The course begins with an overview of risk management and related issues, emphasizing the need for primary care clinicians to establish risk management strategies in their practice. A definition of tort (personal-injury) law and several legal issues related to malpractice lay the foundation for a better understanding of such key concepts as medical negligence and the standard of care, adequate informed consent, statutes of limitations, and measure of damages. In addition, the course discusses malpractice-related laws such as apology statutes, good Samaritan laws, and charitable immunity laws; knowledge of these laws can help healthcare professionals better protect themselves from malpractice. Descriptions of the common characteristics of malpractice claims and the consequences of malpractice are included to enhance healthcare professionals' understanding of the underlying causes and motivations of malpractice claims and to improve their ability to handle a malpractice lawsuit. Tort reform is addressed to enable clinicians to become familiar with the proposed solutions to malpractice problems and participate in this national debate. The course closes with a brief discussion of the initial steps involved in responding to a malpractice claim and minimizing loss.
This course is designed for physicians, physician assistants, and nurse practitioners seeking to enhance their knowledge of risk management strategies, especially in the outpatient setting.
With patient safety as the priority, risk management should focus on the avoidance of medical errors, as they are, along with inadequate informed consent, the most common assertions in malpractice claims in the United States. The purpose of this course is to provide healthcare professionals with the information necessary to engage in risk management practices, including a variety of proven strategies to avoid malpractice.
Upon completion of this course, you should be able to:
- Define the most important issues and trends related to risk management and malpractice.
- Define the key concepts in malpractice.
- Outline malpractice-related laws, such as Good Samaritan laws, charitable immunity laws, and apology statutes.
- Identify the most common underlying causes and characteristics of malpractice claims.
- Describe the consequences of malpractice with respect to healthcare delivery and personal and professional effects on physicians.
- Describe measures to enhance patient-physician communication, ensure appropriate disclosure of errors to patients, and guarantee adequate informed consent.
- Develop efficient office processes to enhance documentation, diagnosis, test tracking, medication management, and other issues.
Lori L. Alexander, MTPW, ELS, MWC, is President of Editorial Rx, Inc., which provides medical writing and editing services on a wide variety of clinical topics and in a range of media. A medical writer and editor for more than 30 years, Ms. Alexander has written for both professional and lay audiences, with a focus on continuing education materials, medical meeting coverage, and educational resources for patients. She is the Editor Emeritus of the American Medical Writers Association (AMWA) Journal, the peer-review journal representing the largest association of medical communicators in the United States. Ms. Alexander earned a Master’s degree in technical and professional writing, with a concentration in medical writing, at Northeastern University, Boston. She has also earned certification as a life sciences editor and as a medical writer.
Contributing faculty, Lori L. Alexander, MTPW, ELS, MWC, has disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
John M. Leonard, MD
John V. Jurica, MD, MPH
The division planners have disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
Sarah Campbell
The Director of Development and Academic Affairs has disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
The purpose of NetCE is to provide challenging curricula to assist healthcare professionals to raise their levels of expertise while fulfilling their continuing education requirements, thereby improving the quality of healthcare.
Our contributing faculty members have taken care to ensure that the information and recommendations are accurate and compatible with the standards generally accepted at the time of publication. The publisher disclaims any liability, loss or damage incurred as a consequence, directly or indirectly, of the use and application of any of the contents. Participants are cautioned about the potential risk of using limited knowledge when integrating new techniques into practice.
It is the policy of NetCE not to accept commercial support. Furthermore, commercial interests are prohibited from distributing or providing access to this activity to learners.
Supported browsers for Windows include Microsoft Internet Explorer 9.0 and up, Mozilla Firefox 3.0 and up, Opera 9.0 and up, and Google Chrome. Supported browsers for Macintosh include Safari, Mozilla Firefox 3.0 and up, Opera 9.0 and up, and Google Chrome. Other operating systems and browsers that include complete implementations of ECMAScript edition 3 and CSS 2.0 may work, but are not supported. Supported browsers must utilize the TLS encryption protocol v1.1 or v1.2 in order to connect to pages that require a secured HTTPS connection. TLS v1.0 is not supported.
The role of implicit biases on healthcare outcomes has become a concern, as there is some evidence that implicit biases contribute to health disparities, professionals' attitudes toward and interactions with patients, quality of care, diagnoses, and treatment decisions. This may produce differences in help-seeking, diagnoses, and ultimately treatments and interventions. Implicit biases may also unwittingly produce professional behaviors, attitudes, and interactions that reduce patients' trust and comfort with their provider, leading to earlier termination of visits and/or reduced adherence and follow-up. Disadvantaged groups are marginalized in the healthcare system and vulnerable on multiple levels; health professionals' implicit biases can further exacerbate these existing disadvantages.
Interventions or strategies designed to reduce implicit bias may be categorized as change-based or control-based. Change-based interventions focus on reducing or changing cognitive associations underlying implicit biases. These interventions might include challenging stereotypes. Conversely, control-based interventions involve reducing the effects of the implicit bias on the individual's behaviors. These strategies include increasing awareness of biased thoughts and responses. The two types of interventions are not mutually exclusive and may be used synergistically.
#41474: Risk Management
Risk management in the healthcare professions refers to strategies designed to enhance patient safety, decrease the risk of malpractice claims, and minimize loss. Effective risk management is essential not only because of the inherent value of patient safety but also because of the high prevalence of malpractice claims, which exact great costs in terms of money, time, and personal and professional losses[1,2].
Healthcare institutions implement interdisciplinary risk management programs to ensure that high-quality medical care is provided to patients and to reduce the risk of malpractice claims brought against the institution and/or its attending physicians and other healthcare professionals. While physicians in surgery and obstetrics/gynecology are most likely to be named in a malpractice suit, primary care physicians in private practice are very vulnerable to malpractice claims and often face greater professional and personal consequences of a malpractice suit [3,4,5]. Thus, this course primarily addresses risk management programs for healthcare providers in private practice.
The course begins with a definition of risk management, emphasizing the need for primary care physicians to establish risk management strategies in their practice. A definition of tort (personal-injury) law and several legal issues related to malpractice lay the foundation for a better understanding of such key concepts as medical negligence and the standard of care, adequate informed consent, and malpractice-related laws such as apology statutes, Good Samaritan laws, and charitable immunity laws. The focus is on the issues that cause the most common allegations in malpractice claims in the United States [6].
Descriptions of the common characteristics of malpractice claims and the consequences of malpractice are included to enhance healthcare professionals' understanding of the underlying causes and motivations of malpractice claims. Such an understanding can help physicians develop targeted risk management strategies and enhance patient safety, and a variety of proven strategies to avoid malpractice are discussed.
Risk management is a program of strategies to minimize the risk of harm to patients and to decrease the healthcare provider's exposure to liability. An effective risk management program includes both proactive and reactive components [7]. The proactive component consists of strategies to prevent adverse occurrences, and the reactive component includes strategies for responding to such occurrences (i.e., minimizing loss). Minimizing loss involves developing a process to handle a malpractice claim as efficiently as possible. Quality assurance is also an important factor in risk management, as improving the quality of medical care is the theoretical underpinning of avoiding malpractice [8].
The following are among the most important issues related to risk management [9]:
Communication (with patients and among staff and other healthcare professionals)
Missed appointments
Follow-up on test results
Documentation
Management of medications
Patient satisfaction
Scope of practice
Disruptive patients
Patient termination
Medical record retention
In addition, in 2014, the American Society for Healthcare Risk Management developed a holistic approach to risk management called enterprise risk management that includes traditional reactive strategies combined with proactive strategies. The following eight risk domains make up enterprise risk management [10]:
Operational
Clinical and patient safety
Strategic
Financial
Human capital
Legal and regulatory
Technological
Environmental- and infrastructure-based hazards
Surveys of medical office practices have shown that problems related to risk management are common across all physician specialties [5]. These problems warrant attention and improvement efforts not only because they are associated with a risk of malpractice but also because they have the potential for causing medical errors, which have been reported to be highly prevalent and highly preventable [11]. An overall understanding of malpractice and its key components is needed to provide a framework for defining and discussing effective risk management strategies.
Physicians are the primary target of malpractice. According to records of malpractice payments in 2024, 81.9% of payments were made in claims against physicians and dentists; professional nurses accounted for 7.9%, and all other healthcare practitioners constituted 10.0% [12]. In total, 34% of physicians have been sued, with 16.8% having been sued more than twice [13]. Lower quality of care does not appear to be the cause of most malpractice claims, as no significant differences have been found in quality between physicians who have and have not been sued [14].
For physicians in low-risk specialties (e.g., pediatrics, psychiatry), there is a substantial gap between physicians' perceived risk of malpractice and their actual risk, with physicians perceiving a much greater risk of malpractice than has been documented for their specialty [15,16]. For example, in a survey regarding malpractice concerns, 62.5% of pediatric physicians agreed or strongly agreed that they were at risk, compared with American Medical Association (AMA) data that indicated 17.8% of pediatric physicians had ever been sued [13,17]. Similarly, radiologists have estimated their risk of litigation within five years as 35%, which compares with an actual rate of approximately 10% [15]. By contrast, using the same datasets, physicians in high-risk specialties (i.e., obstetrics/gynecology and surgery) had a much closer concern/reality gap, with concern data showing 81% for obstetricians/gynecologists and 75.3% for surgical specialists, compared with a lifetime malpractice claim rate of 63.6% and 63.2%, respectively [13,17].
The risk of malpractice varies among medical specialties and typically increases with the frequency with which procedures are performed and with a greater potential for catastrophic injury [5,18]. The rates of malpractice claims against family medicine and internal medicine physicians have historically been low, but the rates have increased since the late 1990s [19]. According to paid claims between 1992 and 2014, family medicine and internal medicine were the specialties with the second and third leading number of claims (behind obstetrics/gynecology), with 18,349 and 17,174 paid claims, respectively (Table 1) [5]. It has been estimated that the typical family physician can expect to be sued about once every 7 to 10 years [20]. One study noted that by 65 years of age, 75% of physicians in low-risk specialties faced a malpractice claim, compared with 99% of physicians in high-risk specialties. It should be noted, however, that more than 75% of these malpractice claims do not result in indemnity payment [21]. In an analysis of overall paid malpractice claims between 1992 and 2014, it was found that the rate of paid claims decreased by 55.7%; however, the mean payment amount increased by 23.3% (Table 1) [5].
ANNUAL PAID MALPRACTICE CLAIMS ACCORDING TO SPECIALTY, 1992–2014
| Specialty | Total Paid Claimsa | Mean Payment |
|---|---|---|
| Obstetrics and gynecology (includes surgery) | 20,060 | $432,959 |
| Family medicine | 18,349 | $290,698 |
| Internal medicine | 17,174 | $318,071 |
| General surgery | 12,981 | $298,625 |
| Orthopedics (includes surgery) | 10,641 | $258,763 |
| Radiology | 9,079 | $333,422 |
| Emergency medicine | 8,007 | $309,411 |
| Anesthesiology | 7,892 | $377,499 |
| Pediatrics | 5,799 | $413,974 |
| Cardiology (includes surgery) | 5,378 | $365,029 |
| General practice | 4,435 | $231,622 |
| Ophthalmology | 4,044 | $244,039 |
| Urology (includes surgery) | 3,631 | $23,290 |
| Otolaryngology | 3,226 | $282,822 |
| Plastic surgery | 3,156 | $189,219 |
| Psychiatry | 3,115 | $238,909 |
| Gastroenterology | 2,881 | $349,013 |
| Neurosurgery | 2,797 | $469,222 |
| Pathology | 2,372 | $411,529 |
| Thoracic surgery | 2,179 | $380,402 |
| Neurology (nonsurgical) | 2,156 | $431,049 |
| Otorhinolaryngology | 1,081 | $282,822 |
| Dermatology | 1,717 | $189,065 |
| Colon and rectal surgery | 549 | $337,976 |
| aIncludes physicians with more than one paid claim. | ||
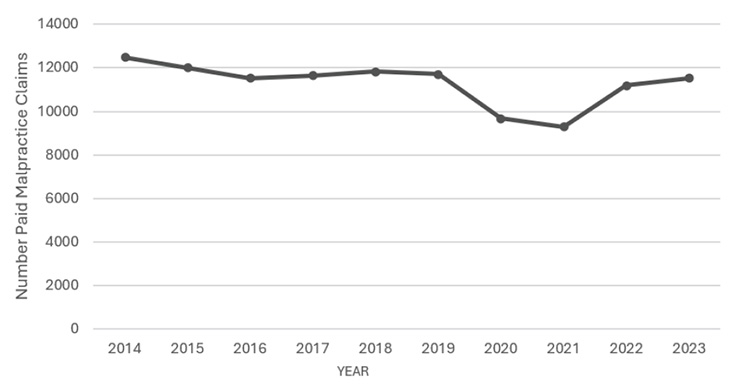
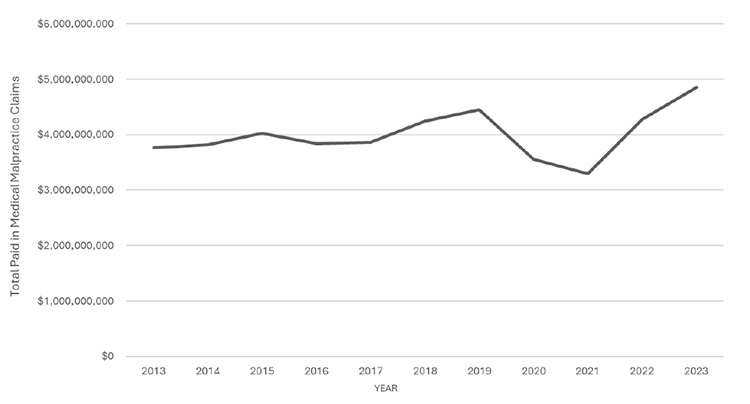
Overall rates of medical malpractice claims declined between 2010 and 2020. The same trend occurred in the number of paid malpractice claims and the average compensation (Figure 1 and Figure 2) [12]. In 2023, 50,404 malpractice claims were paid in the United States, with the compensation totaling more than $4.8 billion [12]. It has been argued that malpractice claims represent a substantial factor in rising healthcare costs. However, estimates for 2010 demonstrate that the total costs related to malpractice claims (compensation plus administrative costs) represented only 0.23% (range: 0.13% to 0.33%) of the $2.8 trillion (range: $2.6 trillion to $3 trillion) spent on health care in the United States that year [22].
The average compensation varies widely according to geography, type of injury, and physician specialty. In 2023, the average compensation ranged from $3.14 million (North Dakota) to $616 million (New York) [12]. Total compensation also varies considerably. In 2023, compensations in New York State accounted for 11% of all payments that year in the United States, and the top six states (New York, Pennsylvania, New Jersey, Illinois, Florida, and California) accounted for more than half of all 2023 compensation payments [12]. Claims payments are typically lowest for "insignificant injury" (average of $35,605 in 2022) and highest for quadriplegia, brain damage, or lifelong care (average of $939,475 in 2022) [23]. Of 24 specialties, general and family medicine ranks 18th in mean compensation (approximately $290,698) and internal medicine ranks 14th (approximately $318,071) [5].
Malpractice draws a great deal of attention by the public at large, but the actual number of malpractice claims that are filed is lower than the number of individuals who seek legal advice about a medical issue, and the number of claims that are won is still lower. One study found that in closed claims between 2016 and 2018, 65% were dropped, dismissed, or withdrawn. In addition, only 6% of claims were decided by a trial verdict, and of these, 89% were won by the defendant [24]. Additionally, a 2021 survey of physicians with a malpractice claim indicated that the result of the lawsuit was settled before trial (33%); dismissed within first few months (13%); verdict in physician's favor (10%); ongoing or in process (7%); dismissed prior to settling (6%); dismissed by court (6%); dismissed prior to trial (6%); voluntarily dismissed by plaintiff prior to trial (6%); verdict in plaintiff's favor (2%); and settled at trial (2%) [4].
The primary goals of the U.S. medical malpractice system are to compensate individuals who have been harmed through medical negligence, to hold a responsible individual accountable, and to provide deterrence to unsafe medical practices or medical errors [8,25]. (The AMA defines a medical error as an "unintended act or omission, or a flawed system or plan, that harms or has the potential to harm a patient" [26].) According to the 2000 landmark Institute of Medicine report, To Err is Human: Building a Safer Health System, 44,000 to 98,000 deaths are caused by medical errors in U.S. hospitals each year, with more than 7,000 of those deaths attributable to medication errors [11]. In addition, a national survey conducted in 2017 indicated that 21% of patients personally experienced a medical error, and 31% have personally been involved in the care of someone who has experienced an error. Combined, 41% of individuals surveyed experienced or were involved in a medical error [27]. However, the true number of adverse outcomes attributable to medical errors or negligence is difficult to determine. In a large study of hospital discharge records and malpractice claims, researchers determined that only 17% of claims involved an injury caused by medical negligence and that there were 7.6 times as many negligent injuries as there were claims, with only 2% of negligent injures resulting in claims [28]. A later study of 1,452 closed malpractice claims demonstrated that 37% did not involve a medical error, and the findings of another study indicated that more than three-quarters of 26,126 malpractice claims against primary care physicians were not considered to involve negligence [2,3]. A separate analysis of four major studies on lethal medical errors indicated that in 2013 there were 251,454 preventable deaths due to medical error [29]. However, this was quickly debated and an estimate of 174,901 preventable deaths was given after adjusting for perceived biases [30]. In either case, medical error was still found to be the third leading cause of death in the United States [29,30]. These results show the difficulty in determining the true number of medical errors and indicate that most patients who sustain a medical injury as a result of medical negligence do not sue and that a substantial number of claims do not involve negligence, which leaves the primary goals of the malpractice system unmet [2,28,31,32]. Calls for reform of the malpractice system have been made in light of these findings, and several organizations, including the AMA, have taken steps toward medical liability reform, with the goal of creating an accurate and fair liability process, while ensuring patient access to physicians and a full range of healthcare services [24].
Medical malpractice is processed in the civil court system or according to tort law. Overall, the civil court system provides a mechanism for an individual or group to recover damages when a tort (derived from the French word for "wrong") is committed against a person or property. Torts are classified as either intentional or negligent. Several intentional torts may be committed by physicians, including assault and battery (e.g., operating on a patient without informed consent), false imprisonment (e.g., forcing a patient to stay in the office until a bill is paid), and fraud (e.g., claiming cure when the physician knows cure is not possible) [33]. A negligent tort involves the omission or commission of an act that a reasonably prudent person would or would not do under given circumstances [34].
The statutes of limitations for medical malpractice vary according to the state, with many states having statutes that vary by cause of action and special rules for minors. In general, a medical claim must be filed within 1 to 5 years after the malpractice occurred or after the alleged injury was discovered if it was not immediately evident.
In a medical malpractice case, the plaintiff has the burden of establishing the appropriate standard of care and demonstrating that the standard of care has been breached. The standard of care is primarily defined by other practitioners with similar qualifications, who provide expert testimony about how they would have managed an individual's care under the same or similar circumstances [35]. In general, expert testimony is based on the physician expert's knowledge, skill, experience, and training and may be supplemented by published literature, practice guidelines, and surveys of practitioners [35]. The focus is whether the physician's actions met or breached the standard of care and, if the latter, whether the plaintiff was harmed as a result of the breach [35].
According to tort law, four elements must be established for a ruling of malpractice [34,36]:
Duty: The physician owed a duty to meet a particular standard of care.
Breach of duty: The physician failed to perform the owed duty.
Causation: There is a causal connection between the physician's failure and the patient's injury.
Damages: An injury occurred for which monetary compensation is adequate relief.
These elements must be shown by a "preponderance of the evidence," defined as more than 50% probability, a lower standard than the "beyond a reasonable doubt" used in criminal law [35,37]. Malpractice cases are decided on the basis of what a "jury is likely to think is fact" rather than actual fact [38,39].
A duty is owed if there is an active patient-physician relationship at the time of alleged injury [34]. This relationship is defined as any service given by a provider to an individual, whether in the provider's office, in an emergency department, or within a telephone discussion [34]. Breach of duty can be claimed if the healthcare provider does not meet a relevant standard of care or there is an obvious error (e.g., retained surgical instruments). Causation requires that the plaintiff establishes that the physician's negligence led to the stated injury; an association can be interpreted as causation by a jury who may be sympathetic to the plaintiff [34]. Damages sustained by the patient are compensatory and/or punitive. Compensatory damages consist of compensation for directs costs, such as for lost earnings and medical expenses (current and future), as well as compensation for indirect costs, such as pain, emotional distress, and loss of consortium. Punitive damages are awarded to a plaintiff when the physician's actions are found to be intentionally harmful or grossly negligent [34].
The informed consent law in medicine was originally developed from battery, an intentional tort [36]. The definition of battery as unwanted physical touching of the body by others was extended to include a treatment provided by a physician without a patient's consent [36]. Battery was also applied to cases in which the procedure performed was substantially different from the one for which consent was given, in which the procedure exceeded the scope of the consent, or in which the procedure was performed by a physician other than the one to whom consent was given [36]. Cases of medical informed consent are now classified as negligence, carrying with it the burden to prove the four elements for liability [36,40].
The primary goal of informed consent is to protect patients by requiring that physicians provide a balanced discussion of a proposed procedure/treatment as well as of the alternative options, so patients can make informed medical decisions [36]. Informed consent was once required only for invasive procedures but the scope of procedures has expanded to include complex treatments (e.g., radiation therapy, chemotherapy), and a separate written consent is required for the use of anesthesia (general, spinal/epidural, or regional) in some states [6,40,41].
The informed consent discussion should focus on the expected benefits, the risks involved with the procedure/treatment, and the feasible alternatives [6,40]. The adequacy of the disclosure of risks is defined differently among states. In most states, a "professional standard" is applied, which means that adequate disclosure is defined as what a reasonable medical practitioner would disclose in a similar situation; in other states, a "lay standard" is applied, with adequate disclosure defined as what a reasonably prudent individual would want to know before consenting to the particular procedure/treatment [6]. In general, physicians must disclose all severe risks, such as death, paralysis, or loss of an extremity, regardless of the likelihood of the event. Less severe events should be disclosed if they are frequent, whereas nominal risks do not need to be disclosed if they are not frequent [36,40].
The Centers for Medicare and Medicaid Services (CMS) mandates that all medical records (inpatient and outpatient) contain completed written informed consent forms for all procedures and treatments [41]. In 2007, CMS issued new interpretive guidelines for informed-consent documentation in patients' medical records. According to these guidelines, informed consent is defined as, "the patient or patient representative is given (in a language or means of communication he/she understands) the information, explanations, consequences, and options needed in order to consent to a procedure or treatment" [41]. In 2024, the CMS issued an update to informed consent guidance for hospitals [42,43]. The update clarifies the need to obtain informed consent from patients and expands it to include medical or other students who perform important surgical tasks or sensitive or invasive procedures or examinations. This update was based on increasing concerns about the absence of informed patient consent prior to allowing medical practitioners or students to perform training- or education-related exams that are outside the medically necessary procedure [42,43].
Several laws have been established to provide healthcare professionals specific types of protection against legal liability. These laws, which include Good Samaritan laws, charitable immunity laws, and apology statutes, vary by state.
Good Samaritan laws, also known as volunteer protection laws, were enacted to protect individuals from being sued as a result of voluntarily rendering emergency aid to an injured person [44,45]. A "volunteer" can help an injured person on the grounds of implied consent, but if the person is conscious and can respond, first asking permission to help him or her is recommended [44]. In most states, a person is not legally obligated to provide first aid (unless it is part of a job description), but when such aid is provided, the person giving aid has a duty to be reasonably careful [44]. Good Samaritan laws protect a volunteer against legal liability in the event he or she makes an error during the provision of emergency care [44]. Some Good Samaritan laws may hold the volunteer liable if he or she does not act to assist during an emergency. Whether the volunteer chooses to act or not, the important consideration is to act in a manner that will not render the volunteer liable [44].
Charitable immunity laws are designed to protect physicians and other healthcare professionals who volunteer their services in free health clinics and other community initiatives to provide health care to uninsured individuals. These laws also differ from state to state, but they act to either raise the negligence standard of care (from simple negligence to gross negligence) or indemnify volunteer healthcare professionals with liability protection as if they were government employees [46]. Some state laws have elements of both approaches.
Requiring evidence of gross negligence (defined as "willful," "wanton," or "reckless" negligence) makes it more difficult to prove medical negligence [47]. States that indemnify volunteer healthcare professionals as government employees have a legal defense fund to cover defense costs and monetary damages; in some cases, there is an established limit on the total amount of compensation that can be paid [47]. Thus, such indemnification, also known as the State Tort Claims Act, can help to limit loss. In addition to state statutes, federal legislation also protects healthcare professionals who provide free health care.
The Volunteer Protection Act of 1997 provides protection against liability for a volunteer clinician "acting within his or her scope of duties in a nonprofit organization" [46]. This law also limits punitive damages to cases in which there is clear and convincing evidence of willful or criminal misconduct or conscious, flagrant indifference to the rights or safety of the individual harmed [46]. All states had laws limiting liability of certain volunteers at the time the Volunteer Protection Act was adopted, and these laws are not preempted if they provide additional protections [48].
Although state and federal charitable immunity laws do not guarantee that a malpractice claim will not be filed, the laws appear to have limited the number of malpractice claims, as physicians in volunteer settings are rarely targets of malpractice claims [47].
Apology statutes are designed to promote disclosure of medical errors by protecting physicians who apologized for an error. According to these laws, expressions of apology made after a medical error are excluded from evidence in a malpractice suit. There are two types of apology statutes [49]:
Sympathy only: protects a physician's expression of sympathy, regret, and condolence
Admission of fault: protects a physician's admission of fault and error (in addition to expressions of sympathy, regret, and condolence)
Massachusetts was the first state to enact an apology law, in 1986. Since then, apology laws have been enacted in 39 states and the District of Columbia. These states have enacted one of the two types of apology statutes, but the majority of states have adopted the sympathy only law [49,50,51,52]. As of 2022, six states have provisions that specifically relate to accidents [52]. However, physicians are often skeptical of apologizing for potential error or adverse outcomes. In a 2021 survey of physicians with malpractice suits, 79% indicated that apologizing would not have made a difference, while only 2% indicated that it would have [4].
Closed malpractice claims have been used in a host of studies to gain a better understanding of the specific factors associated with claims. Data on medical malpractice claims are found in three primary sources, and each source provides slightly different types of data. The most comprehensive source of claims information is the National Practitioner's Data Bank (NPDB), maintained by the U.S. Department of Health and Human Services [12]. The Health Care Quality Improvement Act of 1986 requires that all payments in settlement of malpractice claims must be reported to this system. The drawback to this source is that only claims that have been paid are included. Another source is the Medical Professional Liability (MPL) Association (formerly Physician Insurers Association of America) data sharing project. The MPL Association is a trade association of more than 50 medical malpractice insurance companies that represent more than two-thirds of private practice physicians and 2,500 hospitals, and the data represent approximately 25% of the medical malpractice claims in the United States at a given time [53]. The MPL Association includes both paid and unpaid claims, and queries on physician specialty can be carried out. The third source is Jury Verdicts on Westlaw; this source has limited value, as the number of malpractice claims that are decided by jury verdict is small [54].
Studies of malpractice claims have provided valuable information on the most common underlying causes of alleged injuries/events (also known as "medical misadventures") and the diagnoses at highest risk for malpractice. Additional studies have identified a wide variety of factors that motivate individuals to file a malpractice claim. Understanding the risk factors and patient motivators for malpractice can help physicians develop risk management strategies that address the most common issues related to patient safety.
Diagnostic error (misdiagnosis or missed or delayed diagnosis) is the most common allegation in malpractice claims, noted in 22% to 78% of all claims [2,3,5,16,55,56]. In a study of 307 claims alleging diagnostic error in the ambulatory setting, researchers found that 59% of the claims involved a diagnostic error that harmed the patient [57]. Among the errors that caused harm, 59% caused serious harm and 30% caused death [57]. Another study analyzing paid claims noted that there was a substantial difference in paid claims for diagnostic errors among specialties. The percentage of paid claims for which diagnostic error was alleged was highest among pathology (87%) and radiology (83.9%), and lowest among anesthesiology (3.5%) and plastic surgery (4.3%) [5].
Although "failure in judgment" is usually a contributing factor for diagnostic errors, most errors involve several contributing factors [58,59,60]. The origins of diagnostic errors are multifaceted and may involve communication problems, system-related problems (e.g., lack of supervision, workload, technology issues), physician-related factors (e.g., stress, fatigue, hurriedness), patient-related factors, or a combination of any of these [57,58,61,62]. Researchers have narrowed the diagnostic process down to seven stages, with diagnostic errors occurring in one or more of these stages [62]:
Access and presentation
History taking/collection
Physical exam
Testing
Assessment
Referral
Follow-up
One study in the primary care setting noted that diagnostic process breakdown most frequently occurred during the patient-practitioner clinical encounter (78.9%), which includes errors in history-taking (56.3%), examination (47.4%), and/or ordering diagnostic tests for further work-up (57.4%). Other areas of process breakdown included referrals (19.5%), patient-related factors (16.3%), follow-up and tracking of diagnostic information (14.7%), and performance and interpretation of diagnostic tests (13.6%). A total of 43.7% of cases involved more than one of these processes [63].
Medication errors and adverse drug events represent 6.3% of malpractice claims, and the adverse event has been considered to be preventable in approximately 28% to 73% of claims [64,65,66]. Most medication errors do not cause adverse events, but when they do, serious harm may be the result; 38% to 46% of adverse drug events were reported to be life-threatening or fatal [64,65].
A variety of other underlying causes have been identified, including delayed or inappropriate treatment, failure to supervise or monitor the case, improper performance of procedure, failure/delay in referral, and failure to recognize complications of treatment [2,3,58,67,68]. In one analysis of 596 closed claims, 364 (67%) were diagnosis-related events [68]. Other allegations were related to improper inspection/maintenance of equipment (13%); improper performance of treatment or procedure (5%); improper management of treatment course (3%); failure to ensure patient safety (1%), retained foreign body (1%), and wrong or unnecessary treatment or procedure (1%) [68].
Diagnoses
The leading diagnoses-related allegations have varied somewhat across studies. One analysis of hospital medicine malpractice found that 40% of allegations were failure to diagnose, with the remainder (50%) due to improper procedure and treatment issues [69]. Of the diagnosis-related claims, the most common diagnosis was pulmonary embolism with infarction (6%). Factors that contributed to patient injury in these claims included failure to order diagnostic tests; failure to establish a differential diagnosis; failure to appreciate/reconcile relevant signs, symptoms, and test results; insufficient documentation of clinical rationale; and premature discharge [69]. In another study of claims settled between 1985 and 2000, acute myocardial infarction was the leading diagnosis (5%), followed by lung, breast, and colon cancer (each accounted for 3% of claims) and appendicitis (2%) [3]. Another study of missed diagnoses in the primary care setting found that more than 35% of missed diagnoses were conditions common in primary care, including pneumonia (6.7%), decompensated congestive heart failure (5.7%), acute renal failure (5.3%), cancer (primary) (5.3%), and urinary tract infection or pyelonephritis (4.8%) [63]. Diagnostic errors are also a predominant source of emergency department allegations (37%) [70]. A 2010 study identified the most common conditions associated with emergency department claims, with fractures (6%), acute myocardial infarction (5%), and appendicitis (2%) topping the list [70].
In a review of 307 claims of diagnosis error in an ambulatory setting, cancer accounted for 59% of the missed or delayed diagnoses; breast cancer was the leading type of cancer (24%), followed by colorectal cancer (7%), and skin, gynecologic, and hematologic cancers (4% each) [57]. Other diagnoses frequently missed or delayed according to that review were infection (5%), myocardial infarction (4%), and fractures (4%) [57].
Patient Motivations
Given that a high number of malpractice claims do not involve a medical injury, other factors must motivate patients and families to sue [18,71]. Patient motivations for malpractice have been extensively studied, and a wide variety of motivations have been identified (Table 2) [18,58,71,72]. In general, these motivations are not related to financial need but rather to problems with patient-physician communication or the patient-physician relationship and unmet expectations of the patient [71]. The overwhelming majority of patients and families say they just want information about what happened, and many wish to prevent the situation from happening again [18,71,73].
SPECIFIC REASONS INDIVIDUALS GIVE FOR FILING A MALPRACTICE CLAIM
|
Malpractice exacts a substantial cost on healthcare delivery, physicians, and patients. The fear of litigation alone (real or perceived) has led many physicians to reconsider their profession. For example, the risk of litigation has prompted one-third of radiologists to consider leaving the field of breast imaging [15]. Fear of malpractice also influences physicians' practice behaviors, primarily through the use of defensive medicine. The legal process involved with a malpractice claim takes physicians away from patient care and their families, a burden that is heightened by the amount of time required for resolution of a case.
The threat of malpractice—real or perceived—has been shown to affect clinical decision making, prompting many physicians to practice so-called defensive medicine, or care based primarily on avoidance of litigation rather than on defined clinical need [4,16,74,75]. Defensive medicine has been defined in two categories: "assurance behavior" or "avoidance behavior" [8,16]. Assurance behavior, referred to as "positive defensive medicine," involves excessive ordering of tests and hospitalization of patients and referrals for consultations; avoidance behavior, referred to as "negative defensive medicine," involves decreasing the delivery of high-risk services or declining to treat high-risk patients [8,16,17,25,74,76,77].
The use of defensive medicine has been evaluated among general practitioners as well as several physician specialties and has been found to be widely prevalent [25]. Surveys of urologists have shown that 77% have practiced defensive medicine, with 58% to 60% saying they had considered referring difficult cases and/or limiting the scope of their practice because of the threat of malpractice [8]. Neurologists with higher malpractice concerns were found to order more tests in clinical scenarios related to seizures and Alzheimer disease [17]. A survey of defensive practices among 1,028 neurosurgeons found that 72% ordered additional imaging studies, 67% ordered additional laboratory tests, 66% referred patients to consultants, and 40% prescribed medication. Forty-five percent of respondents reported eliminating high-risk procedures from their practices [78]. Among emergency physicians, the fear of malpractice accounted for significant variability in decision making, especially with regard to individuals with chest pain, and was associated with the increased use of diagnostic tests and the increased hospitalization of low-risk patients [76]. These findings are consistent with those from broad samples of physicians. In a survey of 824 physicians in six high-risk specialties (i.e., emergency medicine, general surgery, orthopedic surgery, neurosurgery, obstetrics/gynecology, radiology), 93% of respondents reported practicing defensive medicine, and a survey of 2,416 physicians, conducted by Mount Sinai School of Researchers, found that 91% of physicians said they practiced defensive medicine [77,79]. A national survey of 1,214 orthopedic surgeons showed that 96% reported having practiced defensive medicine by ordering imaging, laboratory tests, specialist referrals, or hospital admissions to avoid potential malpractice liability [80].
All of these studies and surveys have shown that assurance behaviors are more common than avoidance behaviors, with the most frequent practice being the excessive ordering of tests, especially imaging studies [17,76,77]. For example, in the survey of physicians in high-risk specialties, 92% of respondents reported ordering more tests, performing more diagnostic procedures, and referring more patients for consultation [77]. Approximately 42% of the respondents said they had recently limited their practice to eliminate procedures with a high risk of complications or had avoided patients with complex medical problems or who were perceived as litigious [77]. A 2015 study that included more than 24,000 physicians, evaluated data from acute care hospital admissions in Florida from 2000 to 2009 [81]. Across specialties, greater average spending by physicians was associated with reduced risk of incurring a malpractice claim. For example, among internists, the probability of an alleged malpractice incident ranged from 1.5% with spending at $19,725 to 0.3% with spending at $39,379. In six of the specialties evaluated, a greater use of resources was associated with a statistically significantly lower subsequent rate of alleged malpractice incidents [81].
Both types of defensive medicine have several important implications for health care and healthcare costs. Unneeded testing may be associated with false-positive results and treatment complications, and limitations in physician services can lead to unmet care needs [17,75]. The financial cost of defensive medicine is difficult to quantify, primarily because of the challenges in identifying and measuring assurance and avoidance behaviors. Physician expectations about the benefits and harms of interventions also may be a contributing factor. One systematic review sought to assess clinicians' expectations of the benefits and/or harms of any treatment, test, or screening test [82]. Following a comprehensive search of four well-known databases, the authors included a total of 48 articles in their review: 20 focused on treatment, 20 on medical imaging, and 8 on screening. Of these, the majority (67%) assessed only harm expectations. Among the studies that compared benefit expectations with a correct answer (total of 28 outcomes), most participants provided correct estimation for only 3 outcomes (11%). Among the studies that compared expectations of harm with a correct answer (total of 69 outcomes), most participants correctly estimated harm for only 9 outcomes (13%) [82]. Inaccurate perceptions about the benefits and/or harms of interventions contribute to suboptimal clinical management choices and increased costs. A 1994 study estimated the cost of defensive medicine to be between $5 and $15 billion in 1991 U.S. dollars [74]. A study published in 2010 found that annual overall medical liability costs are an estimated $55.6 billion, or 2.4% of total healthcare spending [82].
A malpractice claim has a profound impact on a physician in terms of time, psychologic effects, and reputation. The average length of time between the date of an incident and closure of the claim is approximately four to five years [1,2,4,72]. During this time, the physician is distracted with the malpractice defense and the legal process robs time from personal and professional activities.
Malpractice litigation has a negative psychologic effect on a physician because of its threat to personal integrity and honor. In general, physicians share personality traits that render them particularly vulnerable to malpractice litigation in which fault must be established [83]. These traits include self-criticism, exaggerated sense of responsibility, and vulnerability to guilt [84]. Physicians may experience loss of self-esteem and engage in self-questioning (e.g., "What did I do wrong?" or "What could I have done better?") [72,85]. In addition, the adversarial nature of litigation contradicts the normal work environment of a physician. As a result, approximately 80% to 95% of physicians have reported emotional distress during the process of malpractice litigation [86,87]. This distress affects not only the physician but also his or her family and office staff [72]. A physician's reaction to a malpractice claim has been described as beginning with a sense of shock, outrage, or dread, followed by feelings of intense anger, frustration, isolation, and inner tension [83]. In a study of physicians with a malpractice claim, 54% indicated that they were very surprised by the claim, 32% were somewhat surprised, and 14% were not surprised [4]. In cases in which there is clearly a negative outcome, the physician may also feel a substantial amount of guilt. Among the most common reactions to malpractice are [87,88]:
Adjustment disorder symptoms (20% to 50%)
Major depressive disorder symptoms (27% to 39%)
Onset or exacerbation of physical illness (2% to 15%)
A malpractice suit may also cause negative professional effects. In addition to the time spent away from the practice to defend a claim, a physician's and/or practice's reputation can be damaged by a claim, regardless of the outcome of the litigation [85]. In a 2021 survey of physicians who have had a malpractice lawsuit, 48% indicated changes to their practice. Among these changes were lack of trust in patients or treating them differently (24%); leaving the practice setting (7%); changing insurer (3%); and/or purchasing more insurance (2%) [4]. In addition, 29% of physicians surveyed felt that the lawsuit negatively affected their medical career [4]. A malpractice suit may also have implications on licensing and credentialing [72]. In general, patterns in the type of adverse events and the severity (amount) of payment to resolve the claim are the focal points for licensing boards and credentialing bodies [6]. Availability and cost of liability insurance may also be concerns; the frequency and severity of claims influence insurance underwriting, but a favorable settlement will weigh positively in the risk evaluation of the insurer [6].
The risk of negative physical and psychologic outcomes during and after a medical malpractice claim has been termed medical malpractice stress syndrome; it presents similarity to post-traumatic stress disorder. Strategies to ensure emotional and physical health due to the consequences of medical malpractice stress syndrome include increasing social support systems, replacing the mystery surrounding litigation with knowledge, and seeking the appropriate medical and psychiatric help [89].
When developing an office-based risk management program, a physician should address the underlying causes, diagnoses, and patient motivators that have been identified most often in malpractice claims, especially as they pertain to his or her medical specialty. Surveys of medical office practices have shown that, across all physician specialties, the most common problems related to risk management include [5]:
Ineffective process to track diagnostic test results/consults
Incomplete or poor documentation
Failure to review patients' medications and provide education on taking prescribed medications
The following elements are essential for an effective risk management program:
Optimum patient-physician communication
Mandate for informed consent
Appropriate and complete documentation
Establishment and maintenance of efficient office processes
Quality assurance program
System for evaluating practice behaviors
Continued development of diagnostic and technical skills
The lack of effective patient-physician communication has been noted to be perhaps the second leading cause of malpractice [18,72]. In one study, communication problems were noted by patients in 70% of malpractice depositions [90]. In addition, problems with patient-physician communication have been reported to contribute significantly to patient dissatisfaction, which is commonly a precursor to a malpractice claim [91]. The quality of the patient-physician relationship affects many areas within a risk management program, including diagnosis, patient satisfaction, disclosure of errors, informed consent, and medication management.
Effective communication also serves to build rapport, to strengthen mutual trust, and to demonstrate the physician's respect of the patient's preferences and culture, which can help avoid malpractice claims [92]. In contrast, ineffective patient-physician communication can lead to anger, misunderstandings, and unrealistic expectations, all of which have been associated with malpractice claims [32,93]. Improved patient-physician communication may mitigate the harm from medical errors in some cases and may also help reduce the frequency of future errors [49]. Thus, optimizing patient-physician communication and strengthening the patient-physician relationship is a priority in managing risk.
Optimum patient-physician communication involves ensuring that patients are adequately informed, which includes addressing the patient's literacy level and cultural context, ensuring that patients are satisfied with their care, and alerting patients about errors in a timely manner.
Physicians with a history of malpractice claims have been described by their patients as not providing enough information about their condition, prognosis, medication side effects, and alternative treatment options [94]. This information is necessary to enable individuals to be active participants in their healthcare decisions. Physicians should also educate patients about realistic outcomes, as surveys have demonstrated a gap between individuals' perceived outcomes and realistic outcomes [7]. As examples, patients have reported that the pain or complications related to a procedure or surgery were not expected, and women have overestimated by 100-fold the value of screening mammography in reducing breast cancer-related mortality [94,95].
To help ensure that individuals are adequately informed about their health and care, the Partnership for Clear Health Communication launched the Ask Me 3 campaign. This patient education initiative is designed to encourage patients to understand the answers to three basic questions [96]:
What is my main problem?
What do I need to do?
Why is it important for me to do this?
If a patient does not ask these questions, the physician should emphasize the importance of understanding the answers. Educational resources for patients are available at the Institute for Healthcare Improvement/National Patient Safety Foundation website, https://www.npsf.org.
Several other strategies have been recommended as ways to strengthen communication and enhance the patient-physician relationship (Table 3) [36,92,97].
ENHANCING THE PATIENT-PHYSICIAN RELATIONSHIP
|
Communicating effectively and establishing rapport are more challenging when the patient's literacy level is low or his or her primary language differs from that of the practitioner. Misunderstandings can lead patients to think that a poor health outcome or adverse event is the result of physician error rather than related to the lack of a clear understanding.
Health literacy, the ability to understand health information and make informed health decisions, is integral to good health outcomes [98]. Yet, the National Assessment of Adult Literacy estimated that only 12% of adults have "proficient" health literacy and 14% have "below basic" health literacy, which means they lack the ability to understand health information and make informed health decisions [98,99,100]. According to the Center for Health Care Strategies (CHCS), a Medicaid partner, nearly 9 out of 10 adults in the United States struggle with health literacy [101]. Rates of health literacy are especially low among ethnic minority populations and individuals older than 60 years of age [98]. Compounding the issue of health literacy is the high rate of individuals with limited English proficiency. According to U.S. Census Bureau data from 2023, more than 68 million Americans speak a language other than English at home, with approximately 26.2 million of them (8.4% of the population) speaking English less than "very well" [102].
Physicians should assess their patients' literacy level and understanding and implement interventions as appropriate. It has been suggested that when patients are first evaluated, they should be asked what language is spoken at home and if they speak English "very well" (if the healthcare professional is English-speaking) [103]. In addition, physicians should ask what language patients prefer for their medical care information, as some prefer their native language even though they have said they can understand and discuss symptoms in English [103].
Physicians should use plain language in their discussions with patients who have low literacy or limited English proficiency. They should ask them to repeat pertinent information in their own words to confirm understanding [104]. Reinforcement with the use of low-literacy or translated written educational materials is helpful.
"Ad hoc" interpreters, such as family members, friends, and bilingual staff members, are often used instead of professional interpreters for a variety of reasons, including convenience and cost. Physicians should check with their state's health officials about the use of ad hoc interpreters, as several states have laws about who can interpret medical information for a patient [105]. Even when allowed by law, the use of a patient's family member or friend as an interpreter should be avoided, as the patient may not be as forthcoming with information and the family member or friend may not remain objective [105]. Children should especially be avoided as interpreters, as their understanding of medical language is limited and they may filter information to protect their parents or other adult family members [105]. Individuals with limited English language skills have actually indicated a preference for professional interpreters rather than family members [106].
Most important, perhaps, is the fact that clinical consequences are more likely with ad hoc interpreters than with professional interpreters [107]. A systematic review of the literature showed that the use of professional interpreters facilitates a broader understanding and leads to better clinical care than the use of ad hoc interpreters, and many studies have demonstrated that the lack of an interpreter for patients with limited English proficiency compromises the quality of care and that the use of professional interpreters improves communication, utilization, clinical outcomes, and patient satisfaction with care [108,109]. The importance of professional interpreters to effective communication and patient safety has been recognized by the development of The National Board of Certification for Medical Interpreters, founded in 2010 by the International Medical Interpreters Association [110].
When professional interpreters are not feasible or available, bilingual staff members may be used, and their adherence to several principles can enhance their effectiveness [105]:
Use the universal form of the language when possible
Avoid assuming the role of interviewer or decision-maker
Allow the patient to lead the discussion
Translate everything (without additions, deletions, or changes to meaning)
Translate in a way to convey the patient's cultural context
Meet the patient before the interaction to be translated
Meet with the physician before the visit, to develop a structure to the interaction
Seek continuing education to improve interpretation skills
Physicians should encourage their bilingual staff members to enhance their interpretation skills. Resources for such training include the Cross Cultural Health Care Program and the National Council on Interpreting in Health Care.
When no professional or ad hoc interpreters are available, physicians may be able to obtain an interpreter from a community organization. In addition, several translation businesses offer fee-based interpretation over the phone or Internet. Many of these businesses also provide translation of documents. Partnering with healthcare plans and hospitals can help identify the best services for your practice [104].
If a patient refuses to use an interpreter, the physician should emphasize to the patient and family the importance of accurate interpretation and understanding on both sides of the patient-physician discussion. A referral to a physician who speaks the patient's primary language may be appropriate [104].
The AMA offers several health literacy resources for healthcare professionals on its website, and the U.S. Department of Health and Human Resources offers valuable information on cultural competency from the Health Resources and Services Administration (HRSA) and the Office of Minority Health. The HRSA also offers a free online course, "Unified Health Communication 101: Addressing Health Literacy, Cultural Competency, and Limited English Proficiency." Another resource is Diversity Rx, a joint initiative of the Resources for Cross Cultural Health Care and the Center for Health Equality at Drexel University School of Public Health.
Issues related to literacy and interpretation should be noted in the patient's record to provide documentation of the physician's assessment of understanding.
Patients who have experienced harm from a medical error are less likely to file a malpractice claim if they consider their physician to be caring or compassionate; in contrast, patients who are dissatisfied with their physician are more apt to file a claim [32,111]. Thus, making efforts to ensure that patients are satisfied with their care is another integral aspect of a risk management program.
Patients are satisfied when they feel as if they receive sufficient attention from healthcare professionals. Patients of physicians with prior malpractice claims have reported feeling rushed and ignored, being given explanations and advice that were inadequate, and having shorter office visit times than patients of physicians with no malpractice history [112]. A study of primary care physicians and their patients showed that physicians with no history of malpractice differed significantly from those with previous claims in terms of the use of facilitation statements, the amount of information given to orient the patient to the office visit, and the use of humor [111]. In addition, the length of a routine office visit was a significant predictor of a malpractice claim [111].
Patient satisfaction can be enhanced by improving service throughout the office. Physicians should assess every aspect of the office, including the waiting room, front desk staff and procedures, billing and scheduling, and staff interactions, to ensure that patients receive a positive experience throughout the office [72]. After these aspects have been assessed, ways to improve service should be discussed with all staff members and service should be assessed in an ongoing manner [72].
Assigning a staff member to receive and review complaints and address them in a timely manner can help mitigate patient dissatisfaction [72]. In addition to helping to address a patient's concern, handling a complaint also provides evidence of efforts to address the situation should a claim be presented [72]. Documenting complaints and their resolution can also serve as an important aspect of a quality assurance program [72].
Numerous studies have shown that patients prefer full disclosure of a medical error and want details about how the error occurred, what the consequences are (including financial costs), and what measures are being taken to prevent the same error from occurring again [73,113,114,115,116,117,118]. Disclosure of errors has been linked to many benefits, including increased patient satisfaction, greater trust with the physician, and higher likelihood of a patient's positive experience, all of which are related to a lower likelihood that a patient will sue [49]. Physicians have indicated that they want to apologize for errors, but in practice, a substantial number of physicians have admitted that they did not disclose an error [114,119,120]. In addition, in a national survey of individuals who had experienced a medical error, only 32% said that the involved healthcare professional had disclosed the error [27].
Physicians and ethicists have long acknowledged that physicians have an ethical and moral obligation to disclose errors [73,121]. However, for many years, defense lawyers have advised physicians to avoid apologizing to a patient for an adverse event for fear that the apology would be used as an admission of wrongdoing [113,117,119,122]. This approach is changing. Several professional associations and patient safety organizations have established statements endorsing disclosure (Table 4) [26,123,124,125,126]. Legislation has also addressed disclosure, with some states requiring that hospitals notify a patient (or patient's family) about a "serious event" in writing within a specific amount of time after the event [118]. The Sorry Works! Coalition was established in 2005 and has become the leading advocacy group for disclosure, apology (when appropriate), and compensation (if necessary) after adverse medical events [127]. Sorry Works! notes four basic facts every physician should know about disclosure [127]:
Disclosure benefits doctors as well as nurses, hospitals, and insurers.
Successful disclosure depends on overall good communication, informed consent, and excellent customer service.
An empathetic apology should be provided immediately after an adverse event.
After apologizing, the healthcare professional should immediately call a risk manager, insurance company, or defense counsel.
STATEMENTS ENDORSING DISCLOSURE
| Organization | Statement | ||
|---|---|---|---|
| American Medical Association |
Code of Medical Ethics (8.6 Promoting Patient Safety) Patients have a right to know their past and present medical status, including conditions that may have resulted from medical error. Open communication is fundamental to the trust that underlies the patient-physician relationship, and physicians have an obligation to deal honestly with patients at all times, in addition to their obligation to promote patient welfare and safety. Concern regarding legal liability should not affect the physician's honesty with the patient. Individual physicians who have been involved in a (possible) medical error should:
| ||
| National Quality Forum |
|
As discussed, apology statutes now protect physicians and other healthcare professionals who apologize, but not all states have enacted apology statutes, and the statutes vary across states. In addition, the majority of physicians are unfamiliar with their state statutes. Physicians are encouraged to talk to their state medical associations and legal counsel to determine how best to comply with their state's apology statute.
Most physicians are uncomfortable with disclosing errors and, because they have not received formal training in how to conduct such a discussion, they are unclear about how much information to provide and what words and phrases to use [122,128]. As a result, physicians who disclose errors often provide minimal information and express incomplete apologies [115,117]. Guidelines have been developed to help physicians disclose errors in a way that provides patients (and family) with the information they desire [126,129,130]. These guidelines recommend:
Disclose the error as soon as possible; do not wait for the patient (or family) to ask.
Be prepared for strong emotions.
Tell what you know; focus on what happened and the possible consequences.
Accept responsibility for the outcome, but avoid attributions of blame.
Express apology and regret.
Outline a plan of care to address the harm and to prevent recurrence.
Offer to get second opinions, when appropriate.
Suggest a family meeting (with the option of having lawyers present).
Document the disclosure discussion.
Offer to have follow-up meetings if the patient desires.
The impact of full disclosure on malpractice liability is unclear [117,122]. Early reports of full-disclosure policies at two institutions (the University of Michigan and the Lexington Veterans Affairs Medical Center, Kentucky) indicated that such policies can reduce the number of malpractice claims, increase the number of settled claims, and decrease legal expenses [91,131]. Studies in which individuals are presented with clinical scenarios or vignettes involving adverse events have also suggested that patients would be less likely to sue if physicians provided disclosure and an apology [73,115,116,121,132]. However, there is no conclusive evidence demonstrating that disclosing errors decreases the likelihood of litigation [113,122]. Some have argued that uniform disclosure of errors may actually lead to an increase in malpractice claims [91].
Informed consent requires patients to sign a document stating that they understand the risks and benefits of a procedure or treatment plan and alternative treatment options. However, the principle of informed consent extends beyond the signed form. The process of informed consent helps patients assume an active role in healthcare decision making and aids in the management of patients' expectations, both of which can reduce the likelihood of a malpractice claim [133].
Essential elements of the informed consent conversation include the diagnosis, the proposed procedure or treatment plan and its potential risks and expected benefits, the risks and benefits of any alternative treatment options, the typical recovery process, and the expected long-term and short-term effects (Table 5) [40,133]. In addition, physicians should tailor the informed consent discussion to a patient's unique situation, noting risks that may be applicable to a patient because of his or her medical history or current comorbidities [41].
DISCUSSION POINTS FOR INFORMED CONSENT
|
In a study to assess the levels of knowledge of patients, more than 80% of patients were satisfied with an informed consent discussion about pending surgery and considered themselves to be fully informed, but more than half could not list a single potential complication related to the surgery [134]. A patient's dissatisfaction with an informed consent discussion is most likely to surface only if an adverse event occurs after the treatment was given. Because of the gap between what is told and what is remembered, a patient may think that an adverse event is the result of inadequate informed consent or negligent care [135].
Given the challenge of knowing whether a patient has understood the informed consent discussion, physicians should take several efforts to enhance understanding. Asking the patient to read a section of the informed consent form aloud enables the physician to assess the patient's literacy level [41]. Physicians should plan sufficient time to speak with the patient and should present information in easy-to-understand language. Patients should be encouraged to ask questions and to take an active role in decision making [135]. Lastly, the patient should be asked to describe a section or sections of the form in his or her own words to demonstrate the level of understanding. Physicians should have consent forms translated into languages spoken by any large percentage of their patient population [41].
Informational resources in a variety of media may be helpful as a supplement to the discussion. These resources help emphasize realistic expectations and address different learning preferences; as such, they have been shown to enhance understanding, especially for patients with low educational levels [72,136,137]. A systematic review of 55 trials on decision aids indicated that they increase patients' involvement and are more likely to lead to informed values-based decisions, but the size of this effect has varied across studies [138]. An updated review that included 105 trials indicated that decision aids are more likely to lead to improved patient knowledge and improved perception of the risks involved [139].
If time allows, it is reasonable to let patients consider a decision made after signing an informed consent form [36]. Giving a patient 24 to 48 hours to think about the risks and benefits can reinforce the validity of the informed consent [36]. If a patient withdraws consent, it should be documented in the medical record, with the date and time of withdrawal.
Documenting the informed consent discussion in the patient's record and including the signed informed consent form in the record decreases the probability of a successful malpractice case against the physician [36]. A signed informed consent form is not automatic protection; patients can argue that the risks were discussed by a healthcare professional other than the physician who performed the treatment or that they did not understand the risks.
The patient's medical record is a legal document that reflects the care provided to a patient, and it serves as the basis of defense against malpractice claims and other types of lawsuits [9]. As such, it is crucial for physicians to document all encounters and patient information carefully and accurately [9]. Experts indicate that no amount of documentation is too much, especially in situations at high risk for malpractice claims because of the patient's diagnosis or the physician's specialty [85]. Careful, complete documentation provides proof that the physician did the right thing and demonstrates that the physician gave logical thought and consideration to the case [85,97].
Despite the importance of complete medical records, surveys of office practices have shown that documentation is frequently incomplete or poor, with the most often lacking elements being [140]:
Updated problem list
Discussion of medications
Allergies
Informed consent process
Physician signature (to indicate review)
Physicians should ensure that all essential information is documented in every patient's record (Table 6) [9,85,141,142]. In addition, the record should include written instructions that were provided to the patient. Documentation should be clear, objective, specific, and dated. The use of abbreviations should be limited to those that are approved.
ESSENTIAL INFORMATION TO DOCUMENT
|
Problems exist with both paper and electronic medical records. Paper records are often found to be illegible, and electronic medical records are frequently used inconsistently by the physicians within a practice [140]. Practices with electronic medical records should have a reliable backup system as well as a disaster recovery program [9]. A physician should never alter a medical record after a claim has been filed [9,85].
Most medical errors have been found to be related to faulty systems rather than incompetence, which means that improving office and practice routines can help physicians avoid adverse outcomes [61]. Efficient office processes and procedures enhance the quality of patient care while decreasing the risk for medical error.
Electronic health records are increasingly being used in hospitals and office-based practices. Since 2009, the percentage of clinicians and hospitals using electronic health records has almost doubled, from 46% in 2009 to 88% in 2019 [143]. Preliminary data suggest that physicians who use electronic health records are less likely to have paid malpractice claims [144]. However, the effect of electronic health records on the quality of care and the potential for mitigating malpractice is unclear. One study of electronic health record-related malpractice claims found that 48% of claims were caused either by system factors such as failure of drug or clinical decision support alerts, or by user factors, such as copying and pasting progress notes [145]. In addition, a 2018 survey of physician attitudes toward electronic health records showed that 69% felt that the clerical aspect of updating records takes valuable time away from their patients, and 49% felt that using an electronic health records detracts from their clinical effectiveness [146]. Regardless of whether an office is paper-based or technology-based, the most important systems that should be established are standardized procedures and tools for improving diagnosis, ordering and tracking tests, and managing patient's medications.
Each task in a physician practice should be standardized to ensure that the task is carried out accurately and efficiently each time, regardless of who is performing the task [146,147,148]. The use of standardized procedures helps to avoid errors related to lapses in staff members' memory or to the use of new staff. Following a standardized approach to each patient ensures consistent, high-quality care for all patients. This approach is also helpful in the event the physician does not provide comprehensive documentation for a visit. For example, if a physician forgets to document a breast examination during a female patient's annual physical examination but uses a standardized approach that includes this examination for all women during an annual physical examination, the physician can confidently describe the care given despite the lack of documentation [97].
Establishment of standardized procedures should begin with evidence-based protocols or standing order sets for chronic diseases and vital sign checks for all patients, regardless of the nature of the visit. Flowcharts, checklists, templates, and/or automatic alerts or reminders can help ensure that standardized procedures are carried out [147,148].
Given that missed or delayed diagnosis is the leading basis of malpractice suits, enhancing diagnostic accuracy is imperative. As stated earlier, diagnostic errors are usually the result of several breakdowns in the diagnostic process [57]. Physicians should develop risk management strategies that focus on the most common breakdowns in the diagnostic process. Thus, physicians should ensure that they:
Obtain a thorough history
Perform a comprehensive physical examination
Order and track diagnostic tests appropriate for a patient's signs and symptoms
Create a proper follow-up plan
Seek additional interpretation of diagnostic tests if results are uncertain or inconclusive or seem incongruous with the patient's condition
Reviews of malpractice claims, as well as a systematic review of the literature, have shown that diagnostic errors are most often involved with atypical or nonspecific presentations, rarity of the disease, or masking comorbidities [60,85]. For example, claims related to myocardial infarction are often associated with no history of cardiac problems, a normal electrocardiogram, and atypical signs and symptoms [85]. Similarly, malpractice claims related to breast cancer often involve younger women (average age: 45 years). Physicians should take care not to exclude diagnoses because of nontraditional presentations or low prevalence of a condition.
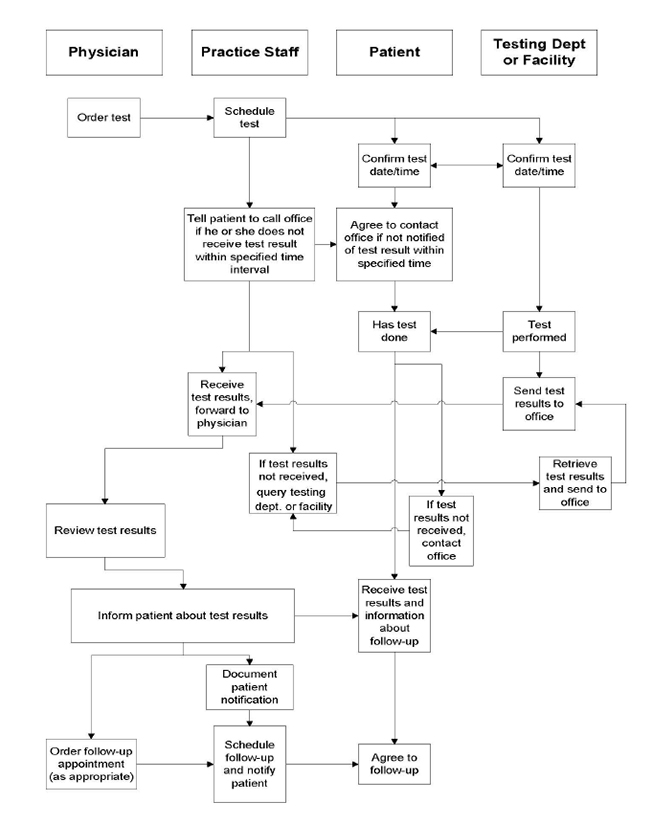
An inappropriate or inadequate follow-up plan has been alleged in nearly one-half of claims of misdiagnosis [57,62]. Failure to follow-up has often involved a lack of follow-up after abnormal testing, an uncertain diagnosis, or referrals [57,97]. In addition to providing guideline-based follow-up, physicians should seek ways to improve scheduling procedures, to check patient compliance with testing and referrals, and to track test results.
Most physicians are not aware that they need help in making accurate diagnoses, which means that automatic strategies, such as clinical decision support integrated into electronic health records, may be most helpful [57,149]. Other effective interventions include electronic prompts in response to input of certain data and automated systems for tracking test results and scheduling follow-up [57].
Documentation of the differential diagnosis in the patient's record will reflect the physician's thought process in determining a diagnosis, which can be helpful if a malpractice claim is made [85]. This is especially important for diagnoses at high risk for malpractice, such as cancer (especially breast cancer) and myocardial infarction. The patient's report of symptoms should be carefully documented, as well as all tests ordered, the patient's compliance with screening and testing, and scheduled follow-up visits.
Laboratory and/or imaging studies are often an integral aspect of determining a definitive diagnosis, and inadequacies in managing test results can be an important factor in enhancing the timeliness and accuracy of diagnoses. Inadequate test tracking is an important factor in medical errors, with studies of primary care patients indicating that 15% to 54% of medical errors are related to test processes [150].
Ordering and tracking test results is a complex process, and the volume and variety of tests ordered within a practice add to the challenge. Four principle steps are involved in managing patients' test results [148,151]:
Tracking tests until the results have been received
Notifying patients of test results
Documenting that patients were notified
Ensuring that patients with abnormal results receive the recommended follow-up care
A literature review indicated that there is no clearly defined method for tracking results that is effective and efficient at each of these steps, but a task flow can be created from some "good processes" that have been defined (Figure 3) [152,153]. Studies have shown that most physician practices do not have an established protocol for managing test results, and the processes used to track test results vary widely, even within a single multiphysician practice [150,152,153]. In fact, the most common finding in a survey of office practices (across a broad range of specialties) was the lack of an effective tracking system for test results [140]. In one study, 92% of physicians said that each physician in their group practice used a different method for reporting lab results, with 61% using different processes for different types of tests [152].
The lack of a clearly defined system for tracking or managing test results has led to high rates of failure to inform patients of test results and delays in notifying patients. The most common problems are a lack of a consistent system to verify that the physician has reviewed the results and communicated them to the patient and the practice of notifying patients only when the results are abnormal [140]. According to one study, 7% to 26% of patients with test results were not informed of the results (or did not have documentation of notification) [153]. In another study, patient notification was documented in 58% to 85% of charts, but rates were lower for documentation of the physician's response to the result (47% to 84%) and for follow-up after abnormal results (28% to 55%) [140,146,150]. A 2022 qualitative study that included 28 patients and 19 general practitioners (GPs) from six practices found that test result communication varied between the GPs and patients were based on habit, unwritten heuristics, and personal preferences rather than protocols [154]. Further, the GPs who participated in the study expected their patients to know how to access their own test results. Both the patients and physicians assumed that the other party would make contact about the results, with potential implications for patient frustration, anxiety, and safety [154]. An analysis of negligence claims involving test results management found that 14 of the 50 cases analyzed (28%) involved a delay in diagnosis or treatment of a patient with cancer; 15 (30%) were judged to be "never events;" 24 cases (48%) involved failure to notify patients of an abnormal test result; and 18 cases (36%) involved a test result not being actioned by a doctor [155]. Frequently occurring contributory factors (60%) were related to local working conditions (e.g., responsibilities, lack of patient care continuity). As noted, prompting through electronic health record systems may help alleviate this issue [146].
Physicians recognize the inadequacy of test results tracking. When surveyed, most physicians have expressed dissatisfaction with their practice's process for tracking test results. These surveys have indicated that only 15% to 41% of physicians said they were satisfied with how test results were managed in their offices [146,156,157]. Physicians were most likely to be satisfied when they actively tracked test orders to completion and/or used tools to help set priorities for workflow and generate letters to patients [157].
The optimum process for managing test results will vary according to a practice's specific needs and resources, especially technology. A focus on patient safety and a willingness to embrace technology throughout a practice are important factors in establishing and maintaining an effective test tracking system [150]. In the past, several practices have established systems in which staff log ordered tests in a notebook or date-defined card boxes, check them off when test results come in and again when the physician signs off on the results, and note when the patient has been notified [85,148]. Although this system is effective, automated systems that perform the same tasks are more reliable and are less labor-intensive, a factor especially important in large practices [148]. Electronic clinical reminders are more efficient, and systems can be programmed to provide alerts when a test result is due or a patient should return for follow-up care [156]. Creating templates of patient notification letters for the most common tests is also helpful [148]. Also available are telephone and web-based programs that allow patients to obtain their test results; privacy is ensured with the need for a password, and some programs enable the physician to include specific comments to the patient [148].
Given the high risk of malpractice claims in association with various types of cancer, physicians should also be thorough in their approach to recommending screening tests. Follow-up should be done to ensure that the patient has had the screening and has been notified of the results. If the patient refuses to have screening despite the physician's recommendation and explanation of the risks, the refusal should be clearly documented in the patient's medical record [85].
Because appropriate follow-up after abnormal test results is often lacking, a test tracking system must involve a consistent process for scheduling follow-up visits. Failure to follow-up on abnormal mammography and ultrasound are common assertions in malpractice claims [85]. In addition, studies have shown that at least 20% to 36% of women do not receive guideline-directed follow-up after abnormal findings on mammography or Pap tests [158,159,160]. Failure to follow-up on suspicious findings on lung radiographs or computed tomography scans has also been noted [67].
Management of patients' medications is a frequent problem in medical office practice and a common basis for malpractice claims [64,65,140]. As noted earlier, a substantial proportion of medication errors and adverse drug events are considered to be preventable [64,65].
In the office and outpatient setting, preventable medication errors occur primarily in the prescribing and monitoring stages [65,161,162]. Prescribing errors were identified in up to 11% of prescriptions written in the primary care setting and were typically related to dosage errors [58,163]. Prescribing errors have also frequently involved the use of inappropriate drugs [65,162]. Inadequate monitoring has caused a wide variety of adverse effects, such as electrolyte/renal imbalance, bleeding, gastrointestinal toxicity, and neuropsychiatric events, and often requires hospitalization of the patient [65,161]. Other common medication-related errors are a failure to prescribe prophylactic agents when appropriate (as for patients taking nonsteroidal anti-inflammatory agents or anticoagulants) and drug-drug interactions [58,161].
Studies and reviews of malpractice claims have identified several drug classes that are most often associated with preventable medication errors: antibiotics, antidepressants or antipsychotic agents, cardiovascular drugs, anticoagulants, analgesics, hypoglycemic agents, and diuretics [64,65,161]. As with most medical errors, preventable medication errors are most frequently caused by system deficiencies [64]. Electronic prescribing systems have not been found to reduce the number of prescribing errors; for example, handwriting legibility issues have now been replaced by e-prescribing issues, such as selecting the wrong box in a dropdown menu [162,163]. General medication errors are still common. A 2014 observational study found that the most frequent prescribing errors were wrong drug quantity (40%), wrong duration of therapy (21%), wrong dosing directions (19%), and wrong dosage formulation (11%) [163]. Several strategies can help physicians avoid medication errors (Table 7) [9,164].
STRATEGIES FOR AVOIDING MEDICATION ERRORS
When administering a medication:
|
Risk management should also involve a quality assurance program in which the efficiency and outcomes related to policies and procedures are evaluated on an ongoing basis. All staff should be encouraged to provide feedback on ways to improve care; patient complaints can also provide opportunities for improvements [9]. In addition, physicians should evaluate their practice behaviors to identify evidence of defensive medicine to help eliminate variations in care and promote better patient outcomes.
It is also important to create an environment in which patient safety is emphasized. Physicians should provide leadership within the practice, encouraging teamwork, offering feedback on performance, and providing access to necessary training and continuing education for all staff [9].
Other issues that should be addressed in a risk management program are the scope of practice, termination of the patient-physician relationship, and retention of medical records.
All staff should perform only those tasks that are within the scope of their job descriptions, licensure, or certification [9]. In addition, staff should operate or maintain medical equipment or devices only if they have received appropriate training and have been certified (if required).
Physicians should have a standardized procedure for dismissing patients (i.e., terminating the patient-physician relationship when the patient presents insurmountable problems, such as unresolved issues with missed appointments, abusive treatment of staff, or threatening behavior) [165]. It is recommended that a physician dismiss a patient who has filed a malpractice suit [71,165].
When terminating a patient-physician relationship, the physician should send a letter to the patient, notifying him or her that the relationship will be terminated by a specific date, typically 30 days from the date of the letter [165]. The letter should be sent by certified mail with a return receipt requested to ensure appropriate delivery. A copy of the letter and the return receipt should be kept in the patient's medical record. Physicians should not refill a patient's prescription beyond the date of termination [9,165]. Physicians are not obligated to help patients find another physician, but assisting with the transfer of medical records demonstrates an interest in facilitating continuity of care, which may be helpful in the event of litigation [165]. The AMA Code of Ethics includes guidance on terminating the patient-physician relationship [166].
Most state and federal laws regarding mandatory retention times for medical records apply to hospitals rather than office-based practices. In the absence of state or federal laws, state medical boards and medical associations have recommended retention times [167]. It is recommended to retain medical records indefinitely, but if not, they should be kept for at least 10 years, and some associations recommend 25 years [167]. Medical records should be destroyed appropriately, and an inventory of all destroyed records should be kept.
Although overall paid medical malpractice claims have decreased since the early 2000s, the number of claims against primary care physicians increased during that time. The association of malpractice and medical errors is complex. Large studies have shown that malpractice claims often do not involve a negligent injury and that most patients who do sustain an injury due to negligence do not file a claim. These findings indicate that factors other than true medical error are motivators for a malpractice claim. A wide variety of motivators have been identified, the most common being inadequate patient-physician communication. Thus, physicians should protect their liability not only through patient safety efforts but also through enhancement of patient-physician communication and the patient-physician relationship.
The threat of malpractice—whether real or perceived—has a negative effect on physicians personally and professionally and ultimately adversely affects healthcare delivery, primarily through the use of defensive medicine. An effective risk management program helps physicians ensure patient safety and avoid the time and stress associated with litigation. The most effective risk management strategies are those that address specific issues identified in studies of closed malpractice claims and surveys of office practices.
Studies of malpractice claims have shown that diagnostic error (missed or delayed diagnosis) is the leading underlying cause of claims and is most often related to cancer (especially breast cancer) and myocardial infarction. Diagnostic errors are usually the result of several contributing factors rather than faulty judgment alone, and the most common breakdowns in the diagnostic process have been failure to order an appropriate diagnostic test or to create a proper follow-up plan. Surveys of medical office practices have shown that the most common risk management-related problem is an ineffective process for tracking diagnostic test results. As such, an effective system for ordering and tracking tests, including follow-up plans for abnormal results, is an essential component of a risk management program. Other essential components include a mandate for informed consent, appropriate and complete documentation, establishment and maintenance of efficient office processes, a quality assurance program, a system for evaluating practice behaviors, and continued development of diagnostic and technical skills of the physician and other healthcare professionals in the practice.
As noted, perhaps the most important element of a risk management program is optimum patient-physician communication. The quality of patient-physician communication and the patient-physician relationship affects many areas within a risk management program, including diagnosis, patient satisfaction, disclosure of errors, informed consent, and medication management. Effective communication also serves to build rapport, foster trust, avoid misunderstandings, and ensure realistic patient expectations, all of which have been shown to be associated with a lower risk of malpractice claims. Improved patient-physician communication may mitigate the harm from medical errors as well as help reduce the frequency of future errors.
| American Medical Association Code of Medical Ethics |
| https://www.ama-assn.org/topics/ama-code-medical-ethics |
| American Medical Association State Medical Liability Reform |
| https://www.ama-assn.org/practice-management/sustainability/state-medical-liability-reform |
| Institute for Healthcare Improvement: Patient Safety |
| https://www.ihi.org/improvement-areas/improvement-area-patient-safety |
| National Council on Interpreting in Health Care |
| https://www.ncihc.org |
1. Cohen D, Chan SB, Dorfman M. Malpractice claims on emergency physicians: time and money. J Emerg Med. 2012;42(1):22-27.
2. Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med. 2006;354(19):2024-2033.
3. Phillips RJ, Bartholomew LA, Dovey SM, Fryer GE Jr, Miyoshi TJ, Green LA. Learning from malpractice claims about negligent, adverse events in primary care in the United States. Qual Saf Health Care. 2004;13(2):121-126.
4. Gallegos A. Medscape Malpractice Report, 2021. Available at https://www.medscape.com/slideshow/2021-malpractice-report-6014604. Last accessed February 18, 2025.
5. Schaffer AC, Jena AB, Seabury SA, et al. Rates and characteristics of paid malpractice claims among us physicians by specialty, 1992–2014. JAMA Intern Med. 2017;177(5):710-718.
7. Fowler PR. Risk Management and Medical Liability: A Manual for Indian Health Service and Tribal Health Care Professionals. 3rd ed. Rockville, MD: Indian Health Service; 2018.
8. Loughlin KR. Medical malpractice: the good, the bad, and the ugly. Urol Clin North Am. 2009;36(1):101-110.
9. Top Ten Risk Management Issues for Medical Office Practices. Available at https://lhatrustfunds.com/assets/uploads/documents/Top-10-Risks-in-Office-Practice.pdf. Last accessed February 18, 2025.
10. American Society for Healthcare Risk Management. Enterprise Risk Management: A Framework for Success. Available at https://www.ashrm.org/sites/default/files/ashrm/ERM-White-Paper-8-29-14-FINAL.pdf. Last accessed February 18, 2025.
11. Institute of Medicine Committee on Quality of Health Care in America. To Err is Human: Building a Safer Health System. Washington, DC: The National Academies Press; 2000.
12. U.S. Department of Health and Human Services. National Practitioner Data Bank. Available at https://www.npdb.hrsa.gov/analysistool/. Last accessed February 18, 2025.
13. Guardado JR. Policy Research Perspectives: Medical Liability Claim Frequency Among U.S. Physicians. Chicago, IL: American Medical Association; 2017.
14. Bilimoria KY, Chung JW, Minami CA, et al. Relationship between state malpractice environment and quality of health care in the United States. Jt Comm J Qual Patient Saf. 2017;43:241-250.
15. Dick JF 3rd, Gallagher TH, Brenner RJ, et al. Predictors of radiologists' perceived risk of malpractice lawsuits in breast imaging. AJR. 2009;192(2):327-333.
16. Carrier ER, Reschovsky JD, Katz DA, Mello MM. High physician concern about malpractice risk predicts more aggressive diagnostic testing in office-based practice. Health Affairs. 2013;32(8):1383-1391.
17. Carrier ER, Reschovsky JD, Mello MM, Mayrell RC, Katz D. Physicians' fears of malpractice lawsuits are not assuaged by tort reforms. Health Affairs. 2010;29(9):1585-1592.
18. Pritchard DJ. A plaintiff attorney's candid view of medical malpractice. Clin Perinatol. 2005;32(1):191-202.
19. Blackston JW, Bouldin MJ, Brown CA, Duddleston DN, Hicks GS, Holman HE. Malpractice risk prevention for primary care physicians. Am J Med Sci. 2002;324(4):212-219.
21. Jena AB, Seabury S, Lakdawalla D, Chandra A. Malpractice risk according to physician specialty. N Engl J Med. 2011;365:629-636.
22. Public Citizen's Congress Watch. Medical Malpractice Payments Sunk to Record Low in 2011. Available at https://www.citizen.org/?s=medical+malpractice+payments. Last accessed February 18, 2025.
23. Diederich Healthcare. 2022 Medical Malpractice Payout Analysis. Available at https://www.diederichhealthcare.com/the-standard/2022-medical-malpractice-payout-analysis/. Last accessed February 18, 2025.
24. American Medical Association. Medical Liability Reform NOW! The Facts You Need to Know to Address the Broken Medical Liability System, 2024 Edition. Available at https://www.ama-assn.org/system/files/mlr-now.pdf. Last accessed February 18, 2025.
25. Kessler DP. Evaluating the medical malpractice system and options for reform. J Econ Perspect. 2011;25(2):93-110.
26. American Medical Association. Code of Medical Ethics. Opinion 8.6: Promoting Patient Safety. Available at https://code-medical-ethics.ama-assn.org/ethics-opinions/promoting-patient-safety#. Last accessed February 18, 2025.
27. NORC at the University of Chicago, IHI/NPSF Lucian Leape Institute. Americans' Experiences with Medical Errors and Views on Patient Safety. Cambridge, MA: Institute for Healthcare Improvement and NORC at the University of Chicago; 2017.
28. Localio AR, Lawthers AG, Brennan TA, et al. Relation between malpractice claims and adverse events due to negligence: results of the Harvard Medical Practice Study III. N Engl J Med. 1991;325(4):245-251.
29. Makary MA, Daniel M. Medical error—the third leading cause of death in the U.S. BMJ. 2016;353:i2139.
30. Baldor DJ, Kravietz A. Rapid Response Re: Medical Error—The Third Leading Cause of Death in the U.S. Available at https://www.bmj.com/content/353/bmj.i2139/rapid-responses. Last accessed February 18, 2025.
31. Studdert DM, Thomas EJ, Burstin HR, Zbar BI, Orav EJ, Brennan TA. Negligent care and malpractice claiming behavior in Utah and Colorado. Med Care. 2000;38(3):250-260.
32. Virshup BB, Oppenberg AA, Coleman MM. Strategic risk management: reducing malpractice claims through more effective patient-doctor communication. Am J Med Qual. 1999;14(4):153-159.
33. Taber's Online Medical Dictionary. Available at https://www.tabers.com/tabersonline. Last accessed February 18, 2025.
34. Cornell University Law School Legal Information Institute. Negligence. Available at https://www.law.cornell.edu/wex/negligence. Last accessed February 18, 2025.
35. Stimson C.J. Hospital risk management and the U.S. legal system: an introduction to U.S. medical malpractice tort law. In: Merkle W (ed). Risk Management in Medicine. Berlin: Springer; 2016.
36. Paterick TJ, Carson GV, Allen MC, Paterick TE. Medical informed consent: general considerations for physicians. Mayo Clin Proc. 2008;83(3):313-319.
37. Sage WM, Kersh R (eds). Medical Malpractice and the U.S. Health Care System. Cambridge: Cambridge University Press; 2006.
39. Bal BS. An introduction to medical malpractice in the United States. Clin Orthop Relat Res. 2008;467(2):339-347.
40. American Medical Association. Informed Consent. Available at https://code-medical-ethics.ama-assn.org/ethics-opinions/informed-consent. Last accessed February 18, 2025.
41. Dixon LA. Informed consent: new requirements from Centers for Medicare and Medicaid Services. Doctor's Advocate. 2007;2.
42. American Hospital Association. CMS Updates Informed Consent Guidance for Hospitals. https://www.aha.org/news/headline/2024-04-01-cms-updates-informed-consent-guidance-hospitals. Last accessed February 18, 2025.
43. Department of Health and Human Services. Centers for Medicare and Medicaid Services. Center for Clinical Standards and Quality/Quality, Safety and Oversight Group. Revisions and Clarifications to Hospital Interpretive Guidelines for Informed Consent. Available at https://www.cms.gov/files/document/qso-24-10-hospitals.pdf. Last accessed February 18, 2025.
44. LawInfo. What are Good Samaritan Laws? Available at https://resources.lawinfo.com/personal-injury/what-are-good-samaritan-laws.html. Last accessed February 18, 2025.
45. U.S. Department of Homeland Security. Law Enforcement Officer "Good Samaritan Act". Available at https://www.fletc.gov/sites/default/files/imported_files/training/programs/legal-division/downloads-articles-and-faqs/downloads/other/gtoodsamar.pdf. Last accessed February 18, 2025.
46. Hattis P, Staton S. Charitable Immunity Manual: A Review of U.S. Charitable Immunity Legislation for Volunteer Health Care Providers. Providence, RI: Volunteers in Health Care; 2002.
47. Shapiro HB. Providing charity care: a primer on liability risk. Fam Pract Manage. 2003;10(1):52-54.
48. ProBono. State Liability Laws for Charitable Organizations and Volunteers. Available at https://probonopartner.org/?s=State+Liability+Laws+for+Charitable+Organizations+and+Volunteers. Last accessed February 18, 2025.
49. McDonnell WM, Guenther E. Narrative review: do state laws make it easier to say "I'm sorry?" Ann Intern Med. 2008;149(11):811-816.
50. Ho B, Liu E. Does Sorry Work? The Impact of Apology Laws on Medical Malpractice. Available at http://irving.vassar.edu/faculty/bh/Ho-Liu-Apologies-and-Malpractice-nov15.pdf. Last accessed February 18, 2025.
51. Beaulieu-Volk D. Apology Laws: Talking to Patients about Adverse Events. Available at https://www.medicaleconomics.com/view/apology-laws-talking-patients-about-adverse-events. Last accessed February 18, 2025.
52. National Conference of State Legislatures. Medical Professional Apologies Statutes. Available at https://www.ncsl.org/financial-services/medical-professional-apologies-statutes. Last accessed February 18, 2025.
53. Medical Professional Liability Association. Available at https://www.mplassociation.org. Last accessed February 18, 2025.
54. Thomson Reuters Expert Witness Services. Jury Verdicts and Statements. Available at https://legal.thomsonreuters.com/en/products/westlaw/jury-verdicts. Last accessed February 18, 2025.
55. Wallace E, Lowry J, Smith SM, Fahey T. The epidemiology of malpractice claims in primary care: a systematic review. BMJ Open. 2013;3(7).
56. Gupta A, Snyder A, Kachalia A, et al. Malpractice claims related to diagnostic errors in the hospital. BMJ Qual Saf. 2018;27:53-60.
57. Gandhi TK, Kachalia A, Thomas EJ, et al. Missed and delayed diagnoses in the ambulatory setting: a study of closed malpractice claims. Ann Intern Med. 2006;145(7):488-496.
58. Sandars J, Esmail A. The frequency and nature of medical error in primary care: understanding the diversity across studies. Fam Practice. 2003;20(3):231-236.
59. Kachalla A, Gandhi TK, Puopolo AL, et al. Missed and delayed diagnoses in the emergency department: a study of closed malpractice claims from 4 liability insurers. Ann Emerg Med. 2007;49(2):196-205.
60. Kostopoulou O, Delaney BC, Munro CW. Diagnostic difficulty and error in primary care—a systematic review. Fam Pract. 2008;25(6):400-413.
61. Troxel DB. Do health system errors cause medical malpractice claims? Bull Am Coll Surg. 2009;94(5):30-31.
62. Committee on Diagnostic Error in Health Care, Board on Health Care Services, Institute of Medicine, The National Academies of Sciences, Engineering, and Medicine, Balogh EP, Miller BT, Ball JR (eds). Improving Diagnosis in Health Care. Washington, DC: National Academies Press; 2015.
63. Singh H, Giardina TD, Meyer AN, et al. Types and origins of diagnostic errors in primary care settings. JAMA Intern Med. 2013;173(6):418-425.
64. Rothschild JM, Federico FA, Gandhi TK, Kaushal R, Williams DH, Bates DW. Analysis of medication-related malpractice claims: causes, preventability, and costs. Arch Intern Med. 2002;162(21):2414-2420.
65. Gurwitz JH, Field TS, Harrold LR, et al. Incidence and preventability of adverse drug events among older persons in the ambulatory setting. JAMA. 2003;289(9):1107-1116.
66. Neumiller JJ, Setter SM, White AM, et al. Advances in Patient Safety and Medical Liability: Medication Discrepancies and Potential Adverse Drug Events During Transfer of Care from Hospital to Home. Available at https://www.ahrq.gov/patient-safety/reports/liability/neumiller.html. Last accessed February 18, 2025.
68. Internal Medicine Closed Claims Study. Available at https://www.thedoctors.com/articles/internal-medicine-closed-claims-study/. Last accessed January 26, 2022.The Doctors Company. Diagnostic and Interventional Radiology Closed Claims Study. Available at https://www.thedoctors.com/articles/diagnostic-and-interventional-radiology-closed-claims-study/. Last accessed February 18, 2025.
69. The Doctors Company. Hospitalist Closed Claims Study. Available at https://www.thedoctors.com/articles/hospitalist-closed-claims-study/#4. Last accessed February 18, 2025.
70. Brown TW, McCarthy ML, Kelen GD, Levy F. An epidemiologic study of closed emergency department malpractice claims in a national database of physician malpractice insurers. Acad Emerg Med. 2010;17(5):553-560.
71. Roberts RG. Seven reasons family doctors get sued and how to reduce your risk. Fam Pract Manage. 2003;10(3):29-34.
72. Broker B. Reducing your risk of malpractice claims. Available at https://physiciansnews.com/2005/04/13/reducing-your-risk-of-malpractice-claims/.Last accessed February 18, 2025.
73. Mazor KM, Simon SR, Yood RA, et al. Health plan members' views about disclosure of medical errors. Ann Intern Med. 2004;140(6):409-418.
74. Rubin RJ, Mendelson DN. How much does defensive medicine cost? J Am Health Policy. 1994;4(4):7-15.
75. Bernstein J, MacCourt D, Abramson BD. Topics in medical economics: medical malpractice. J Bone Joint Surg. 2008;90(8):1777-1782.
76. Katz DA, Williams GC, Brown RL, et al. Emergency physicians' fear of malpractice in evaluating patients with possible acute cardiac ischemia. Ann Emerg Med. 2005;46(6):525-533.
77. Studdert DM, Mello MM, Sage WM, et al. Defensive medicine among high-risk specialist physicians in a volatile malpractice environment. JAMA. 2005;293(21):2609-2617.
78. Nahed BV, Babu MA, Smith TR, Heary RF. Malpractice liability and defensive medicine: a national survey of neurosurgeons. PLoSOne. 2012;7(6):e39237.
79. Mount Sinai. Press Release: Vast Majority of Physicians Practice "Defensive Medicine" According to New Physician Survey. Available at https://www.mountsinai.org/about/newsroom/2010/vast-majority-of-physicians-practice-defensive-medicine-according-to-new-physician-survey. Last accessed February 18, 2025.
80. Sethi MK, Obremskey WT, Natividad H, Mir HR, Jahanqir AA. Incidence and costs of defensive medicine among orthopedic surgeons in the United States: a national survey study. Am J Orthop (Belle Mead NJ). 2012;41(2):69-73.
81. Jena AB, Schoemaker L, Bhattacharya J, Seabury SA. Physician spending and subsequent risk of malpractice claims: observational study. BMJ. 2015;4:351:h5516.
82. Mello MM, Chandra A, Gawande AA, Studdert DM. National costs of the medical liability system. Health Aff (Millwood). 2010;29(9):1569-1577.
85. Davenport J. Documenting high-risk cases to avoid malpractice liability. Fam Pract Manage. 2000;7(9):33-36.
86. Elmore JG, Taplin SH, Barlow WE, et al. Does litigation influence medical practice? The influence of community radiologists' medical malpractice perceptions and experience on screening mammography. Radiology. 2005;236(1):37-46.
87. Charles SC, Pyskoty CE, Nelson A. Physicians on trial: self-reported reactions to malpractice trials. West J Med. 1988;148(3):358-360.
88. Charles SC, Wilbert JR, Kennedy EC. Physicians' self-reports of reactions to malpractice litigation. Am J Psychiatry. 1984;141:563-565.
89. Reyes R, Reyes C. At your defense: medical malpractice stress syndrome takes its toll. EMN. 2017;39(2):19.
90. Beckman HB, Markakis KM, Suchman AL, Frankel RM. The doctor-patient relationship and malpractice: lessons from plaintiff depositions. Arch Intern Med. 1994;154(12):1365-1370.
91. Studdert DM, Mello MM, Gawande AA, Brennan TA, Wang YC. Disclosure of medical injury to patients: an improbable risk management strategy. Health Aff. 2007;26(1):215-226.
92. American Congress of Obstetricians and Gynecologists Committee on Health Care for Underserved Women, Committee on Patient Safety and Quality Improvement. Effective Patient-Physician Communication. Available at https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2014/02/effective-patient-physician-communication. Last accessed February 18, 2025.
93. Stelfox HT, Gandhi TK, Orav EJ, Gustafson ML. The relation of patient satisfaction with complaints against physicians and malpractice lawsuits. Am J Med. 2005;118(10):1126-1133.
94. Adamson TE, Tschann JM, Gullion DS, Oppenberg AA. Physician communication skills: a complex relationship. West J Med. 1989;150(3):356-360.
95. Black WC, Nease RF Jr, Tosteson AN. Perceptions of breast cancer risk and screening effectiveness in women younger than 50 years of age. J Natl Cancer Inst. 1995;87(10):720-731.
96. Institute for Healthcare Improvement. Patient Safety Essentials Toolkit: Ask Me 3. Available at https://www.ihi.org/sites/default/files/SafetyToolkit_AskMe3.pdf. Last accessed February 18, 2025.
98. Committee on Health Literacy Board on Neuroscience and Behavioral Health. Health Literacy: A Prescription to End Confusion. Washington, DC: The National Academies Press; 2004.
99. Kirsch IS, Jungeblut A, Jenkins L, Kolstad A. Adult Literacy in America: A First Look at the Findings of the National Adult Literacy Survey (NALS). Washington, DC: National Center for Education Statistics, U.S. Department of Education; 1993.
100. Kutner M, Greenberg E, Jin,Y, Paulsen C, White S. The Health Literacy of America's Adults: Results from the 2003 National Assessment of Adult Literacy. Washington, DC: National Center for Education Statistics; 2006.
101. Center for Health Care Strategies. Health Literacy Fact Sheets. Available at https://www.chcs.org/resource/health-literacy-fact-sheets/. Last accessed February 18, 2025.
102. U.S. Census Bureau. Selected Social Characteristics in the United States: 2023 American Community Survey 5-Year Estimates. Available at https://data.census.gov/table/ACSDP5Y2023.DP02?q=selected%20social%20characteristics. Last accessed February 18, 2025.
103. Karliner LS, Napoles-Springer AM, Schillinger D, Bibbins-Domingo K, Pérez-Stable EJ. Identification of limited English proficient patients in clinical care. J Gen Intern Med. 2008;23(10):1555-1560.
104. Shepard S. Challenges in cultural diversity: protect your patients and yourself. Doctor's Advocate. 2007;4.
105. Sevilla Mátir JF, Willis DR. Using bilingual staff members as interpreters. Fam Pract Manage. 2004;11(7):34-36.
106. Ngo-Metzger Q, Massagli MP, Clarridge BR, et al. Linguistic and cultural barriers to care: perspectives of Chinese and Vietnamese immigrants. J Gen Intern Med. 2003;18(1):44-52.
107. Flores G. Language barriers to health care in the United States. N Engl J Med. 2006;355(3):229-231.
108. Flores G. The impact of medical interpreter services on the quality of health care: a systematic review. Med Care Res Rev. 2005;62(3):255-299.
109. Karliner LS, Jacobs EA, Chen AH, Mutha S. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv Res. 2007;42(2):727-754.
110. The National Board of Certification for Medical Interpreters. Available at https://www.certifiedmedicalinterpreters.org. Last accessed February 18, 2025.
111. Levinson W, Roter DL, Mullooly JP, Dull VT, Frankel RM. Physician-patient communication: the relationship with malpractice claims among primary care physicians and surgeons. JAMA. 1997;277(7):553-559.
112. Hickson GB, Clayton EW, Entman SS, et al. Obstetricians' prior malpractice experience and patients' satisfaction with care. JAMA. 1994;272(20):1583-1587.
113. Calvert JF Jr, Hollander-Rodriguez J, Atlas M, Johnson KE. Clinical inquiries: what are the repercussions of disclosing a medical error? J Fam Pract. 2008;57(2):124-125.
114. Gallagher TH, Waterman AD, Ebers AG, Fraser VJ, Levinson W. Patients' and physicians' attitudes regarding the disclosure of medical errors. JAMA. 2003;289(8):1001-1007.
115. Mazor KM, Reed GW, Yood RA, Fischer MA, Baril J, Gurwitz JH. Disclosure of medical errors: what factors influence how patients respond? J Gen Intern Med. 2006;21(7):704-710.
116. Schwappach DLB, Koeck CM. What makes an error unacceptable? A factorial survey on the disclosure of medical errors. Int J Qual Health Care. 2004;16(4):317-326.
118. Liebman CB, Hyman CS. A mediation skills model to manage disclosure of errors and adverse events to patients. Health Aff. 2004;23(4):22-32.
120. Kaldjian LC, Jones EW, Wu BJ, Forman-Hoffman VL, Levi BH, Rosenthal GE. Disclosing medical errors to patients: attitudes and practices of physicians and trainees. J Gen Intern Med. 2007;22(7):988-996.
121. Mazor KM, Simon SR, Gurwitz JH. Communicating with patients about medical errors: a review of the literature. Arch Intern Med. 2004;164(15):1690-1697.
122. Kachalia A, Shojania KG, Hofer TP, Piotrowski M, Saint S. Does full disclosure of medical errors affect malpractice liability? The jury is still out. Jt Comm J Qual Saf. 2003;29(10):503-511.
123. Finkelstein D, Wu AW, Holtzman NA, Smith MK. When a physician harms a patient by a medical error: ethical, legal, and risk-management considerations. J Clin Ethics. 1997;8(4):330-335.
124. American College of Physicians. Ethics manual, fourth edition. Ann Intern Med. 1998;128(7):576-594.
125. National Quality Forum. Safe Practices for Better Healthcare—2010 Update. Available at https://www.qualityforum.org/Publications/2010/04/Safe_Practices_for_Better_Healthcare_%E2%80%93_2010_Update.aspx. Last accessed February 18, 2025.
127. Sorry Works! Available at https://www.sorryworks.net. Last accessed February 18, 2025.
128. Gallagher TH, Garbutt JM, Waterman AD, et al. Choosing your words carefully: how physicians would disclose harmful medical errors to patients. Arch Intern Med. 2006;166(15):1585-1593.
129. Massachusetts Coalition for the Prevention of Medical Errors. When Things Go Wrong: Responding to Adverse Events. A Consensus Statement of the Harvard Hospitals. Available at http://www.macoalition.org/documents/respondingToAdverseEvents.pdf. Last accessed February 18, 2025.
130. Agency for Healthcare Research and Quality. Patient Safety Primer: Disclosure of Errors. Available at https://psnet.ahrq.gov/primer/disclosure-errors. Last accessed February 18, 2025.
131. Kraman SS, Hamm G. Risk management: extreme honesty may be the best policy. Ann Intern Med. 1999;131(12):963-967.
132. Wu AW, Huang IC, Stokes S, Pronovost PJ. Disclosing medical errors to patients: it's not what you say, it's what they hear. J Gen Intern Med. 2009;24(9):1012-1017.
133. Morton R. Informed Consent: Substance and Signature. Available at https://www.thedoctors.com/articles/informed-consent-substance-and-signature/. Last accessed February 18, 2025.
134. Burns P, Keogh I, Timon C. Informed consent: a patients' perspective. J Laryngol Otol. 2005;119(1):19-22.
135. Murphy JB. Benefits and challenges of informed consent [editorial]. Mayo Clin Proc. 2008;83(3):272-273.
136. Langdon IJ, Hardin R, Learmonth ID. Informed consent for total hip arthroplasty: does a written information sheet improve recall by patients? Ann Roy Coll Surg Engl. 2002;84(6):404-408.
137. Rossi M, McClellan R, Chou L, Davis K. Informed consent for ankle fracture surgery: patient comprehension of verbal and videotaped information. Foot Ankle Int. 2004;25(10):756-762.
138. Barry MJ, Bennett CL, Stacey D, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2011;10:CD001431.
139. Stacey D, Légaré F, Lewis K, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017;(4):CD001431.
143. Muñana C, Kirzinger A, Brodie M. Data Note: Public's Experiences With Electronic Records. Available at https://www.kff.org/other/poll-finding/data-note-publics-experiences-with-electronic-health-records/. Last accessed February 18, 2025.
144. Virapongse A, Bates DW, Shi P, et al. Electronic health records and malpractice claims in office practice. Arch Intern Med. 2008;168(21):2362-2367.
145. The Doctors Company. Electronic Health Records Continue to Lead to Medical Malpractice Suits. Available at https://www.thedoctors.com/articles/electronic-health-records-continue-to-lead-to-medical-malpractice-suits/. Last accessed February 18, 2025.
146. Stanford Medicine. What Physicians Want From EHRs. (How Doctors Feel About Electronic Health Records: National Physician Poll by The Harris Poll). Available at https://med.stanford.edu/ehr/electronic-health-records-poll-results.html. Last accessed February 18, 2025.
147. Elgert S. Reliability science: reducing the error rate in your practice. Fam Pract Manag. 2005;12(9):59-63.
149. Friedman CP, Gatti GG, Franz TM, et al. Do physicians know when their diagnoses are correct? Implications for decision support and error reduction. J Gen Intern Med. 2005;20(4):334-339.
150. Elder NC, McEwen TR, Flach JM, Gallimore JJ. Management of test results in family medicine offices. Ann Fam Med. 2009;7(4):343-351.
151. Bookhaker EA, Ward RE, Uman JE, McCarthy BD. Patient notification and follow-up of abnormal test results. Arch Intern Med. 1996;156(3):327-331.
152. Mold JW, Cacy DS, Dalbir DK. Management of laboratory test results in family practice. J Fam Pract. 2000;49(8):709-715.
153. Casalino LP, Dunham D, Chin MH, et al. Frequency of failure to inform patients of clinically significant outpatient test results. Arch Intern Med. 2009;169(12):1123-1129.
154. Watson J, Salisbury C, Whiting PF, Hamilton WT, Banks J. 'I guess I'll wait to hear' – communication of blood test results in primary care a qualitative study. Br J Gen Pract. 2022;72(723):e747-e754.
155. Baylis D, Price J, Bowie P. Content analysis of 50 clinical negligence claims involving test results management systems in general practice. BMJ Open Qual. 2018;7(4):e000463.
156. Murff HJ, Gandhi TK, Karson AK, et al. Primary care physician attitudes concerning follow-up of abnormal test results and ambulatory decision support systems. Int J Med Inform. 2003;71(2-3):137-149.
157. Poon EG, Gandhi TK, Sequist TD, Murff HJ, Karson AS, Bates DW. "I wish I had seen this test result earlier!": dissatisfaction with test result management systems in primary care. Arch Intern Med. 2004;164(20):2223-2228.
158. Zapka J, Taplin SH, Price RA, Cranos C, Yabroff R. Factors in quality care: the case of follow-up to abnormal cancer screening tests—problems in the steps and interfaces of care. J Natl Cancer Inst Monogr. 2010;2010(40):58-71.
159. Haas JS, Cook EF, Puopolo AL, Burstin HR, Brennan TA. Differences in the quality of care for women with an abnormal mammogram or breast complaint. J Gen Intern Med. 2000;15(5):321-328.
160. Marcus AC, Crane LA, Kaplan CP, et al. Improving adherence to screening follow-up among women with abnormal Pap smears: results from a large clinic-based trial of three intervention strategies. Med Care. 1992;30(3):216-230.
161. Thomsen LA, Winterstein AG, Sondergaard B, Haugbolle LS, Melander A. Systematic review of the incidence and characteristics of preventable adverse drug events in ambulatory care. Ann Pharmacother. 2007;41(9):1411-1426.
162. Ranum D. Electronic Health Records Continue to Lead to Medical Malpractice Suits. Available at https://www.thedoctors.com/articles/electronic-health-records-continue-to-lead-to-medical-malpractice-suits/. Last accessed February 18, 2025.
163. Odukoya OK, Stone JA, Chui MA. E-prescribing errors in community pharmacies: exploring consequences and contributing factors. Int J Med Inform. 2014;83(6):427-437.
164. Committee on Identifying and Preventing Medication Errors Institute of Medicine. Preventing Medication Errors: Quality Chasm Series. Washington, DC: The National Academies Press; 2007.
165. Willis DR, Zerr A. Terminating a patient: is it time to part ways? Fam Pract Manag. 2005;12(8):34-38.
166. AMA Code of Medical Ethics. 1.1.5 Terminating a Patient-Physician Relationship. Available at https://code-medical-ethics.ama-assn.org/sites/amacoedb/files/2022-08/1.1.5.pdf. Last accessed February 18, 2025.
167. Cahill R. Medical and Dental Record Retention. Available at https://www.thedoctors.com/articles/medical-and-dental-record-retention. Last accessed February 18, 2025.
Mention of commercial products does not indicate endorsement.