Fibrinolytic therapy
Combination PCI and fibrinolytic therapy
CABG surgery
Advances in revascularization procedures and antiplatelet and anticoagulant therapies have improved outcomes for patients with STEMI, with significant decreases in the rates of mortality and morbidity [2,222,223]. The reported mortality rates are approximately 5% to 6% (in-hospital) and 7% to 18% (one-year) [2]. Morbidity includes heart failure, pulmonary edema, reinfarction, cardiogenic shock, and stroke, and rates of these events have also declined significantly [222].
Reperfusion therapy is the cornerstone in the management of STEMI, and antiplatelet and anticoagulant agents are necessary as ancillary therapy. The options for reperfusion include revascularization procedures and/or pharmacologic (fibrinolytic) therapy. As with the treatment for NSTEMI, the use of PCI has become the primary approach to revascularization; approximately 80% to 90% of patients have PCI revascularization based on angiographic findings [224]. In addition, PCI is the preferred strategy for reperfusion because of its superior outcomes compared with fibrinolytic therapy [2,224]. However, gaining the optimal benefit from PCI depends on many factors, and timing is the most important variable in selecting a reperfusion therapy [2,221]. Care should also be taken to evaluate patients for contraindications to fibrinolytic therapy [5].
The ACCF/AHA guideline on the management of STEMI was most recently updated in 2013. The guideline notes that patients with STEMI should be treated in either a coronary care unit or a stepdown unit [2]. Care provided in a coronary care unit should be structured according to evidence-based protocols, and nursing staff should be certified in critical care. Patients who are admitted to a coronary care unit may be transferred to a stepdown unit once they have been clinically stable for 12 to 24 hours [2]. Low-risk patients who have had successful PCI may be admitted directly to a stepdown unit.
A familiar adage associated with STEMI is "time is muscle," and every effort should be made to shorten the ischemic time as much as possible. The timing of reperfusion therapy is a complex issue involving the time from the onset of symptoms and the time from presentation to treatment. The time for transfer to another hospital is also a factor for most patients, as most hospitals do not have a cardiac catheterization laboratory and a skilled, readily available PCI team.
The 2013 ACCF/AHA guideline indicates that PCI is preferred over fibrinolytic therapy for patients with STEMI when it can be performed in a timely manner by experienced operators [2]. PCI should be done within less than 90 minutes after the patient's arrival at the emergency department (door-to-device time) [2]. If PCI cannot be done within 90 minutes, fibrinolytic therapy should be initiated as the reperfusion strategy within 120 minutes of the first medical contact.
The most significant factor in achieving an optimal outcome from PCI is timing. Findings from hospitals reporting to the Centers for Medicare and Medicaid Services have shown an improvement in the number of patients treated with primary PCI within the recommended 90-minute window, from 44.2% in 2005 to 91.4% in 2010 [225]. In addition, the median door-to-balloon or door-to-device time declined from 96 minutes in 2005 to 64 minutes in 2010 [225].
Improvements in door-to-balloon time have been attributed to national initiatives focused on identification of barriers to appropriate care and implementation of innovative protocols. For example, a quality improvement campaign called Door-to-Balloon (D2B) Alliance for Quality, launched by the ACC, has made it possible for patients experiencing STEMI anywhere in the United States to receive lifesaving reperfusion in less than 90 minutes and often in less than 60 minutes [226]. These initiatives successfully addressed physician and organizational barriers with efforts to develop systems of care that increase patient access to primary PCI based on whether the patient presents to a PCI-capable or non-capable facility [2].
Specific strategies that have improved the door-to-device time interval focus on three key components: door-to-ECG time, ECG-to-catheterization laboratory time, and laboratory arrival-to-device time. The ACCF/AHA provides the following steps as a general protocol in improving door-to-device times [2]:
A prehospital ECG to diagnose STEMI is used to activate the PCI team while the patient is en route to the hospital.
Emergency physicians activate the PCI team.
A single call to a central page operator activates the PCI team.
A goal is set for the PCI team to arrive in the catheterization laboratory within 20 minutes after being paged.
Timely data feedback and analysis are provided to members of the STEMI care team.
PCI is an invasive procedure performed in the cardiac catheterization laboratory by a highly skilled, trained team. In the treatment of STEMI, the goal is to open the occlusion in the infarct-related vessel, restoring blood flow and oxygen supply. As noted, PCI has become more commonly used than CABG for revascularization. PCI for STEMI can be subcategorized according to when the procedure is done and whether it is done in conjunction with fibrinolytic therapy. Primary PCI refers to PCI that is done alone as primary treatment after diagnostic angiography [2]. (As will be described, ancillary treatment with anticoagulant and antiplatelet agents should be given to support PCI.) Facilitated PCI was once a strategy of full- or half-dose fibrinolysis (with or without glycoprotein IIb/IIIa inhibitors) and immediate transfer for planned PCI within 90 to 120 minutes [2]. However, no net clinical benefit has been found with this strategy, and it is not recommended [2]. Rescue PCI refers to transfer for PCI after fibrinolysis has failed. A pharmacoinvasive strategy is the administration of fibrinolytic therapy, in either the prehospital setting or at a non-PCI-capable hospital for early coronary angiography and PCI when appropriate [2].
PCI encompasses a variety of procedures that may be used to restore blood flow through an occluded artery. These procedures include percutaneous transluminal coronary angioplasty, or balloon angioplasty, and angioplasty with placement of one or more intracoronary stents. In PCI, a slender balloon-tipped catheter is inserted through an artery in the groin to the area of blockage in the coronary artery. Once in position, the balloon is inflated, compressing the plaque and dilating the narrowed coronary artery so that blood can flow more easily [33,34].
To maintain patency in the newly re-opened artery, intracoronary stents may be deployed. Best described as a wire metal-mesh tube, an intracoronary stent is carried by a balloon catheter to the area of the blockage. When the balloon is inflated, the stent expands and locks in place against the vessel wall, keeping the lumen of the vessel open. Blood flow to the affected area of the heart is restored, and myocardial ischemia is relieved. The stent stays in the artery permanently. Within a few weeks of the time a stent is placed, the endothelium of the artery grows over the metal surface of the stent [33,34].
Following stent placement, occlusions may develop in a stent or near the junction between the end of a stent and the native vessel. To combat this issue, researchers developed a new type of stent called a drug-eluting stent; these stents are coated with medications that reduce inflammation and thrombus formation, thereby reducing the risk of restenosis at the site of the stent. Stents not coated with drugs are called bare-metal stents. Not all occlusions or all vessels are amenable to balloon dilatation or deployment of stents. In some cases, the degree of coronary occlusion is too great to be re-opened through percutaneous means. Coronary artery bypass surgery may be indicated in these cases. PCI also cannot be performed on smaller vessels that branch off from the major arteries; the lumens in these vessels are too small to permit safe passage of the catheter [33,34].
Primary PCI is preferred because of the many advantages it offers compared with fibrinolytic therapy, including wider eligibility, better rates of reperfusion, lower risks, and improved outcomes [100,224,227]. PCI is especially preferred for high-risk patients, specifically patients 75 years of age and older, patients with an unclear diagnosis, and patients with cardiogenic shock, heart failure, or ventricular arrhythmias [2]. However, analysis of data has shown that PCI has been done less often among patients at high risk (41%) than among patients at low risk (60%) or intermediate risk (54%) [190].
Class I indications for primary PCI include the following [5]:
STEMI symptoms within 12 hours (level A)
Severe heart failure or cardiogenic shock (level B)
Contraindications to fibrinolytic therapy with ischemic symptoms less than 12 hours (level B)
The ACC/AHA guideline notes that PCI is reasonable for patients with clinical and/or ECG evidence of ongoing ischemia 12 to 24 hours after onset of symptoms (class IIaB) and might be considered for asymptomatic patients with STEMI and higher risk who presented between 12 and 24 hours after the onset of symptoms (class IIbC) [5].
The use of coronary stents during PCI reduces the rates of adverse events such as reocclusion, restenosis, and target-vessel revascularization [5,100,224]. Drug-eluting stents have been associated with lower long-term rates of target-vessel revascularization and restenosis compared with bare-metal stents, but the reduction has varied among the many types of drug-eluting stents and stent thrombosis was originally a complication [228,229]. Subsequent-generation drug-eluting stents were developed to overcome this complication, and thin-strut fluoropolymer-coated cobalt chromium everolimus-eluting stents have been associated with rates of stent thrombosis that are lower than those for other types of drug-eluting stents or bare-metal stents [230]. The first of the subsequent-generation stents were designed to compensate for the insufficient radial strength of the polymer materials, which resulted in higher thrombosis rates than conventional drug-eluting stents. Newer-generation stents have improved structural design, postprocessing of bioresorbable polymer materials, or altering bioresorbable metallic alloys [231,232].
The complications of primary PCI include adverse reactions to the contrast medium, volume loading, difficulty with arterial access, and technical complications [100]. Reperfusion injury and hemorrhagic transformation of a bland infarction and hemorrhagic stroke are rare after primary PCI [224].
Primary PCI is supported by antiplatelet and antithrombin therapy. Class I recommendations for this therapy in patients with STEMI include the following [5]:
Aspirin (level B)
P2Y12 inhibitors (level A)
Unfractionated heparin (level C)
Bivalirudin (level B)
The aspirin dose before PCI should be 325 mg for patients who had not been taking aspirin therapy and 81–325 mg for patients who had already been taking daily aspirin [5]. If stents are to be implanted during PCI, a loading dose of a P2Y12 inhibitor should be given (clopidogrel, 600 mg; prasugrel, 60 mg; or ticagrelor, 180 mg) [5]. For clopidogrel, a 300-mg loading dose is recommended for patients who have PCI within 24 hours after receiving fibrinolytic therapy; a 600-mg loading dose is recommended for patients who have PCI more than 24 hours after receiving fibrinolytic therapy [5]. This recommendation is based on the results of several investigations to explore various loading doses of clopidogrel before or during PCI. A meta-analysis of seven studies demonstrated that a 600 mg loading of clopidogrel reduces the rate of adverse cardiovascular events without an increase in major bleeding compared with 300 mg [5]. The findings of another study suggested that a 600-mg loading dose (compared with a 300-mg dose) is associated with improvements in procedural angiographic endpoints and one-year clinical outcomes in patients with STEMI who undergo primary PCI [5]. No benefit is derived from increasing the loading dose to 900 mg compared with 600 mg. The guideline acknowledges that the safety and efficacy of pretreatment with clopidogrel remains controversial [5].
When compared with clopidogrel, prasugrel was associated with a 2.2% reduction in a composite endpoint of cardiovascular-related death, nonfatal reinfarction, or nonfatal stroke [5]. Prasugrel is contraindicated in patients with active pathologic bleeding or history of transient ischemia attack or stroke. Its use is not recommended for patients older than 75 years of age because of increased risk of fatal intracranial bleeding [5].
If unfractionated heparin is used, it is reasonable to give a glycoprotein IIb/IIIa inhibitor (abciximab, double-bolus eptifibatide, or high-bolus tirofiban), regardless of whether patients are pretreated with clopidogrel [5]. The ACCF/AHA guideline for STEMI states that it is reasonable to begin treatment with abciximab before or at the time of primary PCI (with or without stenting) [2]. The precise timing of administration has not been defined. Treatment with tirofiban or eptifibatide may also be considered at the time of primary PCI [2].
With regard to anticoagulant therapy, unfractionated heparin is recommended but should not be given to patients already receiving therapeutic enoxaparin (subcutaneously) (class III: harm) [5]. Bivalirudin is also a recommended anticoagulant, with or without previous treatment with unfractionated heparin (class IB) [5]. Bivalirudin or argatroban should be used instead of unfractionated heparin in patients with heparin-induced thrombocytopenia (class IB). Fondaparinux should not be used as the only anticoagulant with PCI (class III) [5]. An additional anticoagulant with anti-Ha activity should be used because of the risk of catheter thrombosis.
Upon further questioning, Patient K reported a history of CHD with stent placement 5 years previously and CABG surgery 10 years previously. The medical team determined that primary PCI was indicated to open the occluded, infarct-related vessel. While awaiting the start of the procedure, Patient K received aspirin 325 mg and 600 mg of clopidogrel. He also received a bolus of abciximab, and a continuous infusion was started.
Monitoring the patient closely for complications and signs of recurrent ischemia is particularly important in the 24-hour period following reperfusion with PCI. Complications may include bleeding, formation of clot or obstruction, drop in platelet count, reocclusion, renal failure, and cerebrovascular accident [34,233].
Bleeding may occur from the arterial puncture site. Initial indications include frank bleeding from the puncture site and/or development of a hematoma in the area surrounding the site. A retroperitoneal bleed may also occur; an early sign is a complaint of severe flank pain. To reduce the likelihood of bleeding, the patient should be maintained on bed rest as specified by physician orders. The length of time bed rest is indicated depends on the method used to close the arterial puncture site. The arterial puncture site, often the femoral artery, should be monitored frequently for signs of bleeding or hematoma formation [34,233].
Formation of a clot at the puncture site reduces distal arterial blood flow and can result in signs of peripheral ischemia below the site. Indications include loss of or decrease in the peripheral pulse distal to the arterial puncture site and change in color or temperature of the distal extremity. The peripheral pulse distant to the site should be checked frequently with vital signs and arterial site checks [34,233].
A significant drop in platelet count may be caused by an allergy or intolerance to infusing glycoprotein IIb/IIIa inhibitors. With a drop in platelet count, the patient's risk of bleeding increases. Patients receiving glycoprotein IIb/IIIa inhibitors should have a complete blood count checked at designated intervals to make sure that platelet counts are not dropping. Parameters should include orders to notify the physician if the platelet count drops below a specified level. If a patient develops a significant drop in platelet count, the infusion of the glycoprotein IIb/IIIa inhibitor is discontinued and the patient is placed on bleeding precautions and observed carefully for any signs of bleeding [34,233].
Abrupt reocclusion of the infarct-related artery can occur within hours of the original procedure. A thrombus may form in the newly placed stent, occluding blood flow and causing symptoms of myocardial ischemia or infarct. Clinical indications include the recurrence of severe chest pain. This chest pain may be similar or worse than the patient's initial chest pain. ECG changes indicative of acute ischemia or infarct may appear. Cardiac biomarkers may trend upward. The treatment of choice is an emergent return to the cardiac catheterization laboratory for direct visualization of the vessels and possible removal of a thrombus in or near the newly placed stent. Cardiac biomarkers should be monitored post-PCI. Troponin levels that fall from previously high levels are indicative of restored perfusion; levels that initially drop then trend upward again are concerning for possible recurrent damage. Continuous ECG monitoring should also be maintained. If only 2 or 3 leads can be monitored continuously, the leads selected for monitoring should be the ones most likely to reflect any recurrent ST-segment changes [34,233].
Renal failure can develop from the kidneys' response to the dye load administered during cardiac catheterization. Postprocedure orders may include administration of IV fluids to help to "flush" the dye through the kidneys. Adequate intake of fluids should be provided as well. Monitoring intake and output and renal function studies is indicated postprocedure [34,233].
During PCI, it is possible for parts of plaque to break off and travel, lodging in cerebral circulation. Patients should be monitored for any change in mental status or abrupt development of any transient ischemic attack-like symptoms [34,233].
Patient K underwent successful PCI to a branch of his circumflex artery, with placement of a drug-eluting stent. Following the procedure, he was transferred to the coronary care unit for observation and monitoring. He was placed on continuous ECG monitoring, which assessed ST-segment changes in the most appropriate leads. Vital signs were checked frequently, and the right femoral site and right pedal pulse were assessed for bleeding, signs of hematoma, or disrupted circulation. The patient remained on bed rest per orders. Laboratory tests were sent at prescribed intervals to monitor cardiac biomarkers and complete blood count. Patient K was also monitored for signs of recurrent ischemia, including recurrent chest pain and recurrent or new ST-wave changes.
Patient K recovered from the PCI. During the postprocedure period, it was noted that his groin site was dry, with no evidence of bleeding or hematoma. His pedal pulse remained strong and readily palpable. His vital signs were stable. The blood pressure measurement remained around 130 mm Hg systolic, and the patient remained chest pain free. ECG showed no further ischemic changes. His initial post-PCI complete blood count showed a slight drop in platelet count, and the initial post-PCI biomarkers showed his elevated levels starting to trend down. The follow-up laboratory results eight hours later showed his platelet count unchanged and his biomarkers continuing to trend downward. Patient K was discharged uneventfully 24 hours later.
Sometimes referred to as "clot-busting drugs," fibrinolytic agents have the potential to open an infarct-related vessel by dissolving existing thrombi. Fibrinolytic agents degrade fibrin clots by converting plasminogen to plasmin. The benefit of fibrinolytic therapy is its potential to establish reperfusion quickly. Re-establishment of coronary blood flow within the first 30 minutes after occlusion can abort infarction [234]. Reperfusion within 30 minutes to 2 hours can salvage myocardial tissue substantially, and fibrinolytic therapy administered within this timeframe has reduced mortality [235].
Although the focus of treatment for patients presenting with STEMI is often given to PCI, fibrinolytic therapy is the treatment of choice for some patients. If a patient arrives at or is transported by EMS to a non-PCI-capable facility, the decision whether to immediately transfer to a PCI-capable facility or administer fibrinolytic therapy must be made. Factors that affect this decision include the time from onset of symptoms, the risk of complications related to STEMI, the risk of bleeding with fibrinolysis, the presence of shock or severe heart failure, and the time required for transfer to a PCI-capable hospital. The ACCF/AHA guideline recommends that, in the absence of contraindications, fibrinolytic therapy should be given to patients with STEMI and onset of ischemic symptoms within the previous 12 hours when it is anticipated that primary PCI cannot be performed within 120 minutes of first medical contact [2].
Prehospital fibrinolytic therapy may reduce the time delay from symptom onset to treatment and can be administered by a trained EMS unit either with a physician on board or with a hospital-based physician in direct contact. A meta-analysis (six randomized controlled trials) showed a 60-minute reduction in time from symptom onset to treatment with prehospital compared to hospital-based initiation of fibrinolytic therapy [236]. Data from several trials indicate that prehospital fibrinolytic therapy may lower STEMI mortality rates and is considered to be of particular benefit in rural areas [236].
Four fibrinolytic agents have been evaluated and approved in the STEMI setting: tenecteplase, reteplase, alteplase (tPA), and streptokinase (Table 11) [2]. Of these agents, only streptokinase is non-fibrin-specific, and a fibrin-specific agent is preferred [2]. Each agent is associated with risks and benefits, and the choice of an agent is based on several factors, including preferences in the hospital formulary, cost, ease of administration, and the possibility of subsequent PCI. Although streptokinase is the least expensive agent, it is rarely used and no longer marketed in the United States because it has been shown to be less effective than the other three drugs [2].
COMPARISON OF FIBRINOLYTIC AGENTS FOR TREATMENT OF STEMI
| Characteristic | Streptokinase | Alteplase | Reteplase | Tenecteplase | |||
|---|---|---|---|---|---|---|---|
| Dose | 1.5 MU | Up to 100 mg | 10 U + 10 U | 30–50 mg | |||
| Administration | Infusion (over 30 to 60 minutes) | Bolus and infusion (over 90 minutes) | Bolus (over 2 minutes) given 30 minutes apart | Bolus | |||
| Weight-based dosing | No | Yes | No | Yes | |||
| Antigenic | Yes | No | No | No | |||
| Patency ratea | 60% to 68% | 73% to 84% | 84% | 85% | |||
| Fibrin specificityb | No | Yes (++) | Yes (++) | Yes (++++) | |||
| |||||||
Alteplase is inconvenient to administer, as it must be given as an initial intravenous bolus over 30 minutes followed by 60 minutes of infusion [2,237]. Reteplase and tenecteplase have both been compared with alteplase. Both have resulted in similar mortality as alteplase, and reteplase has led to better total patency rates or complete perfusion. [238,239,240]. TIMI 3 flow at 90 minutes has been similar for tenecteplase and alteplase [241]. The use of alteplase has thus declined because of the availability of these more convenient drugs with similar or improved outcomes [237].
The most common complication of fibrinolytic therapy is major bleeding, which occurs in approximately 5% to 6% of patients [221]. According to one systematic review and meta-analysis, tenecteplase-based regimens are associated with lower risk of major bleeding compared with other regimens [242]. Adverse outcomes after fibrinolytic therapy are generally more common among women and older patients [240,243]. Many instances of bleeding can be traced to incorrect dosing, particularly with weight-based agents [237]. In addition, patients who receive an improperly high dose of fibrinolytic agents have increased 30-day mortality.
Repeat fibrinolytic therapy after failed fibrinolytic therapy has not led to significant clinical improvement in terms of all-cause mortality or nonfatal reinfarction and has been associated with an increased risk for bleeding [244]. Rescue PCI is the preferred strategy for failed fibrinolytic therapy, as it has been shown to offer benefit when compared with repeat fibrinolytic therapy [244,245,246,247].
Another factor in selecting a reperfusion approach is whether the patient has contraindications to fibrinolytic therapy. Regardless of timing, PCI should be strongly considered for patients who are at high risk for bleeding complications, especially intracranial hemorrhage. There are several absolute and relative contraindications to fibrinolytic therapy; absolute contraindications include a history of intracranial hemorrhage or of substantial closed head or facial trauma within the past 3 months, suspected aortic dissection, or active bleeding (Table 12) [2]. Relative contraindications include history of poorly controlled hypertension, recent internal bleeding, and oral anticoagulant therapy [2].
CONTRAINDICATIONS AND CAUTIONS FOR FIBRINOLYSIS USE IN ST-ELEVATION MYOCARDIAL INFARCTION (STEMI)a
| Absolute Contraindications | ||||||||||||
| ||||||||||||
| Relative Contraindications | ||||||||||||
| ||||||||||||
|
Immediately following reperfusion with fibrinolytics, the patient is at risk to develop serious bleeding episodes or to reocclude the infarct-related vessel [34,227]. Nursing assessment during this period is crucial and should include [34]:
Continuous ECG monitoring for rate, rhythm, or reoccurrence of signs of acute ischemia, development of life-threatening arrhythmias
Assessment for reoccurrence of chest pain or other symptoms associated with an acute ischemic episode
Frequent vital sign monitoring for hypotension, drop in oxygen saturation, or other signs indicative of developing heart failure
Assessment for any changes in level of consciousness
Assessment for indications of bleeding
In addition, explanations about the patient's care and progress should be provided to the patient and the patient's family.
As described, a STEMI-associated thrombus consists of a fibrin-rich core and a platelet-rich cap. Because of this, both antiplatelet and anticoagulant therapies play important roles in supporting reperfusion therapy by helping to maintain patency of the infarct-related artery and preventing reocclusion [2].
Clopidogrel and Aspirin
Recommended antiplatelet therapy has traditionally involved aspirin and clopidogrel. Both the 2013 ACCF/AHA guideline for STEMI and the 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy include a recommendation for clopidogrel (75 mg per day for at least 14 days and up to one year) to be added to aspirin (81 mg/day [range, 75–100 mg]) for patients with STEMI, regardless of whether reperfusion with fibrinolytic therapy has been initiated [2,248]. Although prasugrel has been approved by the FDA for use in patients with STEMI and may be incorporated into the supportive treatment of these patients in place of clopidogrel, it is no longer recommended for use as an adjunct to fibrinolytic therapy [2,248].
Glycoprotein IIb/IIIa Inhibitor
A glycoprotein IIb/IIIa inhibitor may also be considered as an ancillary agent for patients who receive fibrinolytic therapy. The 2013 ACCF/AHA guideline for STEMI notes that the use of a glycoprotein IIb/IIIa inhibitor (abciximab, tirofiban, or eptifibatide) is reasonable at the time of primary PCI for selected patients with STEMI; routine use is not recommended [2].
Three meta-analyses of randomized trials that support this recommendation involved a comparison of glycoprotein IIb/IIIa inhibitors in patients with STEMI who had primary PCI. In each case, there was no significant difference in 30-day mortality, reinfarction, TIMI flow grade 3, or ST-segment resolution among the agents [249,250,251].
Heparin, Fondaparinux, Enoxaparin, or Bivalirudin
Anticoagulant therapy is associated with bleeding complications, so care must be taken in selecting an appropriate agent, with attention paid to the patient's renal function status, the time to an invasive procedure, and overall bleeding risk [252]. Unfractionated heparin, enoxaparin, and fondaparinux are the recommended anticoagulant agents based on studies demonstrating their efficacy [2]. The 2013 ACCF/AHA guideline recommends bivalirudin as an acceptable anticoagulant for primary PCI or for patients undergoing rescue PCI for failed fibrinolysis. Bivalirudin may be useful as a supportive measure for patients undergoing PCI either with or without prior treatment with unfractionated heparin and is particularly useful if patients develop heparin-induced thrombocytopenia and still require anticoagulation [2]. Anticoagulation should be continued for the duration of the index hospitalization (up to eight days) or until revascularization. Enoxaparin is recommended over unfractionated heparin when anticoagulant therapy will extend beyond 48 hours [2].
Unfractionated heparin should be used for patients with severe impairment of renal function, and unfractionated heparin or enoxaparin may be used for patients who are at increased risk of bleeding and who are likely to have early angiography [252]. Researchers reviewed data on 20,479 patients to compare outcomes for unfractionated heparin and enoxaparin [253]. Significantly fewer patients in the enoxaparin group had subsequent PCI within 30 days after fibrinolytic therapy [253]. There were no differences between the two agents with respect to major bleeding in this study, whereas a 2012 meta-analysis found enoxaparin to be superior to unfractionated heparin in reducing the incidence of major bleeding [254].
Fondaparinux may also provide benefit for patients who receive fibrinolytic therapy [252]. In one trial, 12,092 patients with STEMI were randomly assigned to fondaparinux (2.5 mg once daily for up to eight days) or to placebo. Analysis of a subgroup of 5,436 patients who received fibrinolytic therapy (primarily streptokinase) showed that fondaparinux was associated with significantly lower rates of death or nonfatal MI at 30 days and severe bleeding, yielding a significant overall benefit [252]. As noted, an additional anticoagulant (with anti-IIa activity) should be used in addition to fondaparinux when PCI is to be done after fibrinolytic therapy, and fondaparinux should not be used when creatinine clearance is less than 30 mL/min [2].
Despite the clear benefit of reperfusion, a significant percentage of eligible patients with STEMI do not receive reperfusion therapy and some are mistakenly considered "ineligible" [221,222,235,255]. One study of 8,578 STEMI patients found that more than 7% of all individuals with no contraindications to reperfusion were not given fibrinolysis or PCI [256]. Patients who are less likely to receive reperfusion therapy are older than 65 years of age, are female, have an atypical clinical presentation, and have a history of cardiovascular disease [221,256,257]. Another study found that 45% of eligible patients with diabetes on dialysis were not treated with reperfusion because they were mistakenly considered ineligible [2]. Compared with in-hospital mortality rates for patients who do receive therapy, the mortality rates are substantially higher for patients who are eligible for reperfusion but do not receive it, and rates have been higher and more discrepant for women, older patients, and patients with prior congestive heart failure, MI, or CABG surgery (Table 13) [235,255,256,258].
IN-HOSPITAL MORTALITY RATES FOR PATIENTS WITH ST-ELEVATION MYOCARDIAL INFARCTION (STEMI) BASED ON REPERFUSION THERAPY STATUS
| Population | No Reperfusion | Reperfusion | ||
|---|---|---|---|---|
| TIMI 9 (1994) | 18.9% | 10.5%/7.6%a | ||
| NRMI (2000–2003) | ||||
| All patients | 14.9% | 5.7% | ||
| Women | 17.9% | 9.3% | ||
| Older patients (>65 years of age) | 18.9% | 10.5% | ||
| ||||
Patients with no contraindications to reperfusion should be selected for primary PCI or fibrinolysis. Patients who lack access to PCI or have absolute contraindications to fibrinolysis should receive antithrombotic therapy in the hope of restoring TIMI grade 3 flow to the occluded vessel and preventing complications [150]. Older ACC/AHA guidelines for STEMI included recommendations for the treatment of patients who do not receive reperfusion therapy, including administration of aspirin, clopidogrel, and anticoagulants (low-molecular-weight heparin or fondaparinux rather than unfractionated heparin) to be given for the duration of hospitalization [259]. The 2013 guideline for STEMI does not include a specific recommendation for the treatment of patients who do not receive reperfusion therapy [2]. Despite this, it may be reasonable to administer the additional recommended medications (in the absence of contraindications) in these patients [248].
Acting on the theory that late revascularization of an infarct-related artery may improve left ventricular function and survival, some researchers have explored the value of late PCI for patients who have not had reperfusion therapy. However, the results of such studies have shown that elective PCI of an occluded infarct-related artery 3 to 28 days after MI offered no incremental benefit (beyond optimal medical therapy) for stable patients. The ACCF/AHA guideline for STEMI includes a recommendation that PCI of a totally occluded infarct-related artery more than 24 hours after STEMI should not be done in asymptomatic, stable patients with one- or two-vessel disease [2].
Although PCI is performed more frequently, several situations call for the use of CABG. The ACCF/AHA guideline for STEMI and the ACC/AHA guideline for CABG surgery recommend emergent or urgent CABG when PCI has failed, for coronary anatomy not amenable to PCI, and at the time of surgical repair of a mechanical defect (e.g., ventricular septal, papillary muscle, free-wall rupture) [2,6].
CABG results in a longer average recovery time and hospital stay compared with PCI (9.2 days and 3.2 days, respectively), and the in-hospital mortality is higher for CABG than for PCI (5.0% to 6.0% and 3.0% to 3.5%, respectively) [258]. However, long-term outcomes, including survival, have been similar for the two procedures. The mortality risk associated with emergent or urgent CABG is greater than that for elective CABG [100]. In addition, there is an increased risk of bleeding associated with clopidogrel and prasugrel given within five to seven days before CABG [100]. Thus, when CABG is planned, clopidogrel should be withheld for at least five days (seven days for prasugrel) unless the urgency for the procedure outweighs the increased risk for bleeding [2,6]. P2Y12 inhibitor therapy should be resumed postoperatively [248]. The use of CABG should follow the ACC/AHA guideline for this procedure [5].
Exercise testing in patients with STEMI is useful for risk stratification and assessment of functional capacity and should be performed to assess the presence and extent of inducible ischemia in patients who have not had angiography and do not have high-risk features [2]. The optimum time to exercise testing after STEMI has not been clearly defined. Exercise testing before discharge can provide reassurance to patients about their functional capacity and can also be used to establish exercise parameters for cardiac rehabilitation [2]. On the other hand, deferring exercise testing until three weeks after discharge in clinically low-risk patients appears to be safe and reasonable [2]. The ACCF/AHA guideline for STEMI suggests that exercise testing should be done before discharge in patients who may be candidates for a revascularization procedure and who have not undergone coronary angiography [2]. The use of exercise testing and the interpretation of its results should follow the guideline developed for this modality [154].
Echocardiography is also recommended for assessing left ventricular function in patients with STEMI who have not had coronary angiography and can be useful for evaluation of right ventricular infarction in patients with inferior STEMI and initial nondiagnostic findings [2]. Patients who have baseline abnormalities that may compromise interpretation of the ECG findings should have stress echocardiography (or myocardial perfusion imaging) to assess inducible ischemia [2]. Echocardiography and stress echocardiography should be performed according to guidelines or criteria developed for their use [260].
In addition to either catheter-based or pharmacologic reperfusion, treatment of patients with STEMI involves the use of some of the same general care principles (such as those regarding bed rest and the use of oxygen) and drugs as those recommended for patients with NSTE-ACS. Adjuvant therapy involves the use of dual-antiplatelet therapy, nitroglycerin, morphine, beta blockers, ACE inhibitors, calcium-channel blockers, and statins; the drugs used depend on whether the patient is treated with PCI or fibrinolytic agents [2].
The 2013 ACCF/AHA guideline for the management of STEMI recommends aspirin at a dose of 162–325 mg as a loading dose before either PCI or fibrinolytic therapy [2]. A P2Y12 inhibitor is used along with aspirin as dual-antiplatelet therapy. For patients treated with PCI, clopidogrel (600 mg), prasugrel (60 mg), or ticagrelor (180 mg) should be given as a loading dose as early as possible or at the time of the PCI [2]. Treatment with a P2Y12 inhibitor is continued for one year. Clopidogrel is the recommended P2Y12 inhibitor to support fibrinolytic therapy; a loading dose of 300 mg is used for patients 75 years of age or younger, and no loading dose is used for patients older than 75 years of age [2]. Treatment with clopidogrel is continued for at least 14 days and up to one year.
The benefit of nitroglycerin for patients with STEMI has been modest, but the drug can be given sublingually (0.4 mg every five minutes up to three doses) for persistent or recurrent ischemic discomfort [2]. The use of nitroglycerin should not preclude the use of other drugs that have been shown to have more benefit, such as ACE inhibitors.
The drug of choice to manage the pain associated with STEMI is intravenous morphine sulfate [2]. Morphine is indicated to relieve ongoing ischemic discomfort, control hypertension, ameliorate anxiety, or manage pulmonary edema. The initial dose should be 4–8 mg, with lower doses in the elderly. Additional doses of 2–8 mg may be given at intervals of 5 to 15 minutes [2].
The use of beta blockers has been an established recommendation for patients with STEMI because of the drugs' association with lower mortality [2]. The recommendation was modified in the 2007 focused update of the ACC/AHA guideline because of safety issues related to the use of intravenous beta blockers in conjunction with fibrinolytic therapy as well as emerging data on a lack of survival benefit [259]. The findings were confirmed in the 2013 ACCF/AHA guideline, and it is still recommended that oral beta blockers be used within the first 24 hours, except for those subsets of patients at high risk for complications with use of beta blockers [2]. Beta blockers should not be used in patients with signs of heart failure, evidence of a low output state, increased risk of cardiogenic shock, or other relative contraindications to beta blockade.
The use of an oral ACE inhibitor is a strong recommendation for all patients recovering from STEMI, including those with anterior infarction, pulmonary congestion, or LVEF of less than 0.40, as well as those with normal LVEF in whom cardiovascular risk factors are well controlled [2]. Adherence to this recommendation has increased since the late 1990s but remains low [190,261,262,263]. In addition, the doses used in clinical practice have been lower than the target doses used in clinical trials [263].
A meta-analysis of several major trials (more than 100,000 patients) demonstrated that use of an ACE inhibitor was associated with a significant overall odds reduction in mortality of 6.5% [264]. Early treatment is optimal, as reductions in mortality have been greatest within the first five days after the MI [264,265]. The ACCF/AHA guideline for STEMI notes that it is preferable to initiate treatment with an ACE inhibitor within 24 hours [2]. Treatment should start at a low dose that is gradually increased to a full dose within 24 to 48 hours.
ACE inhibitors are of most benefit for patients who are 55 to 74 years of age, have had an anterior infarct, or have a heart rate of at least 80 beats per minute [266]. Contraindications include a systolic blood pressure of less than 100 mm Hg (or more than 30 mm Hg below baseline), the presence of clinically relevant renal failure, a history of bilateral stenosis of the renal arteries, or known allergy. Patients who cannot tolerate an ACE inhibitor should be treated with an ARB [2].
Early treatment with dihydropyridine calcium antagonists (nifedipine and nicardipine) has not been found to improve rates of mortality or reinfarction [2]. Nifedipine is contraindicated in the treatment of STEMI. Although verapamil and diltiazem may be useful to relieve ongoing or recurrent ischemia, lower blood pressure, or control the ventricular response rate to atrial fibrillation when beta blockers are contraindicated (and the patient has well-preserved left ventricular function and no clinical evidence of congestive heart failure or pulmonary congestion), no specific recommendation for their use exists in the 2013 STEMI guideline [2,3]. Both drugs have been associated with significantly reduced mortality and major cardiovascular events [267,268]. Verapamil should not be used for patients with heart failure or bradyarrhythmias, and diltiazem should not be used for patients with left ventricular dysfunction [2].
Appropriate discharge planning and secondary prevention measures are essential, as the morbidity and mortality after UA/NSTEMI or STEMI are high (Table 14). A multidisciplinary team should be involved in preparing the patient for discharge, and detailed discharge instructions should be given to both the patient and family [2]. Discharge instructions should be easily understood, culturally sensitive, given in the patient's preferred language, and reinforced with written instructions. Instructions should include detailed information on the comprehensive care plan, including [2,3]:
Scheduling the first follow-up visit
Returning to normal activities (e.g., driving, work, physical/sexual activities)
Recommended secondary prevention measures
Medication dosing, frequency, and adherence
Plans to obtain prescribed medications immediately after discharge
Referral to cardiac rehabilitation
Exercise-based cardiac rehabilitation and secondary prevention programs have been shown to reduce repeat hospital admissions and improve health-related quality of life and function [269,270]. Referral to a cardiac rehabilitation or secondary prevention program is a recommendation in the ACC/AHA guidelines for NSTE-ACS and STEMI [2,3].
Substantial evidence has demonstrated that aggressive risk-reduction therapies enhance patient outcomes after ACS, and the 2014 AHA/ACC guideline for NSTE-ACS, the 2013 ACCF/AHA guideline for STEMI, and the 2011 update of the AHA/ACCF Secondary Prevention and Risk Reduction Therapy for Patients With Coronary and Other Atherosclerotic Vascular Disease guideline have made several recommendations for secondary prevention focusing on lifestyle modifications and medications.
After an ACS event, patients should address modifiable risk factors associated with atherogenesis by changing certain behaviors. Lifestyle modifications will include improvements in diet and physical activity levels, smoking cessation, blood pressure control, lipid management, and diabetes management [2,271]. Clinicians should involve other healthcare professionals in helping patients to achieve goals and should reinforce patients' positive efforts toward reaching these goals.
Smoking Cessation
Quitting smoking has been described as "probably the most important thing a smoker with acute MI can do to improve future health" [272]. Mortality after an ACS event for a patient who smokes cigarettes is twice that for a patient who does not, but cessation of smoking reduces reinfarction and death rates at one year [2]. Clinicians should use the in-hospital period after MI and each office visit as an opportunity to ask patients who were smokers if they have quit or are ready to quit and should offer counseling, pharmacologic support, and information on formal quit programs. The in-hospital period is unique because many patients are motivated to quit and are typically unable to smoke for three to nine days. Randomized controlled trials have shown that repeated contacts during the hospital stay and at and beyond three months (typically by telephone) are more likely to result in smoking cessation [2]. A Cochrane review showed that only intensive counseling programs work and that nicotine replacement further increases the rates of successful cessation among patients in intensive programs [273]. Another Cochrane review found high-quality evidence for a benefit of combined pharmacotherapy (with any type of nicotine-replacement therapy, bupropion, nortriptyline, or varenicline) and behavioral treatment compared with usual care, brief advice, or less intensive behavioral support [274]. However, many clinicians are reluctant to add another drug to the multitude of medications prescribed after MI.
Diet
Obesity is another well-documented risk factor for CHD, and weight management programs and information on healthy eating/caloric intake should be promoted as appropriate [271]. The patient's body mass index and waist circumference should be measured at each visit. The goal is to attain a body mass index of 18.5–24.9 and a waist circumference of no greater than 35 inches (women) or 40 inches (men) [271]. When weight reduction is needed, the initial goal is weight loss of 5% to 10% from baseline [271].
Exercise
The level of exercise should be prescribed according to risk, previous level of exercise, and possibly the results of a stress test [271]. The minimum goal is 30 minutes of aerobic exercise (e.g., walking, cycling, jogging) five times per week, with an optimal goal of 30 to 60 minutes every day [271]. Resistance training two times per week is reasonable to prescribe. Patients should also be encouraged to increase their routine daily activities (such as house cleaning and gardening).
Four classes of medications are recommended after an ACS event: antiplatelet/anticoagulant agents (aspirin, warfarin, and a P2Y12 inhibitor), beta blockers, ACE inhibitors (or ARBs), and lipid-lowering agents [2,3,146,271]. Treatment with these four classes has been associated with one-year mortality that is significantly lower than that for patients treated with none or one of the medications, with a positive impact most apparent at 24 months postdischarge, regardless of revascularization therapy [274,275]. In addition, nitroglycerin should be prescribed for all patients, and they should be instructed on its use for ischemic pain [2]. The medication profile should be tailored to each patient on the basis of the in-hospital events and procedures, risk factors, and drug tolerability.
Antiplatelet/Anticoagulant Agents
The recommended antiplatelet therapy after discharge is a combination of aspirin and a P2Y12 inhibitor (clopidogrel, prasugrel, or ticagrelor) [2,146,271]. The findings of studies have suggested that lower doses of aspirin (≤100 mg daily) are as effective as higher doses but have a better safety profile [180,245,248,276]. The recommended daily dose of aspirin is 75–100 mg for all patients, and the ACC/AHA guidelines for the management of STEMI and NSTE-ACS and duration of dual antiplatelet therapy state that it is reasonable to use an 81-mg dose [2,3,146,245,248]. However, despite the better safety profile of low-dose aspirin, data have indicated that 325 mg is the most common dose, prescribed for 55.7% of patients with UA/NSTEMI [277].
The addition of clopidogrel to aspirin as maintenance therapy has been found to enhance outcomes for patients [245]. Among 12,562 patients with ACS who were taking aspirin (at a dose of 75–325 mg daily) in one trial, one year of treatment with clopidogrel was associated with a lower rate of a composite endpoint of cardiac death, MI, or stroke, regardless of the aspirin dose [245]. Clopidogrel was also associated with an increased risk for major bleeding, but bleeding risks increased with increasing aspirin dose, with or without clopidogrel [245].
The 2013 update of the ACCF/AHA guideline for the management of STEMI and the 2016 guideline focused update on duration of dual antiplatelet therapy include recommendations for maintenance therapy with a P2Y12 inhibitor [2,248]. The guidelines indicate that patients with a stent should be treated with clopidogrel (75 mg daily), prasugrel (10 mg daily), or ticagrelor (90 mg twice a day) for at least one year [2,248]. Patients not receiving a stent should receive clopidogrel (75 mg daily); it is reasonable to prescribe prasugrel (10 mg daily) in patients not receiving a stent and without a history of stroke or transient ischemic attack [2,248].
Questions about clopidogrel maintenance therapy remain, as the optimal dose and duration of therapy have not been identified [146,183,278,279]. Another concern is the effect of stopping clopidogrel. In a 2008 study of 3,137 patients with ACS (treated either medically or with PCI) who took clopidogrel for a mean of 9 to 10 months, there was a significantly high risk of adverse events in the initial 90 days after stopping treatment with clopidogrel [280]. The reason for this phenomenon is unclear, and the authors suggested that strategies to reduce the incidence of such early events should be identified [280]. Additionally, the response to clopidogrel varies among patients, and diminished responsiveness has been observed [146]. A 2010 retrospective study of 2,017 patients with ACS, conducted to confirm the findings of the 2008 study, found that the 0- to 90-day interval after stopping clopidogrel was associated with higher risk of death/MI compared with the 91- to 360-day interval. There was a similar trend of increased adverse events 0 to 90 days after stopping clopidogrel for various subgroups (i.e., women versus men, medical therapy versus PCI, stent type, and ≥6 months or <6 months of clopidogrel treatment) [281]. Warfarin is recommended as an antithrombotic for patients with UA/NSTEMI or STEMI who are allergic to aspirin [146,271].
Antiplatelet therapy is preferred over anticoagulant therapy with warfarin (or other vitamin K agonists) for treating patients with atherosclerosis [271]. However, warfarin therapy is reasonable for patients with a prosthetic heart valve, persistent or paroxysmal atrial fibrillation, a documented left ventricular thrombus, concomitant venous thromboembolic disease, or other indication. Warfarin should be given to maintain a specific international normalized ratio (INR) depending on the use of stents, underlying cardiac disease, and the concomitant use of clopidogrel [271]. The risk of bleeding is increased when warfarin is used in conjunction with aspirin and/or clopidogrel, and patients treated with the three medications should be monitored closely [271].
Beta Blockers
Treatment with oral beta blockers is recommended for all patients after UA/NSTEMI or STEMI [2]. Treatment should continue indefinitely.
ACE Inhibitors or ARBs
An ACE inhibitor is also recommended as long-term therapy after UA/NSTEMI or STEMI [2,271]. ARBs should be used for patients who are unable to tolerate an ACE inhibitor and have clinical or radiographic signs of heart failure or a left ventricular ejection fraction of less than 40% [2].
Lipid-Lowering Agents
Even before the advent of statins, reducing lipid levels through diet and previously available medications led to significant reductions in MIs. Statins are now the preferred medications for lipid-level management, and several studies have demonstrated their effectiveness in reducing atherogenesis. A fasting lipid profile should be determined within 24 hours after admission, and statin therapy should begin during hospitalization, regardless of this baseline level [2]. Intensive statin therapy appears to be of benefit for patients with recent ACS (but not for patients with stable CHD). In a pooled analysis of data on more than 8,600 patients, intensive statin therapy significantly reduced all-cause mortality compared with standard therapy [282]. This benefit was confirmed in an analysis of data from a total of six trials (28,505 patients), with all-cause mortality at two years of 3.5% for intensive therapy compared with 4.6% for standard therapy [283]. A meta-analysis of 20 trials involving 8,750 patients with ACS undergoing PCI found a time-related benefit to the start of statin therapy. By meta-regression, earlier statin administration correlated significantly with lower risk of MI, major adverse cardiac events, and major adverse cardiac and cerebrovascular events [284].
The 2013 ACCF/AHA guideline for STEMI indicates the need to continue or initiate the use of a statin to manage patients' lipoprotein levels [2]. In particular, the guideline makes a sole recommendation for high-dose atorvastatin (80 mg daily), based primarily on results of the Pravastatin or Atorvastatin Evaluation and Infection Therapy–Thrombolysis in Myocardial Infarction 22 (PROVE IT-TIMI 22) trial. Rates of cardiovascular events did not significantly decrease with tiered simvastatin (40 mg for one month, then 80 mg thereafter), and there are concerns about the safety of the 80-mg dose [2]. The compliance rate of statins may be improved when therapy is initiated before discharge following STEMI.
The goal of statin therapy is to achieve an LDL level less than 100 mg/dL for patients with average risk, and an LDL level of less than 70 mg/dL is reasonable for high-risk patients [2]. If the triglyceride level is 200 mg/dL or higher, the non-HDL cholesterol should be less than 130 mg/dL in patients with average risk, whereas a non-HDL cholesterol level of less than 100 mg/dL is reasonable for very-high-risk patients. Statin therapy should be supplemented with dietary modification, weight management, and exercise. Patients should be encouraged to follow a diet with an increase of fresh fruits and vegetables, with less than 7% of total calories as saturated fat, less than 1% of total calories as trans fatty acids, and less than 200 mg per day of cholesterol [2,271].
If statin therapy fails to control lipid levels or patients do not tolerate statins, treatment with non-statins, such as ezetimibe or PCSK9 inhibitors, may be considered [271,285].
After discharge, patients may need other treatments to manage blood pressure, depression, or diabetes.
Control of Blood Pressure
In addition, blood pressure should be controlled according to the 2017 Guideline for High Blood Pressure in Adults, which recommends treatment when blood pressure is elevated, defined as 120–129/<80 mm Hg [67]. The guideline recommends initial treatment with nonpharmacologic interventions and lifestyle changes. Initiation of pharmacologic treatment is recommended for secondary prevention in patients with clinical cardiovascular disease and an average systolic blood pressure of 130 mm Hg or greater or an average diastolic blood pressure of 80 mm Hg or greater and for primary prevention in adults with an estimated 10-year atherosclerotic cardiovascular disease risk of 10% or higher and an average systolic blood pressure of 130 mm Hg or greater or an average diastolic blood pressure of 80 mm Hg or greater [67]. The AHA/ACCF recommends initial treatment with a beta blocker and/or an ACE inhibitor as secondary prevention for patients with CHD [271].
Treatment of Depression
An ACS event can be distressing for many patients, leading to a heightened fear of dying and anxiety about adjusting to life with cardiac disease [286]. These emotions can substantially affect a patient's psychosocial status and lead to depression [287,288]. Some degree of clinically significant depression has been reported to occur in up to half of patients with ACS, with major depression occurring in 15% to 20% of patients [288]. Depression has been found more often in women compared with men and in men with a history of MI [289]. In addition to the negative effect on the patient's quality of life, depression has also been shown to be associated with lack of adherence to secondary prevention measures and with increased mortality [287,290,291].
Evaluation of a patient's psychosocial status, with particular attention paid to signs of depression, is a recommendation in the ACCF/AHA guidelines for STEMI and UA/NSTEMI, and screening for depression and referral and/or treatment is a recommendation in the 2011 AHA/ACCF Secondary Prevention and Risk Reduction Therapy guideline [2,3,271]. At each visit, clinicians should ask patients about anxiety, sleep disorders, social support, and symptoms of depression. Cognitive behavior therapy and selective serotonin reuptake inhibitors (e.g., sertraline) may be useful for enhancing the quality of life for patients with symptoms of depression, though treatment does not directly improve cardiovascular disease outcomes [271,288].
Management of Diabetes
CHD is responsible for about 75% of deaths in individuals with diabetes, and more than 30% of patients with NSTE-ACS have diabetes [3]. It is now well known that a reduction in blood glucose levels is associated with improved outcomes in patients with diabetes or prediabetes who have experienced UA/NSTEMI or STEMI. This reduction may be achieved as the result of lifestyle changes (including weight management, physical activity, and medical nutrition therapy) or medication therapy [2,3,292]. The patient's primary care physician and/or endocrinologist typically handle the management of diabetes, but it is beneficial for treating physicians to coordinate with a primary care physician or specialist [271].
The goal of diabetes management (aside from reversal of the condition through intensive lifestyle change) is tight glycemic control, as both hyperglycemia and hypoglycemia have a profound impact on in-hospital and six-month mortality rates following a cardiac event [3]. Metformin has possible cardiovascular benefits and has historically been the criterion standard for most patients based on its established efficacy, safety, and cost. However, SGLT2 inhibitors (e.g., dapagliflozin, empagliflozin) or GLP-1 agonists (e.g., dulaglutide, liraglutide) should be considered first line for patients with type 2 diabetes and cardiovascular disease [236]. The intensity of blood glucose-lowering medications should be closely tailored to each patient's risk of hypoglycemia during treatment. It may be reasonable to initiate treatment with medications to achieve an HbA1c of 7% or less [271].
Despite the obvious benefit of secondary prevention strategies, physician adherence to guidelines and patient compliance with cardiac rehabilitation, medication regimens, and lifestyle change recommendations are suboptimal [271,272,293,294,295,296,297,298]. According to data from several studies, referrals to cardiac rehabilitation range from 64% to 87% by hospital (mean: 81%) [295]. Quality improvement initiatives have increased referrals. Rates of actual enrollment are more important than referral rates, however, and enrollment has been much lower than referral rates [295,296]. Only 29% of patients with MI who were referred to cardiac rehabilitation enrolled within one month of discharge; this rate raised to just 48.25% after six months [296]. Women are less likely to be enrolled after one month, as are patients with hypertension or peripheral arterial disease and uninsured patients. Older patients are less likely to have participated at six months, as are smokers and patients with economic hardship. White individuals and patients who attained a higher education level were more likely to enroll by six months [296].
Cardiac rehabilitation coordinators have identified several patient-related barriers to participation in rehabilitation programs as well as implementation of other evidence-based guidelines, including coming to terms with a diagnosis of heart disease, challenges in changing behavior, and cost [299]. Others have identified distance from a rehabilitation center (e.g., long travel time, lack of transportation) and high co-pays as significant barriers [296]. Efforts to improve rates of referral to cardiac rehabilitation should continue, and more research is needed to determine how to address barriers to enrollment.
Data have also indicated that rates of dietary change and smoking cessation in patients with ACS need improvement. Research shows that physicians are recommending dietary modification and smoking cessation to patients (91% and 95%, respectively), but rates of compliance are not optimal [272,297,300]. Smoking cessation rates following MI (roughly 30% at six months) are greater than in similar-age patients in the general population but are still too low [272].
Reasons provided for not adhering to dietary modification (and exercise) include not being able to see a physical change, and many individuals express that they are dissatisfied with having to make so many lifestyle changes at once [298]. However, the results of a 2014 study indicate that ACS patients who comply with nonsmoking, diet, and exercise plans have significantly lower mortality and recurrence of MI despite no change to their waist circumference [301]. Therefore, it is important that patients understand that the benefits of dietary modification are internal (not based on appearance) and that obtaining a regular lipid profile will show their progress.
With regard to medications, studies have shown that up to 57% of patients are not managed optimally, defined as receiving all four classes of medications [20,104,165,188,211,261,294,300]. Optimal medical therapy is less likely among older patients, women, and patients who had CABG during the index hospitalization, had previous heart failure, or had renal dysfunction [275,302,303].
The class I guideline recommendations for all secondary prevention strategies can be organized into a simplified "ABCDE" approach to help clinicians implement guideline-based care [304]:
A: Aspirin, antianginal agents, antiplatelet therapy, and ACE inhibitors (or ARBs)
B: Beta blockers and blood pressure control
C: Cardiac rehabilitation, cholesterol treatment, and cigarette smoking cessation
D: Diet, depression management, and diabetes management
E: Exercise and education
Critical pathways, protocols, and other quality improvement tools are valuable for helping to increase implementation of guidelines [20,305]. For example, the GWTG program helps to enhance compliance through a Web-based tool that provides online reminders about discharge management strategies. This tool can be used to send discharge instructions and information on medications to primary care clinicians [20,145]. The GWTG-Coronary Artery Disease program was implemented in 418 U.S. hospitals and was associated with widespread and prolonged adherence to evidence-based guidelines [305].
Lack of patient compliance with medications is also a serious problem and has been referred to as an unrecognized risk factor for CHD, because of its association with significant increases in adverse events and health costs [306,307]. Among individuals with CHD (many of whom had experienced a recent ACS event), compliance with guideline-recommended medications has ranged from 18% to 55%. Approximately 54% of individuals have been compliant with all of their initial medications, and compliance decreases over time [307,308,309]. One study showed that compliance was 60.3% at one year, 53.7% at two years, and 48.8% at five years [310]. Individuals who discontinue medications are more likely to be older, female, unmarried, and less educated [309]. Several other factors have been found to be associated with noncompliance with medications [307,308,309]:
Choice of medication
Tolerability
Duration of treatment
Dosing frequency
Higher number of prescribed medications
Lack of symptoms as indication for the medication
Uncertainty about how to take the medication
Lack of transportation to the pharmacy
Patient education is an integral component of treatment for patients with ACS and should begin during hospitalization and continue throughout follow-up care [2]. Adequate time for appropriate education during the index hospitalization has been challenged by shorter hospital stays and reduced staffing [311]. The responsibility of patient education has thus shifted to the healthcare team. Surveys have shown that nearly one-half of individuals are not knowledgeable about ACS-related symptoms or their level of risk, even after having an ACS event [311]. Men, older individuals, and individuals with less formal education were less likely to be knowledgeable about their risk and symptoms [311]. This lack of knowledge can contribute to lack of compliance with recommended secondary prevention strategies.
Research has shown that patient education should focus on the importance of [2,312]:
Recognition of symptoms
Timeliness of care
Acknowledgment of risk factors for ACS
Compliance with secondary prevention strategies
Education in these areas should be tailored to individuals, as perceptions of cardiac disease and risk differ across subgroups of patients according to age, gender, and race/ethnicity [137,312]. As noted, many healthcare professionals do not feel confident in their effectiveness in helping patients understand their disease and comply with preventive measures [313]. Table 15 provides a summary of strategies that nurses, physicians, and other healthcare team members can use to facilitate effective education with patients and families [314,315,316,317,318].
STRATEGIES FOR EFFECTIVE EDUCATION FOR ACS PATIENTS
|
Many individuals still believe that the onset of an MI will be "dramatic," with chest pain that is severe and crushing [2,283,319]. Among individuals who had an acute MI, 40% interpreted their symptoms as cardiac in nature [137]. In addition, chest pain and other ACS-related symptoms were interpreted differently by men and women. Men were more likely to think the symptoms were cardiac in nature if the chest pain was severe and if they had a history of CHD. In contrast, women did not relate severity of chest pain with a cardiac origin [137]. Healthcare professionals should talk to patients about the "real" signs and symptoms of ACS, emphasizing the diversity in symptoms [311,312].
On average, individuals wait 1.5 to 2 hours before seeking medical care for ACS-related symptoms, and this delay has not changed over time, despite many national public campaigns emphasizing the importance of timely care [2]. Furthermore, up to 50% of individuals with ACS-related symptoms are transported to the hospital by means other than emergency medical services, which can increase delays [2,283]. Individuals have given several reasons for delays in seeking medical care (Table 16) [283]. Individuals and their families or caregivers should be told that immediate action is needed for ACS-related symptoms, including calling emergency medical services, taking nitroglycerin for ischemic pain, and taking aspirin.
REASONS FOR DELAY IN SEEKING MEDICAL ATTENTION FOR CHEST PAIN
|
The need for better understanding of risk among individuals who have had ACS is evidenced by studies that have shown that perceptions of personal risk are lower than their actual risk [2,283,311,312,319]. Healthcare professionals should reinforce information about modifiable risk factors and provide patients with educational resources that describe risk factors and their effect on the potential for future events. Patients' individual risk factors should be discussed in an ongoing manner, with a focus on positive changes through lifestyle modifications and medications.
Compliance with prevention strategies can be enhanced by identifying the barriers for each individual patient and working together to address the problem. Primary care clinicians and other healthcare professionals should ask patients about medication compliance at each office visit and should emphasize the importance of maintaining drug therapy. Ongoing education about the benefit gained from medications as well as lifestyle modifications is vital to ensuring high compliance and low risk of adverse events.
Suboptimal adherence to guidelines for management and prevention of CHD contributes to increased ACS risk. Adherence has been less than effective, especially among patients at low risk for disease [2]. In one survey, primary care physicians, obstetricians/gynecologists, and cardiologists did not rate themselves as being effective in helping their patients to prevent CHD and manage risk factors. Of particular note is the percentage of respondents who were not aware that CHD leads to more deaths among women than among men; only 8% of primary care physicians, 13% of obstetricians/gynecologists, and 17% of cardiologists recognized this fact. Clinicians have noted several barriers to adhering to CHD prevention guidelines, including [2]:
Cost of medications
Lack of reimbursement, especially for lifestyle interventions
Lack of adequate time for counseling
Lack of patient education tools
Existence of multiple guidelines
Lack of knowledge and skills to recommend dietary changes and facilitate patient adherence
Efforts should be directed at alleviating these barriers to enable healthcare professionals to evaluate patients' risk factors adequately and to develop ways to help patients understand their risk and the importance of prevention strategies. A multidisciplinary team approach is needed to provide expertise in all areas. In addition, initiatives should emphasize the risk of CHD among women.
ACS represents the acute expression (recognition) of a chronic disease, one with pre-event possibilities for primary prevention and post-event need for secondary prevention and management strategies that restore and maintain health. Care of the patient with cardiovascular disease/ACS is challenging, the clinical issues are multifaceted and complex for the patient, the patient's family, and the practitioner alike. Patients with chronic disease are estimated to visit four to nine different healthcare professionals regularly; interprofessional collaboration is an effective way to share the load, facilitate care, and reinforce management goals [321]. Evidence shows that an interprofessional team approach enhances quality of care and improves outcomes for patients with complex illness and diverse needs [322].
Interprofessional practice and collaboration (IPC) is a model of care provided by healthcare professionals with overlapping expertise, who are committed to shared responsibility, mutual trust, and communication to achieve a common goal [322]. Increasingly, IPC is modeled in the context of medical education. The introduction of IPC to primary care and chronic disease management has been shown to foster patient-centered care and reduce healthcare costs [323,324].
Patient E is a man, 54 years of age, who presented to his primary care physician's office with complaints of chest pain. Upon arrival at the primary care physician's office, he was chest pain free. A 12-lead ECG was performed and showed no changes from previous ECGs. The patient's vital signs were found to be stable and within his normal range: blood pressure 135/78 mm Hg, heart rate 68 beats per minute and regular, and respirations 16 breaths per minute and unlabored. He was afebrile.
Comments and Rationale : Persons who present in any healthcare setting with a complaint of chest pain should be evaluated for the presence of signs and symptoms of ACS. Appropriate assessment measures include vital signs and a 12-lead ECG to assess for changes suspicious for ischemia or infarct. Patient E was chest pain free on arrival, his ECG did not show any acute ischemic changes, and his vital signs were stable. Further assessment by the healthcare provider is indicated.
The physician questioned Patient E about his chest pain episodes. The patient reported that, until about a week ago, he just had been having his "usual" occasional chest pain when he "worked too long, too hard in the yard." However, over the last week, his chest pain attacks had been lasting longer and requiring more sublingual nitroglycerin tablets for relief. The previous night he had experienced a prolonged episode of chest pain at rest and decided to seek medical attention.
Comments and Rationale : Chest pain that occurs in a predictable pattern, is generally triggered by the same level of exertion, and is readily relieved by rest and sublingual nitroglycerin can be classified as "stable angina." Stable angina is a hallmark symptom of CHD but is rarely indicative of acute myocardial ischemia. However, chest pain attacks that increase in frequency, severity, and/or require additional nitroglycerin tablets to achieve relief and severe chest pain that occurs at rest are indications that the patient's angina has become "unstable." Immediate medication evaluation and intervention is indicated.
The physician reviewed Patient E's medical record and noted that he had a history of CABG surgery five years previously. Two years ago, Patient E required placement of a drug-eluting stent to open a blockage in one of the saphenous vein grafts from his prior CABG surgery. Patient E was also prescribed medication for dyslipidemia; his most recent laboratory tests showed his LDL was borderline high at 135 mg/dL. He stopped smoking following the stent placement two years previously. The patient was approximately 30 pounds overweight. When the physician mentioned his need for weight loss, the patient's usual reply was, "It's either the weight or the smoking. I can't manage both."
Comments and Rationale : A careful history and physical can provide information necessary to triage patients who present with chest pain and stratify their risk for serious consequences such as acute MI. Major risk factors for ACS include a known history of CHD, history of occlusions that have required intervention to restore blood flow and oxygen supply, and the presence of modifiable risk factors such as obesity, dyslipidemia, smoking, and hypertension.
Given the patient's known CHD, previous history of CABG and PCI with stents, and his continuing risk factors, the physician instructed Patient E to go to the emergency department of the local hospital. The patient declined transport by emergency medical services and insisted on driving himself to the hospital.
Comments and Rationale : ACCF/AHA guidelines strongly recommend that persons with possible ACS be transported to the hospital by emergency medical services. Transport by emergency medical services provides the opportunity for skilled healthcare providers to assess the patient, obtain an immediate ECG, and administer aspirin and other therapies as indicated. In addition, emergency medical services can notify the receiving emergency department to expect the patient so immediate triage and evaluation are facilitated. ACCF/AHA guidelines strongly discourage persons with possible ACS from driving themselves or asking friends or family members for transport to the emergency department.
In the emergency department, Patient E developed an episode of chest pain. He rated the pain as 10 out of 10 and located the pain on the left side of his chest, substernal region. He was slightly diaphoretic with a blood pressure of 170/90 mm Hg and a heart rate of 110 beats per minute.
Comments and Rationale : Severe, intense chest pain located in the left substernal area of the chest coupled with diaphoresis and vital sign changes is a strong indicator of ACS.
The emergency physician activated the chest pain protocol. Patient E received 325 mg of aspirin with instructions to chew it before swallowing. He was also given sublingual nitroglycerin, and supplemental oxygen at 2 liters per nasal cannula was started. A 12-lead ECG was performed, and blood work, including troponin T level, were drawn.
Comments and Rationale : In ACS, aspirin is given immediately for its antiplatelet action to decrease the risk of thrombus formation. Sublingual nitroglycerin acts a vasodilator, reducing myocardial workload while increasing myocardial oxygen supply. It also helps to lower elevated blood pressure.
The 12-lead ECG showed non-specific ST-segment and T-wave changes. Five minutes after one sublingual nitroglycerin tablet, the patient reported that his chest pain was 10/10; his blood pressure was 140/88 mm Hg. A second sublingual nitroglycerin tablet was given; five minutes later, Patient E reported his pain was 8/10, and his blood pressure remained at about 140/88 mm Hg. A third sublingual nitroglycerin tablet was administered, and minutes later, the patient reported that his pain was 5/10. His blood pressure was measured as 132/80 mm Hg. The physician ordered 2 mg of morphine IV.
Comments and Rationale : In patients with clinical symptoms of ACS, nonspecific ST-segment and T-wave changes are worrisome. Serial ECGs may be indicated to identify the presence of an evolving MI. Sublingual nitroglycerin may be given every five minutes up to three doses if the patient does not become hypotensive. The goal of analgesic therapy in ACS is to get the patient "chest pain free." Morphine may be used to treat chest pain that does not resolve after three sublingual nitroglycerin tablets. Morphine acts as a vasodilator, decreasing myocardial oxygen demands and increasing myocardial oxygen supply.
After receiving morphine, Patient E reported that he was chest pain free. His blood pressure and heart rate returned to the "usual" level. His initial troponins were returned negative for cardiac damage. The physician made the decision to admit the patient to the telemetry/stepdown floor for further observation and monitoring. His admitting diagnosis was UA/possible ACS, and his admitting orders included orders for serial troponin monitoring, continuous ECG monitoring, and immediate 12-lead ECG with chest pain.
Comments and Rationale : The combination of Patient E's increasingly severe and frequent chest pain episodes coupled with the presence of nonspecific changes on 12-lead ECG and his previous history of CHD, CABG, and stent placements are indicators that the patient is at increased risk for MI. Serial troponins can provide important diagnostic information and may be used to confirm or rule out a diagnosis of NSTEMI. Continuous ECG monitoring provides information about ST-segment changes indicative of ischemia and infarct. A 12-lead ECG recorded during chest pain can also provide information about possible ischemia/infarction and what part of the heart is at risk.
Patient E's second set of cardiac biomarkers returned showing elevated troponin levels. A repeat ECG indicated no evidence of ischemia or infarct. A third set of cardiac biomarkers approximately eight hours later showed that troponin T was positive for myocardial damage. A diagnosis of NSTEMI was confirmed. Another ECG taken immediately after the return of the laboratory work did not show any evidence of ischemia; however, minutes later, Patient E developed chest pain. ST-segment depression in the inferior leads was noted on continuous ECG monitoring.
Comments and Rationale : ECG changes and cardiac biomarker elevation indicative of myocardial ischemia and infarction can develop over a period of minutes to hours. In persons who have persistent chest pain with initial negative ECG findings and cardiac biomarker levels, serial measurements are indicated. As was the case with Patient E, biomarker changes indicative of infarct may develop several hours after the initial episode of chest pain. Presence of elevated cardiac troponin levels, in the absence of ST-segment elevation, is diagnostic for NSTEMI.
The physician ordered a continuous heparin infusion along with a bolus dose of eptifibatide followed by a continuous infusion. Patient E had been administered aspirin in the emergency department; on the floor, he received 600 mg of clopidogrel along with a low dose of a beta blocker. Patient E developed another episode of chest pain that was not relieved by sublingual nitroglycerin or IV morphine. As a result, the physician ordered a continuous nitroglycerin drip.
Comments and Rationale : The immediate goal of treatment in NSTEMI is to relieve ischemia and prevent ongoing infarction. Key elements of management include aspirin (chewed) and clopidogrel to reduce platelet formation and aggregation, and nitroglycerin and morphine for relief of ischemic pain through reduction of myocardial workload and decrease in myocardial oxygen demand. Chest pain unrelieved by sublingual nitroglycerin may be treated with a continuous nitroglycerin infusion titrated to relieve chest pain and maintain a blood pressure within a prescribed range. A third major element in the management of acute NSTEMI is anticoagulation. A continuous heparin infusion is one option for anticoagulation; use of heparin may be combined with the use of a glycoprotein IIb/IIIa inhibitor. In acute stages of NSTEMI, a glycoprotein IIb/IIIa inhibitor such as eptifibatide may be used. Eptifibatide may be initiated prior to cardiac catheterization, and the infusion can be maintained for a specified period of time following catheterization and stent placement.
Patient E was taken to the cardiac catheterization laboratory for diagnostic coronary angiography and possible PCI. Cardiac catheterization revealed that he had an area of blockage in his right coronary artery. The patient's previous stent remained open, and the other vein grafts from previous surgery were also patent. A PCI with placement of a bare-metal stent was performed.
Comments and Rationale : Intracoronary stents are deployed during PCI to help to keep the lumen of the affected vessel open. The choice of type of stent (bare-metal or drug-eluting) is left to the interventional cardiologist performing the procedure.
Following recovery in the cardiac catheterization area, Patient E was returned to his room. The postcatheterization orders included instructions for bed rest for 4 hours, continuation of the eptifibatide drip for a total of 18 hours following the conclusion of the PCI procedure, and serial monitoring of cardiac biomarkers and complete blood count. Nursing care included continuous ECG monitoring, frequent vital sign checks, frequent monitoring of the arterial puncture site for evidence of bleeding or hematoma, and assessment for signs of recurrent chest pain (indicative of reocclusion of the infarct-related vessel) or severe left flank pain (indicative of retroperitoneal bleed). Patient E was encouraged to drink fluids, and his urine output was monitored and recorded.
Comments and Rationale : Key elements of care during the immediate post-PCI period include monitoring for bleeding, maintaining the eptifibatide drip as ordered to decrease the risk of stent occlusion, and monitoring the patient for changes in vital signs, heart rhythm, or the development of chest pain. Potential complications during this period include bleeding from the puncture site and reocclusion in the coronary artery.
Patient E's initial blood work following the PCI showed a drop in his platelet count from the high normal to borderline low range. A second set of blood work sent six hours later showed a dramatic and significant drop in his platelet count. The physician was notified and ordered the discontinuation of the eptifibatide infusion. Appropriate nursing interventions included close monitoring of the patient for any signs of bleeding.
Comments and Rationale : Use of glycoprotein IIb/IIIa inhibitors can cause an unsafe drop in platelet counts in some individuals. Careful monitoring of platelet levels at specified intervals during the infusion is indicated to identify this complication promptly and intervene in timely fashion.
Patient Z, a woman 63 years of age, presented to the emergency department with a complaint of intermittent epigastric and chest discomfort. She reported that the discomfort had occurred intermittently over the previous two to three weeks. When questioned, she admitted that she had felt more fatigued and had periods of shortness of breath and light-headedness over the same time period.
Comments and Rationale : While women may present with ACS symptoms similar to men, they may also present with symptoms labeled as "atypical." Epigastric pain, fatigue, and light-headedness have been identified as "atypical" symptoms associated with ACS.
At the time of presentation to the emergency department, Patient Z reported that she was experiencing no discomfort. Her blood pressure was elevated at 210/120 mm Hg, her heart rate was 84 beats per minute, her respirations were even and easy, and she did not appear to be in acute distress. An initial ECG showed no signs of acute ischemia or infarct but did reveal a pathologic Q wave. The initial cardiac troponin I returned indicating the level to be "borderline" but not yet elevated. When asked, Patient Z admitted that she has had high blood pressure "for a while" and that she does not always take her medications as prescribed.
Comments and Rationale : At the time of admission to the emergency department, Patient Z shows no signs of acute ischemia or infarct; she is chest pain free, her ECG shows no ST-segment elevation or ST-segment depression, and her initial cardiac troponin level is equivocal. However, she has at least one major risk factor for CHD and subsequent ACS: hypertension that appears poorly controlled. Her ECG also shows evidence (i.e., a pathologic Q wave with no evidence of ST-segment elevation or T-wave inversion) that she had experienced an MI sometime in the past.
The emergency department physician admitted Patient Z to the telemetry unit with hypertension and possible ACS/UA. Serial cardiac biomarkers remained essentially unchanged from the initial levels. Repeat 12-lead ECG eight hours after admission showed no indications of acute ischemia or infarct. Patient Z had several episodes of epigastric discomfort/chest discomfort following her transfer to the telemetry unit. She developed nausea and emesis with one episode. Sublingual nitroglycerin was effective in relieving her discomfort. Oral medications to lower her blood pressure were effective and subsequent measurements indicated a blood pressure of 150/88 mm Hg. When asked, the patient denied any history of a previous MI. When asked if a physician had ever instructed her to take a lipid-lowering medication, she replied that she "couldn't afford it."
Comments and Rationale : Risk stratification indicates that Patient Z has risk factors for CHD and ACS but is not currently experiencing an acute episode. An early conservative approach, including a stress test, is indicated.
The physician ordered a fasting lipid panel, to evaluate for dyslipidemia, and an exercise stress test.
Comments and Rationale : The focus of medical therapy for Patient Z will be on continued risk stratification and risk factor reduction. Exercise stress testing will provide information about presence of ischemic disease and risk for adverse cardiac events.
During the exercise stress test, Patient Z developed chest pain, diaphoresis, and nausea before reaching the targeted heart rate. She underwent a follow-up cardiac catheterization with placement of a stent in her right coronary artery. Following a conversation with the patient regarding adherence to dual antiplatelet therapy, the interventional cardiologist chose to implant a bare-metal stent.
Comments and Rationale : Inability to reach a heart rate target due to development of chest pain or other ischemia-associated symptoms during a stress test is an indication of ischemic disease and high risk for future ischemia and infarct. Cardiac catheterization is indicated; it provides direct visualization of coronary circulation and permits percutaneous intervention if indicated. Implantation of drug-eluting stents should generally be avoided in persons for whom adherence to dual antiplatelet therapy is unlikely.
Patient Z recovered uneventfully from the PCI. Her prescribed medications included simvastatin, metoprolol, hydrochlorothiazide, additional oral antihypertensive medications, her "usual" oral hypoglycemic medications, aspirin, and clopidogrel. Patient Z's fasting lipid panel showed an LDL level of 190 mg/dL and a total cholesterol of 250 mg/dL. The discharge nurse began planning for Patient Z's return home.
Comments and Rationale : Unless complications develop, patients only remain in the hospital 24 to 48 hours after PCI. Therefore, assessment of discharge needs and initial teaching should begin immediately.
The nurses caring for Patient Z noted that she was taking several medications that were new to her: simvastatin, metoprolol, aspirin, and clopidogrel. From the admission assessment, the nurse saw that the patient stopped taking her previously prescribed statin because of its cost. She also noted that Patient Z's fasting lipid levels were high; some diet teaching might be helpful in assisting the patient to modify her diet and reduce this risk factor. The nurse referred Patient Z to social work for possible financial assistance with medications and to the dietician for assistance with diet changes. When questioned, the patient stated that she preferred written information in English, so written material on reducing cholesterol and triglyceride consumption were provided as well as a list of local resources. The nurse also reviewed all of Patient Z's current medications with her when she administered them, stressing the importance of taking them as prescribed and making sure that the patient understood the purpose and prescribed dosage of all her new medications. Provided education and the patient's responses were recorded in the patient's medical record.
Comments and Rationale : Patient education should be provided in the language and format that the patient prefers. Teaching about new medications and facilitating the patient's ability to obtain medications after discharge through referral to social work or appropriate resources is very important. Short hospital stays do not permit time for exhaustive, extensive education. Written materials and referrals that the patient can use to follow up on recommended lifestyle changes are therefore helpful. Risk reduction for Patient Z will involve major lifestyle changes. Healthcare practitioners in all settings who encounter this patient will have a role to play in promoting increased adherence to recommended measures.
The identification of the pathophysiologic process leading to ACS has redefined the treatment of this spectrum of cardiac disorders, and researchers continue to refine therapeutic options to produce optimal patient outcomes. Despite a shared initiating event (plaque rupture or erosion), UA/NSTEMI and STEMI are distinct clinical entities, with differences in pathophysiology, clinical presentation, treatment, and prognosis. The diagnosis of UA/NSTEMI (also known as NSTE-ACS) relies primarily on elevated levels of cardiac troponins and the lack of ST-segment elevation on ECG. By contrast, the diagnosis of STEMI is made solely on ECG findings. After the type of MI has been determined, complex decision making is required to determine the appropriate course of treatment.
The goal of immediate treatment of NSTE-ACS is relief of ischemia and prevention of recurrent ischemic events. Risk stratification is essential for determining whether an early invasive or ischemia-guided strategy is best for the patient. Antiplatelet therapy, P2Y12 inhibitors, and antithrombotic therapy are adjuncts to treatment. With STEMI, the goal of immediate treatment is re-establishment of blood flow to the heart. The crucial factor for determining the treatment approach is timing from the onset of symptoms to treatment and from arrival in the emergency department to treatment. The preferred option for reperfusion is PCI, but the recommended 90-minute door-to-balloon time is difficult to achieve in most cases. However, there is an increased emphasis on developing systems of care that increase patient access to primary PCI. The other option for reperfusion, fibrinolytic therapy, has the advantage of immediately re-establishing blood flow, but it is associated with lower rates of reperfusion and higher risks compared with PCI. Ancillary therapy with antiplatelet therapy, P2Y12 inhibitors, and antithrombotic therapy is used to maintain patency of the infarct-related artery and prevent reocclusion.
Review of data from several large-scale studies, cardiac registries, and quality improvement initiatives has shown that adherence to guideline recommendations for the diagnosis, treatment, and secondary prevention NSTE-ACS and STEMI are suboptimal, particularly for older individuals, women, and minority populations. In addition, an inverse relationship has been found between risk and treatment, with more low-risk patients than high-risk patients receiving aggressive treatment. The data have also demonstrated a clear benefit in survival and outcomes when guideline recommendations are followed. Thus, clinicians should become more familiar with these guidelines and should encourage hospitals to implement system-wide policies and procedures to facilitate guideline-driven care. The use of protocols, clinical pathways, and standardized order forms can help to ensure that all patients receive appropriate care in a timely manner. After discharge, effective communication among the treating physician, the healthcare team, the patient and family, and the patient's primary care clinician is essential for ensuring long-term compliance with lifestyle modifications and medications, which will help to reduce the risk of future cardiac events.
| American Heart Association |
| 1-800-242-8721 |
| https://www.heart.org |
| American Cancer Society |
| 1-800-227-2345 |
| https://www.cancer.org |
| American Lung Association |
| 1-800-586-4872 |
| https://www.lung.org |
| DASH Diet Eating Plan |
| https://dashdiet.org |
| D2B Sustain the Gain |
| https://www.d2balliance.org |
| Assessing Cardiovascular Risk: Systematic Evidence Review from the Risk Assessment Work Group |
| https://www.nhlbi.nih.gov/health-topics/assessing-cardiovascular-risk |
| Global Registry of Acute Coronary Events (GRACE) |
| https://www.outcomes-umassmed.org/grace |
| National Heart, Lung, and Blood Institute |
| 1-877-645-2448 |
| https://www.nhlbi.nih.gov |
| TIMI Study Group |
| 1-800-385-4444 |
| http://www.timi.org |
2. O'Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127(4):e362-e425.
3. Amsterdam E, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes. J Am Coll Cardiol. 2014;64(24):e139-228.
4. Tian J, Ren X, Vergallo R, et al. Distinct morphological features of ruptured culprit plaque for acute coronary events compared to those with silent rupture and thin-cap fibroatheroma: a combined optical coherence tomography and intravascular ultrasound study. J Am Coll Cardiol. 2014;63(21):2209-2216.
5. Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention: executive summary. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation. 2011;124:2574-2609.
6. Hillis LD, Smith PK, Anderson JL, et al. 2011 ACCF/AHA guideline for coronary artery bypass graft surgery: executive summary. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011;124(23):2610-2642.
7. Maddox TM, Ho PM, Tsai TT, et al. Clopidogrel use and hospital quality in medically managed patients with non-ST-segment-elevation myocardial infarction. Circ Cardiovasc Qual Outcomes. 2012;5(4):523-531.
8. Sherwood MW, Wiviott SD, Peng SA, et al. Early clopidogrel versus prasugrel use among contemporary STEMI and NSTEMI patients in the U.S.: insights from the National Cardiovascular Data Registry. J Am Heart Assoc. 2014;3(2):e000849.
9. Peterson ED, Shah BR, Parsons L. Trends in quality of care for patients with acute myocardial infarction in the National Registry of Myocardial Infarction from 1990 to 2006. Am Heart J. 2008;156(6):1045-1055.
10. Somma KA, Bhatt DL, Fonarow GC, et al. Guideline adherence after ST-segment elevation versus non-ST segment elevation myocardial infarction. Circ Cardiovasc Qual Outcomes. 2012;5(5):654-661.
11. Poon S, Goodman SG, Yan RT, et al. Bridging the gender gap: insights from a contemporary analysis of sex-related differences in the treatment and outcomes of patients with acute coronary syndromes. Am Heart J. 2012;163:66-73.
12. Wang TY, Chen AY, Roe MT, et al. Comparison of baseline characteristics, treatment patterns, and in-hospital outcomes of Asian versus non-Asian white Americans with non-ST-segment elevation acute coronary syndromes from the CRUSADE quality improvement initiative. Am J Cardiol. 2007;100(3):391-396.
13. Patel MR, Chen AY, Roe MT, et al. A comparison of acute coronary syndrome care at academic and nonacademic hospitals. Am J Med. 2007;120(1):40-46.
14. Alexander KP, Newby LK, Cannon CP, et al. Acute coronary care in the elderly, part I: non-ST-segment-elevation acute coronary syndromes: a scientific statement for healthcare professionals from the American Heart Association Council on Clinical Cardiology: in collaboration with the Society of Geriatric Cardiology. Circulation. 2007;115(19):2549-2569.
15. Grosmaitre P, Le Vavasseur O, Yachouh E, et al. Significance of atypical symptoms for the diagnosis and management of myocardial infarction in elderly patients admitted to emergency departments. Arch Cardiovasc Dis. 2013;106(11):586-592.
16. Dreyer RP, Wang Y, Strait KM, et al. Gender differences in the trajectory of recovery in health status among young patients with acute myocardial infarction: results from the VIRGO study. Circulation. 2015;131(22):1971-1980.
17. Alfredsson J, Clayton T, Damman P, et al. Impact of an invasive strategy on 5 years outcome in men and women with non-ST-segment elevation acute coronary syndromes. Am Heart J. 2014;168(4):522-529.
18. Davis M, Diamond J, Montgomery D, Krishnan S, Eagle K, Jackson E. Acute coronary syndrome in young women under 55 years of age: clinical characteristics, treatment, and outcomes. Clin Res Cardiol. 2015;104(8):648-655.
19. Roe MT. Success stories: how hospitals are improving care. Am Heart J. 2004;148(5 Suppl):S52-S55.
20. LaBresh KA, Fonarow GC, Smith SC Jr, et al. Improved treatment of hospitalized coronary artery disease patients with the Get with the Guidelines Program. Crit Pathw Cardiol. 2007;6(3):98-105.
21. Grol R. Improving the quality of medical care: building bridges among professional pride, payer profit, and patient satisfaction. JAMA. 2001;286(20):2578-2585.
22. Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction. J Am Coll Cardiol. 2018;138:e618-e651.
23. Virani SS, Alonso A, Aparicio HJ, et al. Heart disease and stroke statistics – 2021 update. A report from the American Heart Association. Circulation. 143(8):e254-e743.
25. Lansky AJ, Ng VG, Maehara A, et al. Gender and the extent of coronary atherosclerosis, plaque composition, and clinical outcomes in acute coronary syndromes. JACC Cardiovasc Imaging. 2012;5(3 Suppl):S62-S72.
26. Leening MJ, Ferket BS, Steyerberg EW, et al. Sex differences in lifetime risk and first manifestation of cardiovascular disease: prospective population based cohort study. BMJ. 2014;349:g5992.
27. Motoyama S, Sarai M, Harigaya H, et al. Computed tomographic angiography characteristics of atherosclerotic plaques subsequently resulting in acute coronary syndrome. J Am Coll Cardiol. 2009;54(1):49-57.
28. Masoudi FA, Ponirakis A, de Lemos JA, et al. Trends in U.S. cardiovascular care: 2016 report from 4 ACC national cardiovascular data registries. J Am Coll Cardiol. 2017;69(11):1427-1450.
29. Kontos MC, Rennyson SL, Chen AY, Alexander KP, Peterson ED, Roe MT. The association of myocardial infarction process of care measures and in-hospital mortality: a report from the NCDR®. Am Heart J. 2014;168(5):766-775.
30. Marceau A, Samson JM, Laflamme N, et al. Short and long-term mortality after STEMI versus non-STEMI: a systematic review and meta-analysis [abstract]. J Am Coll Cardiol. 2013;61(10):e96.
31. Bentzon JF, Otsuka F, Virmani R, Falk E. Mechanisms of plaque formation and rupture. Circ Res. 2014;114(12):1852-1866.
32. Boudi FB. Noncoronary Atherosclerosis Overview of Atherosclerosis. Available at https://emedicine.medscape.com/article/1950759-overview. Last accessed December 28, 2021.
33. American Heart Association. Available at https://www.heart.org/en/. Last accessed December 28, 2021.
34. Jacobson C, Marzlin K, Webner C. Cardiovascular Nursing Practice. Burien, WA: Cardiovascular Nursing Education Associates; 2007.
35. Mosca L, Linfante AH, Benjamin EJ, et al. National study of physician awareness and adherence to cardiovascular disease prevention guidelines. Circulation. 2005;111(4):499-510.
36. Falk E, Nakano M, Bentzon JF, Finn AV, Virmani R. Update on acute coronary syndromes: the pathologists' view. Eur Heart J. 2013;34(10):719-728.
37. Sakakura K, Nakano M, Otsuka F, Ladich E, Kolodgie FD, Virmani R. Pathophysiology of atherosclerosis plaque progression.Heart Lung Circ. 2013;22(6):399-411.
38. Rittersma SZH, van der Wal AC, Koch KT, et al. Plaque instability frequently occurs days or weeks before occlusive coronary thrombosis: a pathological thrombectomy study in primary percutaneous coronary intervention. Circulation. 2005;111:1160-1165.
39. Virmani R, Burke AP, Farb A, Kolodgie FD. Pathology of the vulnerable plaque. J Am Coll Cardiol. 2006;47(8 Suppl):C13-C18.
40. Cheruvu PK, Finn AV, Gardner C, et al. Frequency and distribution of thin-cap fibroatheroma and ruptured plaques in human coronary arteries: a pathologic study. J Am Coll Cardiol. 2007;50(10):940–949.
41. Fuji K, Kawasaki D, Masutani M, et al. OCT assessment of thin-cap fibroatheroma distribution in native coronary arteries. JACC Cardiovasc Imaging. 2010;3(2):168-175.
42. Wykrzykowska JJ, Mintz GS, Garcia-Garcia HM, et al. Longitudinal distribution of plaque burden and necrotic core-rich plaques in nonculprit lesions of patients presenting with acute coronary syndromes. JACC Cardiovasc Imaging. 2012;5(3 Suppl):S10-S18.
43. Xie Y, Mintz GS, Yang J, et al. Clinical outcome of nonculprit plaque ruptures in patients with acute coronary syndrome in the PROSPECT study. JACC Cardiovasc Imaging. 2014;7(4):397-405.
44. Shimamura K, Ino Y, Kubo T, et al. Difference of ruptured plaque morphology between asymptomatic coronary artery disease and non-ST elevation acute coronary syndrome patients: an optical coherence tomography study. Atherosclerosis. 2014;235(2):532-537.
45. Libby P. Mechanisms of acute coronary syndromes and their implications for therapy. N Engl J Med. 2013;368(21):2004-2013.
46. Ino Y, Kubo T, Tanaka A, et al. Difference of culprit lesion morphologies between ST-segment elevation myocardial infarction and non-ST-segment elevation acute coronary syndrome: an optical coherence tomography study. JACC Cardiovasc Interv. 2011;4(1):76-82.
47. Foster DB. Twelve-Lead Electrocardiography: Theory and Interpretation. 2nd ed. London: Springer-Verlag; 2007.
48. McCord J, Jneid H, Hollander JE, et al. Management of cocaine-associated chest pain and myocardial infarction: a scientific statement from the American Heart Association Acute Cardiac Care Committee of the Council on Clinical Cardiology. Circulation. 2008;117(14):1897-1907.
49. Wilson PW, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97(18):1837-1847.
50. Greenland P, Alpert JS, Beller GA, et al. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: executive summary. Circulation. 2010;122(25):2748-2764.
51. Rodondi N, Locatelli I, Aujesky D, et al. Framingham risk score and alternatives for prediction of coronary heart disease in older adults. PLoS One. 2012;7(3):e34287.
52. Goff DC Jr, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl 2):S49-S73.
53. U.S. Preventative Services Task Force. Hypertension in Adults: Screening. Available at https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/hypertension-in-adults-screening. Last accessed December 28, 2021.
54. U.S. Preventative Services Task Force. Statin Use for the Primary Prevention of Cardiovascular Disease in Adults: Preventive Medication. Available at https://uspreventiveservicestaskforce.org/uspstf/recommendation/statin-use-in-adults-preventive-medication. Last accessed December 28, 2021.
55. U.S. Preventative Services Task Force. Tobacco Smoking Cessation in Adults, Including Pregnant Persons: Interventions. Available at https://uspreventiveservicestaskforce.org/uspstf/recommendation/tobacco-use-in-adults-and-pregnant-women-counseling-and-interventions. Last accessed December 28, 2021.
56. Buckley DI, Fu R, Freeman M, Rogers K, Helfand M. C-reactive protein as a risk factor for coronary heart disease: a systematic review and meta-analyses for the U.S. Preventive Services Task Force. Ann Intern Med. 2009;151(7):483-495.
57. Emerging Risk Factors Collaboration. C-reactive protein, fibrinogen, and cardiovascular disease prediction. N Engl J Med. 2012;367(14):1310-1320.
58. Helfand M, Buckley DI, Freeman M, et al. Emerging risk factors for coronary heart disease: a summary of systematic reviews conducted for the U.S. Preventive Services Task Force. Ann Intern Med. 2009;151(7):496-507.
59. Emerging Risk Factors Collaboration. Lipid-related markers and cardiovascular disease prediction. JAMA. 2012;307(23):2499-2506.
60. Gepner AD, Young R, Delaney JA, et al. Comparison of coronary artery calcium presence, carotid plaque presence, and carotid intima-media thickness for cardiovascular disease prediction in the Multi-Ethnic Study of Atherosclerosis. Circ Cardiovasc Imaging. 2015;8(1).
61. Zeb I, Budoff M. Coronary artery calcium screening: does it perform better than other cardiovascular risk stratification tools? Int J Mol Sci. 2015;16(3):6606-6620.
62. Taylor AJ, Cerqueira M, Hodgson JMcB, et al. ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 appropriate use criteria for cardiac computed tomography. A report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the Society of Cardiovascular Computed Tomography, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the American Society of Nuclear Cardiology, the North American Society for Cardiovascular Imaging, the Society for Cardiovascular Angiography and Interventions, and the Society for Cardiovascular Magnetic Resonance. Circulation. 2010;122(21):e525-e555.
63. Peters SA, den Ruijter HM, Bots ML, Moons KG. Improvements in risk stratification for the occurrence of cardiovascular disease by imaging subclinical atherosclerosis: a systematic review. Heart. 2012;98(3):177-184.
64. Peters SA, Bakker M, den Ruijter HM, Bots ML. Added value of CAC in risk stratification for cardiovascular events: a systematic review. Eur J Clin Invest. 2012;42(1):110-116.
65. Chou R, for the High Value Care Task Force of the American College of Physicians. Cardiac screening with electrocardiography, stress echocardiography, or myocardial perfusion imaging: advice for high-value care from the American College of Physicians. Ann Intern Med. 2015;162(6):438-447.
66. U.S. Preventive Services Task Force. Cardiovascular Disease Risk: Screening with Electrocardiograpy. Available at https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/cardiovascular-disease-risk-screening-with-electrocardiography. Last accessed December 28, 2021.
67. Whelton PK, Carey RM, Aranow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71(6):e1-e487.
68. Navar-Boggan AM, Pencina MJ, Williams K, Sniderman AD, Peterson ED. Proportion of U.S. adults potentially affected by the 2014 hypertension guideline. JAMA. 2014;311(14):1424-1429.
69. Borden WB, Maddox TM, Tang F, et al. Impact of the 2014 expert panel recommendations for management of high blood pressure on contemporary cardiovascular practice: insights from the NCDR PINNACLE registry. J Am Coll Cardiol. 2014;64(21):2196-2203.
70. Murthy VL, Shah RV, Rubenfire M, Brook RD. Comparison of the treatment implications of American Society of Hypertension and International Society of Hypertension 2013 and Eighth Joint National Committee Guidelines: an analysis of National Health and Nutrition Examination Survey. Hypertension. 2014;64(2):275-280.
71. Blood Pressure Lowering Treatment Trialists' Collaboration. Blood pressure-lowering treatment based on cardiovascular risk: a meta-analysis of individual patient data. Lancet. 2014;384(9943):591-598.
72. Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl 2):S1-S45.
73. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA. 2001;285(19):2486-2497.
74. Hughes LS, Ebell MH. 2013 ACC/AHA cholesterol guideline greatly increases number eligible for statin treatment. Am Fam Physician. 2014;90(4):online.
75. Schoen MW, Salas J, Scherrer JF, Buckhold FR. Cholesterol treatment and changes in guidelines in an academic medical practice. Am J Med. 2015;128(4):403-409.
76. Johnson KM, Dowe DA. Accuracy of statin assignment using the 2013 AHA/ACC Cholesterol Guideline versus the 2001 NCEP ATP III guideline: correlation with atherosclerotic plaque imaging. J Am Coll Cardiol. 2014;64(9):910-919.
77. Martin SS, Sperling LS, Blaha MJ, et al. Clinician-patient risk discussion for atherosclerotic cardiovascular disease prevention: importance to implementation of the 2013 ACC/AHA guidelines. J Am Coll Cardiol. 2015;65(13):1361-1368.
78. Mozaffarian D, Wilson PWF, Kannel WB. Beyond established and novel risk factors. Lifestyle risk factors for cardiovascular disease. Circulation. 2008;117:3031-3038.
79. Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation. 2014;129(25 Suppl 2):S102-S138.
80. Ebbert JO, Elrashidi MY, Jensen MD. Managing overweight and obesity in adults to reduce cardiovascular disease risk. Curr Athersoscler Rep. 2014;16(10):445.
81. Eckel RH, Jakicic JM, Ard JD, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(Suppl 2):S76-S99.
82. U.S. Preventive Services Task Force. Healthy Diet and Physical Activity for Cardiovascular Disease Prevention in Adults with Cardiovascular Risk Factors: Behavioral Counseling Interventions. Available at https://uspreventiveservicestaskforce.org/uspstf/recommendation/healthy-diet-and-physical-activity-counseling-adults-with-high-risk-of-cvd. Last accessed December 28, 2021.
83. Lin JS, O'Connor E, Evans CV, Senger CA, Rowland MG, Groom HC. Behavioral counseling to promote a healthy lifestyle in persons with cardiovascular risk factors. A systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2014;161(8):566-578.
84. Pearson TA, Palaniappan LP, Artinian NT, et al. American Heart Association guide for improving cardiovascular health at the community level, 2013 update. A scientific statement for public health practitioners, healthcare providers, and health policy makers. Circulation. 2013;127(16):1730-1753.
85. U.S. Preventive Services Task Force. Behavioral counseling interventions to promote a healthy diet and physical activity for cardiovascular disease prevention in adults without cardiovascular risk factors. JAMA. 2020;324(20):2069-2075.
86. Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008;10(12):1-23.
87. Ventola CL. Current issues regarding complementary and alternative medicine (CAM) in the United States: part 1: the widespread use of CAM and the need for better-informed health care professionals to provide patient counseling. P T. 2010;35(8):461-468.
88. Clarke TC, Black LI, Stussman BJ, Barnes PM, Nahin RL. Trends in the use of complementary health approaches among adults: United States, 2001–2012. Natl Health Stat Report. 2015;79:1-15.
89. Flowers N, Hartley L, Todkill D, Stranges S, Rees K. Co-enzyme Q10 supplementation for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2014;12:CD010405.
90. Moyer VA, LeFevre ML, Siu AL, et al. Vitamin, mineral, and multivitamin supplements for the primary prevention of cardiovascular disease and cancer: U.S. Preventive services Task Force recommendation statement. Ann Intern Med. 2014;160(8):558-564.
91. Rees K, Harley L, Day C, Flowers N, Clarke A, Stranges S. Selenium supplementation for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2013;1:CD009671.
92. Hartley L, Flowers N, Holmes J, et al. Green and black tea for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2013;6:CD009934.
93. Hartley L, Flowers N, Lee MS, Ernst E, Rees K. Tai chi for primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2014;4:CD010366.
94. Rees K, Takeda A, Martin N, et al. 'Mediterranean' dietary pattern for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2019;3:CD009825.
95. Doroodchi H, Abdolrasulnia M, Foster JA, et al. Knowledge and attitudes of primary care physicians in the management of patients at risk for cardiovascular events. BMC Fam Pract. 2008;9:42.
96. Hira RS, Kennedy K, Nambi V, et al. Frequency and practice-level variation in inappropriate aspirin use for the primary prevention of cardiovascular disease: insights from the National Cardiovascular Disease Registry's Practice Innovation and Clinical Excellence registry. J Am Coll Cardiol. 2015;65(2):111-121.
97. Mathews R, Peterson ED, Li S, et al. Use of emergency medical service transport among patients with ST-segment-elevation myocardial infarction: findings from the National Cardiovascular Data Registry Acute Coronary Treatment Intervention Outcomes Network Registry-Get With The Guidelines. Circulation. 2011;124(2):154-163.
98. Henderson SO, Magana RN, Korn CS, Genna T, Bretsky PM. Delayed presentation for care during acute myocardial infarction in a Hispanic population of Los Angeles County. Ethn Dis. 2002;12(1):38-44.
99. McGinn AP, Rosamund WD, Goff DC Jr, Taylor HA, Miles JS, Chambless L. Trends in prehospital delay time and use of emergency medical services for acute myocardial infarction: experience in 4 U.S. communities from 1987–2000. Am Heart J. 2005;150(3):392-400.
100. Peacock WF, Hollander JE, Smalling RW, Bresler MJ. Reperfusion strategies in the emergency treatment of ST-segment elevation myocardial infarction. Am J Emerg Med. 2006;25(3):353-366.
101. Haro LH, Decker WW, Boie ET, Wright SR. Initial approach to the patient who has chest pain. Cardiol Clin. 2006;24(1):1-17.
102. Kosuge M, Kimura K, Ishikawa T, et al. Differences between men and women in terms of clinical features of ST-segment elevation acute myocardial infarction. Circ J. 2006;70(3):222-226.
103. McNamara RL, Wang Y, Herrin J, et al. Effect of door-to-balloon time on mortality in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2006;47:2180-2186.
104. Blomkalns AL, Chen AY, Hochman JS, et al. Gender disparities in the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes: large-scale observations from the CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the American College of Cardiology/American Heart Association Guidelines) National Quality Improvement Initiative. J Am Coll Cardiol. 2005;45(6):832-837.
105. Kosuge M, Kimura K, Ishikawa T, et al. Differences between men and women in terms of clinical features of ST-segment elevation acute myocardial infarction. Circ J. 2006;70(3):222-226.
106. McNamara RL, Wang Y, Herrin J, et al. Effect of door-to-balloon time on mortality in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2006;47:2180-2186.
107. Arslanian-Engoren C, Patel A, Fang J, et al. Symptoms of men and women presenting with acute coronary syndromes. Am J Cardiol. 2006;98(9):1177-1181.
108. Heer T, Gitt AK, Juenger C, et al. Gender differences in acute non-ST-segment elevation myocardial infarction. Am J Cardiol. 2006;98(2):160-166.
109. Shaw LJ, Shaw RE, Merz CN, et al. Impact of ethnicity and gender differences on angiographic coronary artery disease prevalence and in-hospital mortality in the American College of Cardiology-National Cardiovascular Data Registry. Circulation. 2008;117(14):1787-1801.
110. Pryor DB, Shaw L, McCants CB, et al. Value of the history and physical in identifying patients at increased risk for coronary artery disease. Ann Intern Med. 1993;118(2):81-90.
111. Morise AP, Haddad WJ, Beckner D. Development and validation of a clinical score to estimate the probability of coronary artery disease in men and women presenting with suspected coronary disease. Am J Med. 1997;102(4):350-356.
112. Ho KT, Miller TD, Hodge DO, Bailey KR, Gibbons RJ. Use of a simple clinical score to predict prognosis of patients with normal or mildly abnormal resting electrocardiographic findings undergoing evaluation for coronary artery disease. Mayo Clin Proc. 2002;77(6):515-521.
113. Morise AP, Haddad WJ, Beckner D. Development and validation of a clinical score to estimate the probability of coronary artery disease in men and women presenting with suspected coronary disease. Am J Med. 1997;102(4):350-356.
114. Amsterdam EA, Kirk JD, Bluemke DA, et al. Testing of low-risk patients presenting to the emergency department with chest pain. A scientific statement from the American Heart Association. Circulation. 2010;122(17):1756-1776.
115. Winters ME, Katzen SM. Identifying chest pain emergencies in the primary care setting. Prim Care. 2006;33(3):625-642.
116. Patel H, Rosengren A, Ekman I. Symptoms in acute coronary syndromes: does sex make a difference? Am Heart J. 2004;148(1):27-33.
117. Canto JG, Goldberg RJ, Hand MM, et al. Symptom presentation of women with acute coronary syndromes: myth vs. reality. Arch Intern Med. 2007;167(22):2405-2413.
118. Panju AA, Hemmelgarn BR, Guyatt GH, Simel DL. Is this patient having a myocardial infarction? JAMA. 1998;280(14):1256-1263.
119. Goldberg R, Goff D, Cooper L, et al. Age and sex differences in presentation of symptoms among patients with acute coronary disease: the REACT Trial (Rapid Early Action for Coronary Treatment). Coron Artery Dis. 2000;11(5):399-407.
122. Butler KH, Swencki SA. Chest pain: a clinical assessment. Radiol Clin North Am. 2006;44(2):165-179.
123. Kelly BS. Evaluation of the elderly patient with acute chest pain. Clin Geriatr Med. 2007;23(2):327-349.
124. Eslick GD. Usefulness of chest pain character and location as diagnostic indicator of an acute coronary syndrome. Am J Cardiol. 2005;95(10):1228-1231.
125. Thygesen K, Alpert JS, Jaffee AS, Simoons ML, Chaitman BR, White HD, on behalf of the Joint ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial Infarction. Third universal definition of myocardial infarction. Circulation. 2012;126(16):2020-2035.
126. Arslanian-Engoren C, Engoren M. Physiological and anatomical bases for sex differences in pain and nausea as presenting symptoms of acute coronary syndromes. Heart Lung. 2010;39(5):386-393.
127. Thuresson M, Jarlöv MB, Lindahl B, Svensson L, Zedigh C, Herlitz J. Symptoms and type of symptom onset in acute coronary syndrome in relation to ST elevation, sex, age, and a history of diabetes. Am Heart J. 2005;150(2):234-242.
128. DeVon HA, Zerwic JJ. Symptoms of acute coronary syndromes: are there gender differences? A review of the literature. Heart Lung. 2002;31(4):235-245.
129. Meischke H, Larsen MP, Eisenberg MS. Gender differences in reported symptoms for acute myocardial infarction: impact on prehospital delay time interval. Am J Emerg Med. 1998;16(4):363-366.
130. Kyker KA, Limacher MC. Gender differences in the presentation and symptoms of coronary artery disease. Curr Womens Health Rep. 2002;2(2):115-119.
131. Arslanian-Engoren C, Patel A, Fang J, et al. Symptoms of men and women presenting with acute coronary syndromes. Am J Cardiol. 2006;98(9):1177-1181.
132. Stephen SA, Darney BG, Rosenfeld AG. Symptoms of acute coronary syndrome in women with diabetes: an integrative review of the literature. Heart Lung. 2008;37(3):179-189.
133. Merinopoulos I, Bloore D. But he has no chest pain…. Oxf Med Case Reports. 2014;2014(7):129-131.
134. Han JH, Lindsell CJ, Hornung RW, et al. The elder patient with suspected acute coronary syndromes in the emergency department. Acad Emerg Med. 2007;14(8):732-739.
135. Mosca L, Banka CL, Benjamin EJ, et al. Evidence-based guidelines for cardiovascular disease prevention in women: 2007 update. Circulation. 2007;115(11):1481-1501.
136. Ryan CJ, DeVon HA, Zerwic JJ. Typical and atypical symptoms: diagnosing acute coronary syndromes accurately. Am J Nurs. 2005;105(2):34-36.
137. Brieger D, Eagle KA, Goodman SG, et al. Acute coronary syndromes without chest pain, an underdiagnosed and undertreated high-risk group. Insights from the Global Registry of Acute Coronary Events. Chest. 2004;126(2):461-469.
138. Gurm HS, Topol EJ. The ECG in acute coronary syndromes: new tricks from an old dog. Heart. 2005;91(7):851-853.
139. Tsai CL, Magid DJ, Sullivan AF, et al. Quality of care for acute myocardial infarction in 58 U.S. emergency departments. Acad Emerg Med. 2010;17(9):940-950.
140. Dasari TW, Roe MT, Chen AY, et al. Impact of time of presentation on process performance and outcomes in ST-segment-elevation myocardial infarction: a report from the American Heart Association: Mission Lifeline program. Circ Cardiovasc Qual Outcomes. 2014;7(5):656-663.
141. Diercks DB, Peacock WF, Hiestand BC, et al. Frequency and consequences of recording an electrocardiogram >10 minutes after arrival in an emergency room in non–ST-segment elevation acute coronary syndromes (from the CRUSADE Initiative). Am J Cardiol. 2006;97(4):437-442.
142. Blomkalns AL, Roe MT, Peterson ED, Ohman EM, Fraulo ES, Gibler WB. Guideline implementation research: exploring the gap between evidence and practice in the CRUSADE Quality Improvement Initiative. Acad Emerg Med. 2007;14(11):949-954.
143. Tricoci P, Peterson ED, Roe MT; CRUSADE Quality Improvement Initiative. Patterns of guideline adherence and care delivery for patients with unstable angina and non-ST-segment elevation myocardial infarction (from the CRUSADE Quality Improvement Initiative). Am J Cardiol. 2006;98(12A):30Q-35Q.
144. Takakuwa KM, Burek GA, Estepa AT, Shofer FS. A method for improving arrival-to-electrocardiogram time in emergency department chest pain patients and the effect on door-to-balloon time for ST-segment elevation myocardial infarction. Acad Emerg Med. 2009;16(10):921-927.
145. Miller KL, Pollack CV Jr, Peterson ED. Moving from evidence to practice in the care of patients who have acute coronary syndrome. Cardiol Clin. 2006;24(1):87-102.
146. Jneid H, Anderson JL, Wright RS, et al. 2012 ACCF/AHA focused update of the guideline for the management of patients with unstable angina/non-ST-elevation myocardial infarction (updating the 2007 guideline and replacing the 2011 focused update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.J Am Coll Cardiol. 2012;60(7):645-681.
147. Corbett JV, Banks A. Laboratory Tests and Diagnostic Procedures with Nursing Diagnoses. 8th ed. Upper Saddle River, NJ: Pearson; 2012.
148. Barstow C, Rice M, McDivitt JD. Acute coronary syndrome: diagnostic evaluation. Am Fam Physician. 2017;95(3):170-177.
149. Cheitlin MD, Armstrong WF, Aurigemma GP, et al. ACC/AHA/ASE 2003 guideline update for the clinical application of echocardiography: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASE Committee to Update the 1997 Guidelines for the Clinical Application of Echocardiography). Circulation. 2003;108(9):1146-1162.
150. Bohula EA, Morrow DA. ST-elevation myocardial infarction: management. In: Mann DL, Zipes DP, Libby P, Bonow RO (eds). Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 11th ed. Philadelphia, PA: Elsevier/Saunders; 2019: 1172-1180.
152. White HD, Kleiman NS, Mahaffey KW, et al. Efficacy and safety of enoxaparin compared with unfractionated heparin in high-risk patients with non-ST-segment elevation acute coronary syndrome undergoing percutaneous coronary intervention in the Superior Yield of the New Strategy of Enoxaparin, Revascularization and Glycoprotein IIb/IIIa Inhibitors (SYNERGY) trial.Am Heart J. 2006;152(6):1042-1050.
153. Kwong RY, Schussheim AE, Rekhraj S, et al. Detecting acute coronary syndrome in the emergency department with cardiac magnetic resonance imaging. Circulation. 2003;107(4):531-537.
154. Gibbons R, Balady GJ, Bricker JT, et al. ACC/AHA 2002 guideline update for exercise testing: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines). Circulation. 2002;106:1883-1892.
155. Hinkle JL, Cheever KH. Brunner and Suddarth's Textbook of Medical-Surgical Nursing. 14th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2018.
156. U.S. Food and Drug Administration. FDA Warns of Rare but Serious Risk of Heart Attack and Death With Cardiac Nuclear Stress Test Drugs Lexiscan (regadenoson) and Adenoscan (Adenosine). Available at https://www.fda.gov/Drugs/DrugSafety/ucm375654.htm. Last accessed December 28, 2021.
157. Collinson PO, Gaze DC, Thokala P, Goodacre S. Randomised assessment of treatment using panel assay of cardiac markers—contemporary biomarker evaluation (RATPAC CBE). Health Technol Assess. 2013;17(15):v-vi, 1-122.
158. Rosenbaum LS, Januzzi JL. Moving troponin testing into the 21st century: will greater sensitivity be met with greater sensibility? Cardiovasc Hematol Disord Drug Targets. 2008;8(2):118-126.
159. Layfield C, Rose J, Alford A, et al. Effectiveness of practices for improving the diagnostic accuracy of non ST elevation myocardial infarction in the emergency department: A Laboratory Medicine Best Practices™ systematic review. Clin Biochem. 2015;48(4-5):204-212.
160. Dai X, Busby-Whitehead J, Alexander KP. Acute coronary syndrome in older adults. J Geriatr Cardiol. 2016;13:101-108.
161. Hoeller R, Rubini Giménez M, Reichlin T, et al. Normal presenting levels of high-sensitivity troponin and myocardial infarction. Heart. 2013;99(21):1567-1572.
162. Weber M, Bazzino O, Navarro Estrada JL, et al. N-terminal B-type natriuretic peptide assessment provides incremental prognostic information in patients with acute coronary syndromes and normal troponin T values upon admission. J Am Coll Cardiol. 2008;51(12):1188-1195.
163. Haaf P, Reichlin T, Corson N, et al. B-type natriuretic peptide in the early diagnosis and risk stratification of acute chest pain.Am J Med. 2011;124(5):444-452.
164. Antman EM, Cohen M, Bernink PJ, et al. The TIMI risk score for unstable angina/non-ST elevation MI: a method for prognostication and therapeutic decision making. JAMA. 2000;284(7):835-842.
165. Granger CB, Goldberg RJ, Dabbous O, et al. Predictors of hospital mortality in the global registry of acute coronary events. Arch Intern Med. 2003;163(19):2345-2353.
166. Windhausen F, Hirsch A, Tijssen JG, et al. ST-segment deviation on the admission electrocardiogram, treatment strategy, and outcome in non-ST-elevation acute coronary syndromes: substudy of the Invasive versus Conservative Treatment in Unstable coronary Syndromes (ICTUS) Trial. J Electrocardiol. 2007;40(5):408-415.
167. Weinstock MB, Weingart S, Orth F, et al. Risk for clinically relevant adverse cardiac events in patients with chest pain at hospital admission. JAMA Intern Med. 2015;175(7):1207-1212.
168. Than M, Aldous S, Lord SJ, et al. A 2-hour diagnostic protocol for possible cardiac chest pain in the emergency department: a randomized clinical trial. JAMA Intern Med. 2014;174(1):51-58.
169. Aldous SJ, Richards MA, Cullen L, Troughton R, Than M. A new improved accelerated diagnostic protocol safely identifies low-risk patients with chest pain in the emergency department. Acad Emerg Med. 2012;19(5):510-516.
170. Six AJ, Backus BE, Kelder JC. Chest pain in the emergency room: value of the HEART score. Netherlands Heart Journal. 2008;16(6):191-196.
171. Mahler SA, Riley RF, Hiestand BC, et al. The HEART Pathway randomized trial: identifying emergency department patients with acute chest pain for early discharge. Circ Cardiovasc Qual Outcomes. 2015;8(2):195-203.
172. Fraker TJ, Fihn SD. 2007 Chronic angina focused update of the ACC/AHA 2002 guidelines for the management of patients with chronic stable angina: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines Writing Group to develop the focused update of the 2002 guidelines for the management of patients with chronic stable angina. J Am Coll Cardiol. 2007;50(23):2264-2274.
174. Miller CD, Roe MT, Mulgund J, et al. Impact of acute beta-blocker therapy for patients with non-ST-segment elevation myocardial infarction. Am J Med. 2007;120(8):685-692.
175. Buch P, Rasmussen S, Abildstrom SZ, Køber L, Carlsen J, Torp-Pedersen C; TRACE investigators. The long-term impact of the angiotensin-converting enzyme inhibitor trandolapril on mortality and hospital admissions in patients with left ventricular dysfunction after a myocardial infarction: follow-up to 12 years. Eur Heart J. 2005;26(2):145-152.
176. Teo KK, Yusuf S, Pfeffer M, et al. Effects of long-term treatment with angiotensin-converting-enzyme inhibitors in the presence or absence of aspirin: a systematic review. Lancet. 2002;360(9339):1037-1043.
177. Murphy JG, Lloyd MA (eds). Mayo Clinic Cardiology. 3rd ed. Toronto: Mayo Clinical Scientific Press; 2007.
178. Tataris KL, Mercer MP, Govindarajan P. Prehospital aspirin administration for acute coronary syndrome (ACS) in the USA: an EMS quality assessment using the NEMSIS 2011 database. Emerg Med J. 2015;32(11):876-881.
179. Nguyen HL, Goldberg RJ, Gore JM, et al. Age and sex differences, and changing trends, in the use of evidence-based therapies in acute coronary syndromes: perspectives from a multinational registry. Coron Artery Dis. 2010;21(6):336-344.
180. Yusuf S, Zhao F, Mehta SR, et al. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med. 2001;345(7):494-502.
181. Wiviott SD, Trenk D, Frelinger AL, et al. Prasugrel compared with high loading- and maintenance-dose clopidogrel in patients with planned percutaneous coronary intervention: the Prasugrel in Comparison to Clopidogrel for Inhibition of Platelet Activation and Aggregation-Thrombolysis in Myocardial Infarction 44 trial. Circulation. 2007;116(25):2923-2932.
182. Roe MT, Armstrong PW, Fox KA, et al. Prasugrel versus clopidogrel for acute coronary syndromes without revascularization.N Engl J Med. 2012;367(14):1297-1309.
183. Lexi-Comp Online. Available at https://online.lexi.com. Last accessed December 28, 2021.
184. Gaglia MA Jr, Waksman R. Overview of the 2010 Food and Drug Administration Cardiovascular and Renal Drugs Advisory Committee meeting regarding ticagrelor. Circulation. 2011;123:451-456.
185. Wallentin L, Becker RC, Budaj A, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361(11):1045-1057.
186. Mahaffey KW, Wojdyla DM, Carroll K, et al. Ticagrelor compared with clopidogrel by geographic region in the Platelet Inhibition and Patient Outcomes (PLATO) trial. Circulation. 2011;124(5):544-554.
187. Bosch X, Marrugat J, Sanchis J. Platelet glycoprotein IIb/IIIa blockers during percutaneous coronary intervention and as the initial medical treatment of non-ST segment elevation acute coronary syndromes. Cochrane Database Syst Rev. 2013;11:CD002130.
188. Mehta RH, Roe MT, Chen AY, et al. Recent trends in the care of patients with non-ST-segment elevation acute coronary syndromes: insights from the CRUSADE initiative. Arch Intern Med. 2006;166(18):2027-2034.
189. Spinler SA. Managing acute coronary syndrome: evidence-based approaches. Am J Health Syst Pharm. 2007;64(11 Suppl 7):S14-S24.
190. Fox KA, Anderson FA Jr, Dabbous OH, et al. Intervention in acute coronary syndromes: do patients undergo intervention on the basis of their risk characteristics? The Global Registry of Acute Coronary Events (GRACE). Heart. 2007;93(2):177-182.
191. Hoekstra JW, Roe MT, Peterson ED, et al. Early glycoprotein Iib/IIIa inhibitor use for non-ST-segment elevation acute coronary syndrome: patient selection and associated treatment patterns. Acad Emerg Med. 2005;12(5):431-438.
192. Alexander KP, Chen AY, Roe MT, et al. Excess dosing of antiplatelet and antithrombin agents in the treatment of non-ST-segment elevation acute coronary syndromes. JAMA. 2005;294(24):3108-3116.
193. Bhatheja R, Mukherjee D. Acute coronary syndromes: unstable angina/non-ST elevation myocardial infarction. Crit Care Clin. 2007;23(4):709-735.
194. Goodman SG, Fitchett D, Armstrong PW, Tan M, Langer A. Randomized evaluation of the safety and efficacy of enoxaparin versus unfractionated heparin in high-risk patients with non-ST-segment elevation acute coronary syndromes receiving the glycoprotein IIb/IIIa inhibitor eptifibatide. Circulation. 2003;107:238-244.
195. Petersen JL, Mahaffey KW, Hasselblad V, et al. Efficacy and bleeding complications among patients randomized to enoxaparin or unfractionated heparin for antithrombin therapy in non-ST-Segment elevation acute coronary syndromes: a systematic overview. JAMA. 2004;292(1):89-96.
196. He P, Liu Y, Wei X, et al. Comparison of enoxaparin and unfractionated heparin in patients with non-ST-segment elevation acute coronary syndrome undergoing percutaneous coronary intervention: a systematic review and meta-analysis. J Thorac Dis. 2018;10(6):3308-3318.
197. LaPointe NM, Chen AY, Alexander KP, et al. Enoxaparin dosing and associated risk of in-hospital bleeding and death in patients with non ST-segment elevation acute coronary syndromes. Arch Intern Med. 2007;167(14):1539-1544.
198. Stone GW, McLaurin BT, Cox DA, et al. Bivalirudin for patients with acute coronary syndromes. N Engl J Med. 2006;355(21):2203-2216.
199. Stone GW, Ware JH, Bertrand ME, et al. Antithrombotic strategies in patients with acute coronary syndromes undergoing early invasive management: one-year results from the ACUITY trial. JAMA. 2007;298(21):2497-2506.
200. Bavry AA, Elgendy IY, Mahmoud A, Jadhav MP, Huo T. Critical appraisal of bivalirudin versus heparin for percutaneous coronary intervention: a meta-analysis of randomized trials. PLoS One. 2015;10(5):e0127832.
201. Yusuf S, Mehta SR, Chrolavicius S, et al. Comparison of fondaparinux and enoxaparin in acute coronary syndromes. N Engl J Med. 2006;354(14):1464-1476.
202. Yusuf S, Mehta SR, Chrolavicius S, et al. Effects of fondaparinux on mortality and reinfarction in patients with acute ST-segment elevation myocardial infarction: the OASIS-6 randomized trial. JAMA. 2006;295(13):1519-1530.
203. Steg PG, Jolly SS, Mehta SR, et al. Low-dose vs standard-dose unfractionated heparin for percutaneous coronary intervention in acute coronary syndromes treated with fondaparinux: the FUTURA/OASIS-8 randomized trial. JAMA. 2010;304(12):1339-1349.
204. Oler A, Whooley MA, Oler J, Grady D. Adding heparin to aspirin reduces the incidence of myocardial infarction and death in patients with unstable angina: a meta-analysis. JAMA. 1996;276(10):811-815.
205. Hoenig MR, Aroney CN, Scott IA. Early invasive versus conservative strategies for unstable angina and non-ST elevation myocardial infarction in the stent era. Cochrane Database Syst Rev. 2010;3:CD004815.
206. Dolor RJ, Melloni C, Chatterjee R, et al (eds). Treatment Strategies for Women with Coronary Artery Disease. AHRQ Comparative Effectiveness Reviews. Report No. 66. Rockville, MD: Agency for Healthcare Research and Quality; 2012.
207. Fanning JP, Nyong J, Scott IA, Aroney CN, Walters DL. Routine invasive strategies versus selective invasive strategies for unstable angina and non-ST elevation myocardial infarction in the stent era. Cochrane Database Syst Rev. 2016;5:CD004815.
208. Navarese EP, Gurbel PA, Andreotti F, et al. Optimal timing of coronary invasive strategy in non-ST-segment elevation acute coronary syndromes: a systematic review and meta-analysis. Ann Intern Med. 2013;158(4):261-270.
209. Chan MY, Becker RC, Harrington RA, et al. Noninvasive, medical management for non-ST-elevation acute coronary syndromes. Am Heart J. 2008;155(3):397-407.
210. Carruthers KF, Dabbous OH, Flather MD, et al. Contemporary management of acute coronary syndromes: does the practice match the evidence? Heart. 2005;91:290-298.
211. Sonel AF, Good CB, Mulgund J, et al. Racial variations in treatment and outcomes of black and white patients with high-risk non-ST-elevation acute coronary syndromes: insights from CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the ACC/AHA Guidelines?). Circulation. 2005;111(10):1225-1232.
213. O'Donoghue M, Boden WE, Braunwald E, et al. Early invasive vs. conservative treatment strategies in women and men with unstable angina and non-ST-segment elevation myocardial infarction: a meta-analysis. JAMA. 2008;300(1):71-80.
214. Epstein AJ, Polsky D, Yang F, Yang L, Groeneveld PW. Coronary revascularization trends in the United States: 2001–2008. JAMA. 2011;305(17):1769-1776.
215. Smit Y, Vlayen J, Koppenaal H, Eefting F, Kappetein AP, Mariani MA. Percutaneous coronary invervention versus coronary artery bypass grafting: a meta-analysis. J Thorac Cardiovasc Surg. 2015;149(3):831-838.
216. Hannan EL, Racz MJ, Walford G, et al. Long-term outcomes of coronary-artery bypass grafting versus stent implantation. N Engl J Med. 2005;352(21):2174-2183.
217. Hannan EL, Wu C, Walford G, et al. Drug-eluting stents vs. coronary-artery bypass grafting in multivessel coronary disease. N Engl J Med. 2008;358(4):331-341.
218. Linn W, Wofford M, O'Keefe ME, Posey LM. Pharmacotherapy in Primary Care. New York, NY: McGraw Hill; 2009.
219. Wang SS. Coronary Artery Vasospasm Treatment and Management. Available at https://emedicine.medscape.com/article/153943-overview.153943-overview. Last accessed December 28, 2021.
220. Finkel JB, Marhefka GD. Rethinking cocaine-associated chest pain and acute coronary syndromes. Mayo Clin Proc. 2011;86(12):1198-1207.
221. Boden WE, Eagle K, Granger CB. Reperfusion strategies in acute ST-segment elevation myocardial infarction: a comprehensive review of contemporary management options. J Am Coll Cardiol. 2007;50(10):917-929.
222. Fox KAA, Steg PG, Eagle KA, et al. Decline in rates of death and heart failure in acute coronary syndromes, 1999–2006. JAMA. 2007;297(17):1892-1900.
223. Karam N, Bataille S, Marijon E, et al. Incidence, mortality, and outcome-predictors of sudden cardiac arrest complicating myocardial infarction prior to hospital admission. Circulation: Cardiovasc Intervention. 2019;12(1):e007081.
224. Stone GW. Angioplasty strategies in ST-segment-elevation myocardial infarction: part I: primary percutaneous coronary intervention. Circulation. 2008;118(5):538-551.
225. Krumholz HM, Herrin J, Miller LE, et al. Improvements in door-to-balloon time in the United States, 2005 to 2010. Circulation. 2011;124(9):1038-1045.
226. Cardiology Magazine. Door-to-Balloon 10 Years Later: Successful Model Sets the Stage for the Next Generation of ACC's QI Programs. Available at https://www.acc.org/latest-in-cardiology/articles/2016/11/29/10/30/door-to-balloon-10-years-later. Last accessed December 28, 2021.
227. Fitchett D. Tailored antithrombotic therapy for acute coronary syndromes. Expert Rev Cardiovasc Ther. 2008;6(7):935-944.
228. Bangalore S, Kumar S, Fusaro M, et al. Short- and long-term outcomes with drug-eluting and bare-metal coronary stents: a mixed-treatment comparison analysis of 117 762 patient-years of follow-up from randomized trials. Circulation. 2012;125(23):2873-2891.
229. Palmerini T, Biondi-Zoccai G, Della Riva D, et al. Clinical outcomes with drug-eluting and bare-metal stents in patients with ST-segment elevation myocardial infarction: evidence from a comprehensive network meta-analysis. J Am Coll Cardiol. 2013;62(6):496-504.
230. Palmerini T, Biondi-Zoccai G, Della Riva D, et al. Stent thrombosis with drug-eluting stents. Is the paradigm shifting? J Am Coll Cardiol. 2013;62(21):1-7.
231. Peng X, Qu W, Jia Y, Wang Y, Yu B, Tian J. Bioresorbable scaffolds: contemporary status and future directions. Front Cardiovasc Med. 2020;30:7:589571.
232. Wu X, Wu S, Kawashima H, et al. Current perspectives on bioresorbable scaffolds in coronary intervention and other fields.Expert Rev Med Devices. 2021;18(4):351-365.
233. Nallamothu BK, Bates ER, Herrin J, Wang Y, Bradley EH, Krumholz HM. Times to treatment in transfer patients undergoing primary percutaneous coronary intervention in the United States: National Registry of Myocardial Infarction (NRMI)-3/4 analysis. Circulation. 2005;111(6):761-767.
234. Cannon CP, Bahit MC, Haugland JM, et al. Underutilization of evidence-based medications in acute ST elevation myocardial infarction: results of the Thrombolysis in Myocardial Infarction (TIMI) 9 registry. Crit Pathw Cardiol. 2002;1(1):44-52.
235. Gibson CM, Pride YB, Frederick PD, et al. Trends in reperfusion strategies, door-to-needle and door-to-balloon times, and in-hospital mortality among patients with ST-segment elevation myocardial infarction enrolled in the National Registry of Myocardial Infarction from 1990 to 2006. Am Heart J. 2008;156(6):1035-1044.
236. Bowling A, Culliford L, Smith D, Rowe G, Reeves BC. What do patients really want? Patients' preferences for treatment for angina. Health Expect. 2008;11(2):137-147.
237. Ahmed S, Antman EM, Murphy SA, et al. Poor outcomes after fibrinolytic therapy for ST-segment elevation myocardial infarction: impact of age (a meta-analysis of a decade of trials). J Thromb Thrombolysis. 2006;21(2):119-129.
238. Sinnaeve P, Alexander J, Belmans A, et al. One-year follow-up of the ASSENT-2 trial: a double-blind, randomized comparison of single-bolus tenecteplase and front-loaded alteplase in 16,949 patients with ST-elevation acute myocardial infarction. Am Heart J. 2003;146(1):27-32.
239. Bode C, Smalling RW, Berg G, et al. Randomized comparison of coronary thrombolysis achieved with double-bolus reteplase (recombinant plasminogen activator) and front-loaded, accelerated alteplase (recombinant tissue plasminogen activator) in patients with acute myocardial infarction. The RAPID II Investigators. Circulation. 1996;94(5):891-898.
240. Wijeysundera HC, Vijayaraghavan R, Nallamothu BK, et al. Rescue angioplasty or repeat fibrinolysis after failed fibrinolytic therapy for ST-segment myocardial infarction: a meta-analysis of randomized trials. J Am Coll Cardiol. 2007;49(4):422-430.
241. Cannon CP, Gibson CM, McCabe CH, et al. TNK-tissue plasminogen activator compared with front-loaded alteplase in acute myocardial infarction: results of the TIMI 10B trial. Circulation. 1998;98(25):2805-2814.
242. Jinatongthai P, Kongwatcharapong J, Foo CY, et al. Comparative efficacy and safety of reperfusion therapy with fibrinolytic agents in patients with ST-segment elevation myocardial infarction: a systematic review and network meta-analysis. Lancet. 2017;39(10096):747-759.
243. Reynolds HR, Farkouh ME, Lincoff AM, et al. Impact of female sex on death and bleeding after fibrinolytic treatment of myocardial infarction in GUSTO V. Arch Intern Med. 2007;167(19):2054-2060.
244. Collet JP, Montalescot G, Le May M, Borentain M, Gershlick A. Percutaneous coronary intervention after fibrinolysis: a multiple meta-analyses approach according to the type of strategy. JAm Coll Cardiol. 2006;48(7):1326-1335.
245. Peters RJ, Mehta SR, Fox KA, et al. Effects of aspirin dose when used alone or in combination with clopidogrel in patients with acute coronary syndromes: observations from the Clopidogrel in Unstable angina to prevent Recurrent Events (CURE) study. Circulation. 2003;108(14):1682-1687.
246. Tungsubutra W, Chichareon P, Tresukosol D, et al. In-hospital outcomes after rescue percutaneous coronary intervention in patients with ST segment elevation myocardial infarction. J Med Assoc Thai. 2016;99(6):645-652.
247. Faslur Rahuman MB, Jayawardena JB, Francis GR, et al. A comparison of rescue and primary percutaneous coronary interventions for acute ST elevation myocardial infarction. Indian Heart J. 2017;(69 Suppl 1):S57-S62.
248. Levine GN, Bates ER, Bittl JA, et al. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines: an update of the 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention, 2011 ACCF/AHA guideline for coronary artery bypass graft surgery, 2012 ACC/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease, 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction, 2014 ACC/AHA guideline for the management of patients with non-ST-elevation acute coronary syndromes, and 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery. Circulation. 2016;134:e123-e155.
249. Gurm H, Tamhane U, Meier P, et al. A comparison of abciximab and small molecule glycoprotein IIb/IIIa inhibitors in patients undergoing primary percutaneous coronary intervention: a meta-analysis of contemporary randomized controlled trials. Circ Cardiovasc Intervent. 2009;2(3):230-236.
250. De Luca G, Ucci G, Cassetti E, et al. Benefits from small molecule administration as compared with abciximab among patients with ST-segment elevation myocardial infarction treated with primary angioplasty: a meta-analysis. J Am Coll Cardiol. 2009;53(18):1668-1673.
251. Dong L, Zhang F, Shu X. Early administration of small-molecule glycoprotein IIb/IIIa inhibitors before primary percutaneous coronary intervention for ST-elevation myocardial infarction: insights from randomized clinical trials. J Cardiovasc Pharmacol Ther. 2010;15(2):135-144.
252. Peters RJG, Joyner C, Bassand JP, et al. The role of fondaparinux as an adjunct to thrombolytic therapy in acute myocardial infarction: a subgroup analysis of the OASIS-6 trial. Eur Heart J. 2008;29(3):324-331.
253. Gharacholou SM, Alexander KP, Chen AY, et al. Implications and reasons for the lack of use of reperfusion therapy in patients with ST-segment elevation myocardial infarction: findings from the CRUSADE initiative. Am Heart J. 2010;159(5):757-763.
254. Silvain J, Beygui F, Barthélémy O, et al. Efficacy and safety of enoxaparin versus unfractionated heparin during percutaneous coronary intervention: systematic review and meta-analysis. BMJ. 2012;344:e553.
255. Grines CL, Bonow RO, Casey DE Jr, et al. Prevention of premature discontinuation of dual antiplatelet therapy in patients with coronary artery stents: a science advisory from the American Heart Association, American College of Cardiology, Society for Cardiovascular Angiography and Interventions, American College of Surgeons, and American Dental Association, with representation from the American College of Physicians. Circulation. 2007;115(6):813-818.
256. Cohen M, Boiangiu C, Abidi M. Therapy for ST-segment elevation myocardial infarction patients who present late or are ineligible for reperfusion therapy. J Am Coll Cardiol. 2010;55(18):1895-1906.
257. Alexander KP, Newby LK, Armstrong PW, et al. Acute coronary care in the elderly, part II: ST-segment-elevation myocardial infarction: a scientific statement for healthcare professionals from the American Heart Association Council on Clinical Cardiology: in collaboration with the Society of Geriatric Cardiology. Circulation. 2007;115(19):2570-2589.
258. Sugiyama T, Hasegawa K, Kobayashi Y, et al. Differential time trends of outcomes and costs of care for acute myocardial infarction hospitalizations by ST elevation and type of intervention in the United States, 2001–2011. J Am Heart Assoc. 2015;4(3):e001445.
259. Antman EM, Hand M, Armstrong PW, et al. 2007 focused update of the ACC/AHA 2004 guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: developed in collaboration With the Canadian Cardiovascular Society: endorsed by the American Academy of Family Physicians: 2007 Writing Group to Review New Evidence and Update the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction, writing on behalf of the 2004 Writing Committee. Circulation. 2008;117(2):296-329.
260. Douglas PS, Garcia MJ, Haines DE, et al. ACCF/ASE/AHA/ASNC/HFSA/HRS/SCAI/SCCM/SCCT/SCMR 2011 appropriate use criteria for echocardiography: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, American Society of Echocardiography, American Heart Association, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Critical Care Medicine, Society of Cardiovascular Computed Tomography, and Society for Cardiovascular Magnetic Resonance endorsed by the American College of Chest Physicians. J Am Coll Cardiol. 2011;57(9):1126-1166.
261. Roe MT, Parsons LS, Pollack CV Jr, et al. Quality of care by classification of myocardial infarction: treatment patterns for ST-segment elevation vs non-ST-segment elevation myocardial infarction. Arch Intern Med. 2005;165(14):1630-1636.
262. Cannon CP, Weintraub WS, Demopoulos LA, et al. Comparison of early invasive and conservative strategies in patients with unstable coronary syndromes treated with the glycoprotein IIb/IIIa inhibitor tirofiban. N Engl J Med. 2001;344(25):1879-1887.
263. Gibson CM. NRMI and current treatment patterns for ST-elevation myocardial infarction. Am Heart J. 2004;148(5 Suppl):S29-S33.
264. Latini R, Maggioni AP, Flather M, Sleight P, Tognoni G. ACE inhibitor use in patients with myocardial infarction: summary of evidence from clinical trials. Circulation. 1995;92(10):3132-3137.
265. ISIS-4 (Fourth International Study of Infarct Survival) Collaborative Group. ISIS-4: a randomised factorial trial assessing early oral captopril, oral mononitrate, and intravenous magnesium sulphate in 58,050 patients with suspected acute myocardial infarction. Lancet. 1995;345(8951):669-685.
266. Effect of verapamil on mortality and major events after acute myocardial infarction: the Danish Verapamil Infarction Trial II (DAVIT II). Am J Cardiol. 1990;66(10):779-785.
267. The Multicenter Diltiazem Postinfarction Trial Research Group. The effect of diltiazem on mortality and reinfarction after myocardial infarction. N Engl J Med. 1988;319(7):385-392.
268. The Danish Study Group on Verapamil in Myocardial Infarction. Verapamil in acute myocardial infarction. Eur Heart J. 1984;5(7):516-528.
269. Clark AM, McAlister FA, Hartling L, Vandermeer B. Randomized Trials of Secondary Prevention Programs in Coronary Artery Disease: A Systematic Review. Rockville, MD: Agency for Healthcare Research and Quality; 2005.
270. Anderson L, Taylor RS. Cardiac rehabilitation for people with heart disease: an overview of Cochrane systematic reviews. Cochrane Database Syst Rev. 2014;12:CD011273.
271. Smith SC Jr, Benjamin EJ, Bonow RO, et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update. Circulation. 2011;124:2458-2473.
272. Benowitz NL, Prochaska JJ. Smoking cessation after acute myocardial infarction. J Am Coll Cardiol. 2013;61(5):533-555.
273. Rigotti NA, Clair C, Munafò MR, Stead LF. Interventions for smoking cessation in hospitalised patients. Cochrane Database Syst Rev. 2012;5:CD001837.
274. Stead LF, Klilpillai P, Fanshawe TR, Lancaster T. Combined pharmacotherapy and behavioural interventions for smoking cessation. Cochrane Database Syst Rev. 2016;3:CD008286.
275. Yan AT, Yan RT, Tan M, et al. Optimal medical therapy at discharge in patients with acute coronary syndromes: temporal changes, characteristics, and 1-year outcome. Am Heart J. 2007;154(6):1108-1115.
276. Antithrombotics Trialists' Collaboration. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ. 2002;324(7329):71-86.
277. Tickoo S, Roe MT, Peterson ED. Patterns of aspirin dosing in non-ST-elevation acute coronary syndromes in the CRUSADE Quality Improvement Initiative. Am J Cardiol. 2007;99(11):1496-1499.
278. Depta JP, Bhatt DL. Aspirin and platelet adenosine diphosphate receptor antagonists in acute coronary syndromes and percutaneous coronary intervention: role in therapy and strategies to overcome resistance. Am J Cardiovasc Drugs. 2008;8(2): 91-112.
279. Braunwald E, Angiolillo D, Bates E, et al. Antiplatelet strategies: evaluating their current role in the setting of acute coronary syndromes. Clin Cardiol. 2008;31(Suppl I):I2-I9.
280. Ho PM, Peterson ED, Wang L, et al. Incidence of death and acute myocardial infarction associated with stopping clopidogrel after acute coronary syndrome. JAMA. 2008;299(5):532-539.
281. Ho PM, Tsai TT, Wang TY, et al. Adverse events after stopping clopidogrel in post-acute coronary syndrome patients: insights from a large integrated healthcare delivery system. Circ Cardiovasc Qual Outcomes. 2010;3(3):33-308.
282. Murphy SA, Cannon CP, Wiviott SD, et al. Effect of intensive lipid-lowering therapy on mortality after acute coronary syndrome (a patient-level analysis of the Aggrastat to Zocor and Pravastatin or Atorvastatin Evaluation and Infection Therapy—Thrombolysis in Myocardial Infarction 22 Trials). Am J Cardiol. 2007;100(7):1047-1051.
283. Afilalo J, Majdan AA, Eisenberg MJ. Intensive statin therapy in acute coronary syndromes and stable coronary heart disease: a comparative meta-analysis of randomised controlled trials. Heart. 2007;93(8):914-921.
284. Navarese EP, Kowalewski M, Andreotti F, et al. Meta-analysis of time-related benefits of statin therapy in patients with acute coronary syndrome undergoing percutaneous coronary intervention. Am J Cardiol. 2014;113(10):1753-1764.
285. Cannon CP, Blazing MA, Giugliano RP, et al. Ezetimibe added to statin therapy after acute coronary syndromes. N Engl J Med. 2015;372:2387-2397.
286. Whitehead DL, Strike P, Perkins-Porras L, Steptoe A. Frequency of distress and fear of dying during acute coronary syndromes and consequences for adaptation. Am J Cardiol. 2005;96(11):1512-1516.
287. Grace SL, Abbey SE, Kapral MK, Fang J, Nolan RP, Stewart DE. Effect of depression on five-year mortality after an acute coronary syndrome. Am J Cardiol. 2005;96(9):1179-1185.
288. Swenson JR, O'Connor CM, Barton D, et al. Influence of depression and effect of treatment with sertraline on quality of life after hospitalization for acute coronary syndrome. Am J Cardiol. 2003;92(11):1271-1276.
289. Naqvi TZ, Rafique AM, Andreas V, Rahban M, Mirocha J, Naqvi SS. Predictors of depressive symptoms post-acute coronary syndrome. Gend Med. 2007;4(4):339-351.
290. Rieckmann N, Gerin W, Kronish IM, et al. Course of depressive symptoms and medication adherence after acute coronary syndromes: an electronic medication monitoring study. J Am Coll Cardiol. 2006;48(11):2218-2222.
291. Kronish IM, Rieckmann N, Halm EA, et al. Persistent depression affects adherence to secondary prevention behaviors after acute coronary syndromes. J Gen Intern Med. 2006;21(11):1178-1183.
292. Buse JB, Ginsberg HN, Bakris GL, et al. Primary prevention of cardiovascular diseases in people with diabetes mellitus: a scientific statement from the American Heart Association and the American Diabetes Association. Diabetes Care. 2007;30(1):162-172.
293. Cheng K, Ingram N, Keenan J, Choudhury RP. Evidence of poor adherence to secondary prevention after acute coronary syndromes: possible remedies through the application of new technologies. Open Heart. 2015;2(1):e000166.
294. Bradley SM, Bryson CL, Maynard C, Maddox TM, Fihn SD. Recent hospitalization for non-coronary events and use of preventive medications for coronary artery disease: an observational cohort study. BMC Cardiovasc Disord. 2011;11:42.
295. Beatty AL, Li S, Thomas L, Amsterdam EA, Alexander KP, Whooley MA. Trends in referral to cardiac rehabilitation after myocardial infarction: data from the National Cardiovascular Data Registry 2007 to 2012. J Am Coll Cardiol. 2014;63(23):2582-2583.
296. Parashar S, Spertus JA, Tang F, et al. Predictors of early and late enrollment in cardiac rehabilitation, among those referred, after acute myocardial infarction. Circulation. 2012;126(13):1587-1595.
297. Peterson ED, Roe MT, Rumsfeld JS, et al. A call to ACTION (acute coronary treatment and intervention outcomes network): a national effort to promote timely clinical feedback and support continuous quality improvement for acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2009;2(5):491-499.
298. Condon C, McCarthy G. Lifestyle changes following acute myocardial infarction: patients' perspectives. Eur J Cardiovasc Nurs. 2006;5(1):37-44.
299. Fernandez RS, Davidson P, Griffiths R. Cardiac rehabilitation coordinators' perceptions of patient-related barriers to implementing cardiac evidence-based guidelines. J Cardiovasc Nurs. 2008;23(5):449-457.
300. Peterson ED, Roe MT, Mulgund J, et al. Association between hospital process performance and outcomes among patients with acute coronary syndromes. JAMA. 2006;295(16):1912-1920.
301. Booth JN 3rd, Levitan EB, Brown TM, Farkouh ME, Safford MM, Muntner P. Effect of sustaining lifestyle modifications (nonsmoking, weight reduction, physical activity, and mediterranean diet) after healing of myocardial infarction, percutaneous intervention, or coronary bypass (from the REasons for Geographic and Racial Differences in Stroke Study). Am J Cardiol. 2014;113(12):1933-1940.
302. Lewis WR, Ellrodt AG, Peterson E, et al. Trends in the use of evidence-based treatments for coronary artery disease among women and the elderly: findings from the Get With the Guidelines quality improvement program. Circ Cardiovasc Qual Outcomes. 2009;2(6):633-641.
303. Lee HY, Cooke CE, Robertson TA. Use of secondary prevention drug therapy in patients with acute coronary syndrome after hospital discharge. J Manag Care Pharm. 2008;14(3):271-280.
304. Gluckman TJ, Sachdev M, Schulman SP, Blumenthal RS. A simplified approach to the management of non-ST-segment elevation acute coronary syndromes. JAMA. 2005;293(3):349-357.
305. Birtcher KK, Pan W, LaBresh KA, Cannon CP, Fonarow GC, Ellrodt G. Performance achievement award program for Get With The Guidelines—Coronary Artery Disease is associated with global and sustained improvement in cardiac care for patients hospitalized with an acute myocardial infarction. Crit Pathw Cardiol. 2010;9(3):103-112.
306. Ho PM, Magid DJ, Shetterly SM, et al. Medication nonadherence is associated with a broad range of adverse outcomes in patients with coronary artery disease. Am Heart J. 2008;155(4):772-779.
307. Munger MA, Van Tassell BW, LaFleur J. Medication nonadherence: an unrecognized cardiovascular risk factor. Med Gen Med. 2007;9:58.
308. Kripalani S, Henderson LE, Jacobson TA, Vaccarino V. Medication use among inner-city patients after hospital discharge: patient-reported barriers and solutions. Mayo Clin Proc. 2008;83(5):529-535.
309. Kulkarni SP, Alexander KP, Lytle B, Heiss G, Peterson ED. Long-term adherence with cardiovascular drug regimens. Am Heart J. 2006;151(1):185-191.
310. Blackburn DF, Dobson RT, Blackburn JL, Wilson TW, Stang MR, Semchuk WM. Adherence to statins, beta-blockers and angiotensin-converting enzyme inhibitors following a first cardiovascular event: a retrospective cohort study. Can J Cardiol. 2005;21(6):485-488.
311. Ratner PA, Tzianetas R, Tu AW, et al. Myocardial infarction symptom recognition by the lay public: the role of gender and ethnicity. J Epidemiol Community Health. 2006;60(7):606-615.
312. Fukuoka Y, Dracup K, Moser DK, et al. Is severity of chest pain a cue for women and men to recognize acute myocardial infarction symptoms as cardiac in origin? Prog Cardiovasc Nurs. 2007;22(3):132-137.
313. Cooper H, Booth K, Fear S, Gill G. Chronic disease patient education: lessons from meta-analyses. Patient Educ Couns. 2001;44(2):107-117.
314. Kingsbury K. Taking AIM: how to teach primary and secondary prevention effectively. Can J Cardiol. 1998;14(Suppl A):22A-26A.
315. Boyd MD. Strategies for effective health teaching. In: Boyd MD, Graham BA, Gleit CJ, Whitman NI (eds). Health Teaching in Nursing Practice: A Professional Model. 3rd ed. Stanford, CT: Appleton and Lange; 1998:201-229.
316. Theis SL, Johnson JH. Strategies for teaching patients: a meta-analysis. Clin Nurse Spec. 1995;9(2):100-105, 120.
317. Wang WW. The educational needs of myocardial infarction patients. Prog Cardiovasc Nurs. 1994;9(4):28-36.
318. Finnegan JR Jr, Meischke H, Zapka JG, et al. Patient delay in seeking care for heart attack symptoms: findings from focus groups conducted in five U.S. regions. Prev Med. 2000;31(3):205-213.
319. Thuresson M, Jarlöv MB, Lindahl B, Svensson L, Zedigh C, Herlitz J. Factors that influence the use of ambulance in acute coronary syndrome. Am Heart J. 2008;156(1):170-176.
320. Herlitz J, Thuresson M, Svensson L, et al. Factors of importance for patients' decision time in acute coronary syndrome. Int J Cardiol. 2010;141(3):236-242.
321. Van Dongen JJJ, van Bokhoven MA, Daniels R, et al. Developing interprofessional care plans in chronic care: a scoping review. BMC Family Practice. 2016;17:1-9.
322. Donovan AL, Aldrich JM, Gross AK, et al. Interprofessional care and teamwork in the ICU. Crit Care Med. 2018;46:980-990.
1. O'Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.J Am Coll Cardiol. 2013;61(4):e78-e140. Available at https://www.ahajournals.org/doi/10.1161/CIR.0b013e3182742c84. Last accessed January 10, 2022.
2. American College of Cardiology Foundation, American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, et al. 2011 ACCF/AHA guideline for coronary artery bypass graft surgery: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American Association for Thoracic Surgery. J Am Coll Cardiol. 2011;58(24):e123-e210. Available at https://www.ahajournals.org/doi/full/10.1161/cir.0b013e31823c074e. Last accessed January 10, 2022.
Mention of commercial products does not indicate endorsement.