This course is a departure from traditional instruction on clinical supervision where the emphases tend to be on models of counselor development and approaches specific to clinical supervision. Taking the person-centered values of empathy, unconditional positive regard, and congruence, this workshop will teach you how to work with supervisees in a manner that will honor their perspectives and experience and thus maximize their development as counselors. Supervisors are encouraged to "step into the shoes" of their supervisees and remember what it was like to receive clinical supervision as a way of building stronger working alliances with those they supervise. Special attention is devoted to using motivational enhancement principles in working with resistant supervisees, and various legal/ethical and pragmatic scenarios are also incorporated into the content.
- INTRODUCTION
- FOUNDATIONS: TAKING A PERSON-CENTERED APPROACH TO CLINICAL SUPERVISION
- CONSULTATION AND THE PERSON-CENTERED APPROACH
- DEFINING THE PERSON-CENTERED APPROACH TO SUPERVISION
- PRACTICING EMPATHY AND THE ART OF SUPERVISION
- CLINICAL DEVELOPMENT AND FORMATION
- LEGAL AND ETHICAL ISSUES IN SUPERVISION
- SELF-CARE AS A SUPERVISION ISSUE
- CONCLUSION
- GLOSSARY
- APPENDIX
- Works Cited
This course is designed for professional clinicians, including counselors, social workers, therapists, and pastoral counselors, who supervise others, clinically and/or administratively.
The purpose of this course is to help supervisors or potential supervisors in the human services or helping professions to more effectively work with those they are entrusted to supervise.
Upon completion of this course, you should be able to:
- Identify and discuss common problems in supervising counselors/clinicians.
- Define the basic components of clinical supervision.
- Discuss the role of consultation in effective work with supervisees.
- Describe what the psychotherapeutic professions reveal about the importance of empathy and therapeutic alliance in treatment (regardless of specific method or model).
- Apply these principles of empathy to the practice of clinical supervision.
- Articulate and discuss the stages of counselor development as they relate to the person- centered approach to clinical supervision.
- Utilize motivational interviewing approaches with resistant supervisees.
- Incorporate empathetic, person-centered principles into ethical and legal decision making.
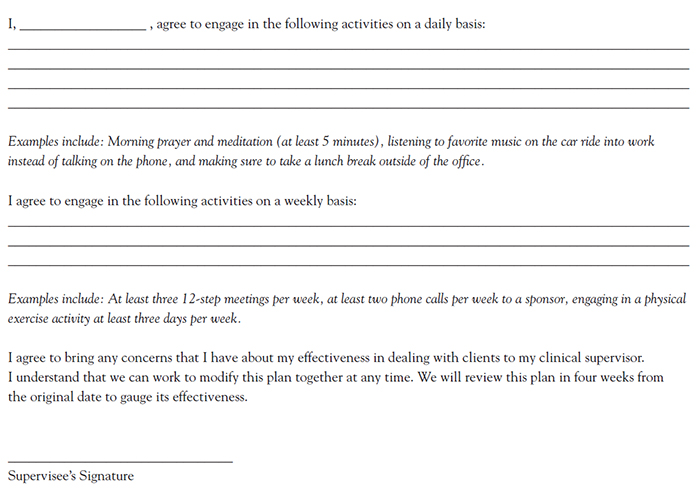
- Develop a self-care plan that takes into account empathetic approaches to self and others.
- Assist others in developing both work plans and self-care plans.
Jamie Marich, PhD, LPCC-S, REAT, RYT-500, RMT, (she/they) travels internationally speaking on topics related to EMDR therapy, trauma, addiction, expressive arts, and mindfulness while maintaining a private practice and online education operation, the Institute for Creative Mindfulness, in her home base of northeast Ohio. She is the developer of the Dancing Mindfulness approach to expressive arts therapy and the developer of Yoga for Clinicians. Dr. Marich is the author of numerous books, including EMDR Made Simple, Trauma Made Simple, and EMDR Therapy and Mindfulness for Trauma Focused Care (written in collaboration with Dr. Stephen Dansiger). She is also the author of Process Not Perfection: Expressive Arts Solutions for Trauma Recovery. In 2020, a revised and expanded edition of Trauma and the 12 Steps was released. In 2022 and 2023, Dr. Marich published two additional books: The Healing Power of Jiu-Jitsu: A Guide to Transforming Trauma and Facilitating Recovery and Dissociation Made Simple. Dr. Marich is a woman living with a dissociative disorder, and this forms the basis of her award-winning passion for advocacy in the mental health field.
Contributing faculty, Jamie Marich, PhD, LPCC-S, REAT, RYT-500, RMT, has disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
Alice Yick Flanagan, PhD, MSW
The division planner has disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
Sarah Campbell
The Director of Development and Academic Affairs has disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
The purpose of NetCE is to provide challenging curricula to assist healthcare professionals to raise their levels of expertise while fulfilling their continuing education requirements, thereby improving the quality of healthcare.
Our contributing faculty members have taken care to ensure that the information and recommendations are accurate and compatible with the standards generally accepted at the time of publication. The publisher disclaims any liability, loss or damage incurred as a consequence, directly or indirectly, of the use and application of any of the contents. Participants are cautioned about the potential risk of using limited knowledge when integrating new techniques into practice.
It is the policy of NetCE not to accept commercial support. Furthermore, commercial interests are prohibited from distributing or providing access to this activity to learners.
Supported browsers for Windows include Microsoft Internet Explorer 9.0 and up, Mozilla Firefox 3.0 and up, Opera 9.0 and up, and Google Chrome. Supported browsers for Macintosh include Safari, Mozilla Firefox 3.0 and up, Opera 9.0 and up, and Google Chrome. Other operating systems and browsers that include complete implementations of ECMAScript edition 3 and CSS 2.0 may work, but are not supported. Supported browsers must utilize the TLS encryption protocol v1.1 or v1.2 in order to connect to pages that require a secured HTTPS connection. TLS v1.0 is not supported.
The role of implicit biases on healthcare outcomes has become a concern, as there is some evidence that implicit biases contribute to health disparities, professionals' attitudes toward and interactions with patients, quality of care, diagnoses, and treatment decisions. This may produce differences in help-seeking, diagnoses, and ultimately treatments and interventions. Implicit biases may also unwittingly produce professional behaviors, attitudes, and interactions that reduce patients' trust and comfort with their provider, leading to earlier termination of visits and/or reduced adherence and follow-up. Disadvantaged groups are marginalized in the healthcare system and vulnerable on multiple levels; health professionals' implicit biases can further exacerbate these existing disadvantages.
Interventions or strategies designed to reduce implicit bias may be categorized as change-based or control-based. Change-based interventions focus on reducing or changing cognitive associations underlying implicit biases. These interventions might include challenging stereotypes. Conversely, control-based interventions involve reducing the effects of the implicit bias on the individual's behaviors. These strategies include increasing awareness of biased thoughts and responses. The two types of interventions are not mutually exclusive and may be used synergistically.
#76863: Clinical Supervision: A Person-Centered Approach
A horrible supervisor has a huge impact on job satisfaction and performance. Most people can relate to the feeling of dread the seemingly authoritarian command of those in power can cause. In an ideal sense, a supervisor is supposed to be a mentor, a leader to learn from and hopefully to emulate as part of professional formation. Yet for a variety of reasons, these relationships, whether they be of a boss-employee, supervisor-supervisee, or mentor-protégé variety, can go horribly wrong. Although incompetence or unwillingness to accept feedback from those being led can be a factor in these troublesome dynamics, more often the problems seem to arise from unpreparedness on the part of the supervisor to work with people in a respectful way that manages dynamics of power, responsibility, and humanity.
The purpose of this course is to help supervisors or potential supervisors in the human services or helping professions to more effectively work with those they are entrusted to supervise. As will be explored, the supervisory relationship in the helping professions is unique because it implies more than just management, it entails genuine leadership in the formation of professionals who are typically new to the professions. Because respecting the personhood of the professional being supervised is paramount to a successful supervisory dynamic in the helping professions, it is important that the same person-centered principles used with clients (e.g., empathy, unconditional positive regard, congruence) be incorporated into work with supervisees. This course will address how to work these principles into supervision within traditional frameworks for clinical supervision. Although traditional models and approaches will be covered, in addition to ancillary issues such as legal/ethical management and monitoring self-care of your supervisees, learners are encouraged to think outside of the proverbial box when it comes to incorporating these person-centered elements. Just as there are a variety of models and theories in the helping professions to guide the execution of psychotherapy, there are a variety of models available to guide the supervision process; the developmental model, the psychodynamic model, the skills-based model, the systemic model, and the blended model are among the most popular. Whatever model is chosen to guide supervision, person-centered principles of empathy, congruence, and unconditional positive regard can be implemented to enhance delivery of supervisory services. Thus, the focus of this course is more practical, as opposed to academic. As such, learners are encouraged to view this course as an exercise in their professional development as a supervisor. Staying with the person-centered theme of the course, take time to reflect on your own experiences and be mindful of how you respond (or in the case of past reflections, responded) as a person. Reflection questions are included throughout the course to facilitate this process; the questions may also be used as journal prompts or guides for meditation. Above all, take from this course what you most need, personally and professionally. By approaching this course with an open mind to the personal and the professional, you will be best able to put person-centered supervision into action.
Clinical supervision trainings are notoriously theoretical. But even clinical supervision trainings can be interesting if they meet the practical needs of those taking the course. Most states require some form of continuing education specific to supervision in order to acquire and/or to obtain supervisory endorsements on clinical licenses. Thus, it is imperative that operational foundations of various definitions and concepts connected to supervision be discussed.
Supervision can have different meanings for different people. The word origin traces back to 17th century Latin, literally meaning "to look over." In this most basic definition of the word, it is clear it has multiple applications: parents can supervise their children at play, leaders can supervise volunteers, and employers can supervise those under their employ. In some professions, the supervisory relationship is simply one of a boss overseeing his or her employees. For instance, a movie theater manager may be responsible for making sure that his or her employees report to work on time and perform the tasks of their job description, like selling concessions, taking tickets, and sweeping theaters after shows. The manager may also be responsible for conducting quarterly evaluations and writing up or otherwise punishing an employee if he or she consistently fails to meet the tasks of the job. Ensuring that employees complete these tasks with efficiency is vital to ensuring satisfactory customer service, a priority for any person or entity running a business.
In consumer-driven businesses, supervisors can choose to be authoritarian, simply carrying out the function of management, or they can choose to see themselves more as mentors to those they supervise, helping supervisees grow in their job or their chosen profession. While taking on this mentorship component is an option in conventional business, it becomes a necessity in the helping professions. This combined mentorship and management component is the essence of clinical supervision. In examining educational trends in the history of the helping professions, discussion about clinical supervision is a relatively newer idea. In fact, there is little direct, empirical evidence within mental health professions to show that clinical supervision has an impact on clinician behavior and thus service quality with clients [1]. This is supported by reviews of the literature, with the majority of peer-reviewed literature on clinical supervision reading as theoretical in nature. Rather, the helping professions adopted the practice of clinical supervision as a measure of good common sense, carrying on the tradition of the master working with the apprentice that has existed in many professions for centuries.
Historically, Kadushin's definition of supervision is cited as one of the first guiding descriptions of what constitutes clinical supervision [2]. He described clinical supervision as, "an administrative and clinical process designed to facilitate the counselor's ability to deliver the best possible services to clients, both quantitative and qualitative, in accordance with agency policies and procedures, and the context of a positive relationship between counselor and supervisor" [2]. This foundational definition still resonates in the present day, especially because the duplicity of the administrative and clinical functions is acknowledged. Moreover, the imperative of quality supervision as a client care issue is directly stated in this seminal definition. In the Handbook of Clinical Social Worker Supervision, clinical supervision is defined as an interactional process in which a supervisor has been assigned or designated to assist in and direct the practice of supervisees in the areas of teaching, administration, and helping [3]. Kadushin's original thoughts, originating in social work, have been long regarded by the field of social work, with widespread acceptance in the field of clinical supervision as an effective practice [4]. However, the various helping professions have established their own definitions.
In the counseling field, clinical supervision is best defined as a process whereby consistent observation and evaluation of the counseling process is provided by a trained and experienced professional who recognizes and is competent in the unique body of knowledge and skill required for professional development [5]. In counselor education, supervision involves facilitating the counselor's personal and professional development as well as promoting counselor competencies for the welfare of the client [6].
The purpose of supervision in substance abuse counseling is to bring about change in the knowledge, skills, and behavior of another individual, typically one with less training and experience than the supervisor. Regardless of various models or definitions, there are five essential components that constitute supervision in the field of substance abuse counseling [6]:
An experienced supervisor
Actual clients in clinical settings
"Do no harm"/welfare focus for both the clients and the supervisee
Monitoring performance through direct or indirect observation
The goal of changing the counselor's behavior
Finally, in psychology, supervision is a distinct professional activity in which education and training aimed at developing science-informed practice are facilitated through a collaborative, interpersonal process. It involves observation, evaluation, feedback, the facilitation of supervisee self-assessment, and the acquisition of instruction and skills by instruction, modeling, and mutual problem solving [7]. Although there are solid merits in each definition, this last description serves as the best operational definition for this course. Not only does it cover many of the components of clinical supervision and the activities involved, but it emphasizes two key components that are essential to person-centered supervision. First, like in person-centered therapy, supervision is a collaborative process. Second, clinical supervision is educational in its nature. Although there may be managerial and legal/ethical implications in any given supervisory relationship, supervision is fundamentally an educational activity, a critical part of a helper's professional formation.
Formation is a term often used in seminaries and monastic life to describe the process by which a person responding to his or her vocation (or "calling") learns how to live the calling to the fullest. Formation entails receiving mentorship and formal instruction and growing through the initial trials or tests, often called a novitiate or probationary period. So much of what new helping professionals experience during their initial internships and first several years in the field parallels the concept of formation, and by choosing to view supervision as a function in assisting formation, supervisors can truly help new professionals to live their callings to help to the fullest. As British psychotherapists Peter Hawkins and Robin Shohet express, "supervision can be a place where a living profession breathes and learns" [8]. This is a beautiful concept, yet it is up to supervisors to create and foster an environment that is free of professional suffocation. This course will explore how adopting person-centered concepts into the function of supervision is optimal for establishing and maintaining such an environment.
Before delving into person-centered concepts and how to apply them to supervision, consider how taking on a consultant's role within the context of supervision may help a new professional to grow into the fullness of his or her calling. It is important to make an essential distinction, from the standpoint of responsibility, between a supervisor and a consultant. With technical, clinical supervision, in most states and within most organizations, the role of supervisor carries some form of responsibility. In essence, if the work of a counselor or helper is called into question, especially regarding an ethical breach, the supervisor will be questioned and may even be subjugated to legal or ethical responsibility if the counseling occurred under the umbrella of the supervisor's license or certification. A much higher degree of responsibility is implied with supervision compared to consultation, which can simply be defined as collaborating with a specialist who is called upon for his or her expert advice in the field, for instance, in matters of assessment, diagnosis, or treatment planning. Sears, Rudisill, and Mason-Sears describe a consultant as a "person with special knowledge, skills, or talent who makes needed expertise for clients available for a fee" [9]. When consultation services are provided, the consultant is being compensated for his or her opinion and guidance; there is no sense of responsibility or obligation implied in the relationship.
The hierarchical structure of the supervisory relationship can put a damper on supervision being a formational experience, and removing this element results in more of a consultant position; an enriching collaboration can result. To use terms often employed in the addiction recovery field, in consultation, the consultant can share his or her experiences, strengths, and hope with a consultee. Many who have achieved an independent status with their licensure and practice and who no longer require formal clinical supervision continue to engage in consultation with peers, colleagues, and administrative supervisors. The revised codes of many states encourage this consultation (and documentation of it) for continued growth in the profession [10,11]. Indeed, learning experiences can certainly be experienced by independent counselors no longer in need of formal, clinical supervision. Valuable lessons are learned through informal exchange of experience, strength, and hope with trusted colleagues.
Formal, clinical supervision may never be this casual because there is such a responsibility implied with the relationship, but consider how adopting some of the spirit of peer-to-peer consultation may help those supervisees to better relate to their supervisor. Implementing some of the same skills practiced in consultation (e.g., fostering confidence, supporting self-efficacy) work in supervision as well. These skills can be especially effective with professionals who may be new to the field but entered the helping professions as a second or third career and are not necessarily new to life. For instance, when supervising those who are older chronologically, taking on more of a consultation-based, collaborative mindset may allow for more effective supervision.
A clinical supervisor is someone who can play four primary roles: a teacher, a coach, a mentor, and a consultant. However, a myriad of other roles can emerge at any given time: an administrator, a liaison (between upper management and those being supervised), a champion of the underdog, a client care coordinator, and even an emergency therapist or helper if the supervisee is encountering an especially rough day on the job due to personal circumstances. As with juggling many life roles, it is best for the supervisee to wear one hat at a time, but due to circumstances in the fast paced world of human services, this is often impossible. Regardless of what role or roles are being juggled at any given time, the most effective clinical supervision takes place in the context of a solid relationship between supervisee and supervisor. One could visualize these different roles orbiting the sun like planets, with the relationship as the sun. This is also a good metaphor for the person-centered approach to therapy. Just as adopting person-centered principles like empathy and unconditional positive regard can work alongside many models, so too can applying person-centered approaches to your specific philosophy or model of supervising others. An approach is not a model in and of itself; rather, it is a mindset or attitude that can be applied to a variety of existent models.
One of the core principles of the person-centered approach to psychotherapy is empathy. It may be valuable to pause and reflect on what empathy means to you. Perhaps it is more of a feeling or a body-level, visceral reaction to a specific memory in which someone showed empathy in a difficult situation. Empathy is a human quality that can manifest in a variety of arenas, not just in psychotherapy, and it is perhaps the inherent compassion of empathy, shown amongst people, that makes it so powerful.
A colloquial phrase often intoned to explain empathy is being able to "step into the shoes" of another person. German philosopher Rudolf Lotze coined the term empathy, as a humanistic concept, in 1858. The German word Einfühlung literally translates as "in" and "feeling." The derivation is from the Greek empatheia, em meaning "in" and pathos defined as feeling. Interestingly, pathos is also the root of the words "passion" and "pain," two elements of living that are significant to human experience and, of course, to psychotherapy. Although English language dictionaries interpret these origins in a variety of ways, useful definition of empathy to those in service professions appears in Stedman's Medical Dictionary, which defines the term as the "direct identification with, understanding of, and vicarious experience of another person's situation, feelings, and motives" [12]. When it comes to having empathy for supervisees, this final word of the definition (motives) is a significant part of the process. Consider that every helper is drawn into the field for a certain reason or a variety of reasons; these reasons constitute the motive of a developing helper for being in the field in the first place. Motive is a fascinating component of empathy that is not often considered, but it can help one to appreciate another person's perspective. Appreciating an individual's perspective is a key factor in being able to mentor, to coach, and ultimately to work with that individual.
For psychotherapeutic professionals, empathy is often associated with the person-centered or humanistic approach to psychotherapy and its father, Dr. Carl Rogers. Along with other elements, such as unconditional positive regard for the client and congruence, practicing empathy is vital to adopting a person-centered approach. Rogers created a metaphor of empathy as a dance between a client and the helper serving the client in order to explain the concept [13]:
Being empathetic reflects an attitude of profound interest in the client's world of meanings and feelings. The therapist receives these communications and conveys appreciation and understanding, assisting the client to go further or deeper. The notion that this involves nothing more than a repetition of the client's last words is erroneous. Instead, an interaction occurs in which one person is a warm, sensitive, respectful companion in the typically difficult exploration of another's emotional world. The therapist's manner of responding should be individual, natural, and unaffected. When empathy is at its best, the two individuals are participating in a process comparable to that of a couple dancing, with the client leading and the therapist following.
If you re-read this passage, replacing the word client with supervisee, and the word therapist with supervisor, one has a good idea of the application of the metaphor. Consider whether or not this metaphor of "the dance" can make sense within the supervisory relationship.
On first reading, it may be concerning to think of giving supervisees this much autonomy, especially when one's license could be at risk if they end up going in an unforeseen direction. However, in any structured dance, one of the partners is the leader while the other is led. If one feels that he or she is being led erratically, they can halt the dance in order to make adjustments to correct the original problem. On the other hand, if both dancers try to lead, the overall training ultimately suffers. As scary as it may seem, the supervisees are the ones leading; they inform the supervisor of their needs and of where they need to go. One can best supervise by following their lead, knowing you have every right (and responsibility) to intervene if something is clearly wrong.
Psychiatrist Irvin Yalom is perhaps best known in the context of his text on group therapy [14]. However, one of his later works, The Gift of Therapy, may have a greater application to our professional formation as clinical supervisors [15]. In this text, published more than 30 years after his seminal piece on group therapy, Yalom declares that in spite of all his years writing about techniques, it really is the relationship that matters most [15].
Written in plain English as an "open letter" to young therapists, the book's thesis is that therapy should not be theory-driven, but relationship-driven. Yalom contends that our heightened sensibility to existential issues deeply influences the nature of the therapeutic relationship and the therapy itself [15]. According to this perspective, a therapist has no place forcing solutions, a piece of guidance that may be helpful in clinical work, especially with clients who seem to be labeled as "difficult" cases. This does not mean that supervisors should abandon theories, models, or technical training, but simply that letting humanity take precedence and focusing on building the relationship with supervisees should be a priority.
Although the relationship-based ideals expressed by Rogers and Yalom may sound humanistic but not exactly scientific, they are supported by the research literature. Several leaders in the field, in investigating what works in psychotherapy, assert through use of meta-analytic research and literature that the relationship is the vital ingredient in what makes therapy successful [16,17,18]. A term often used to refer to this concept is therapeutic alliance; however, in the context of clinical supervision, the term relational alliance is a better fit. A relational alliance is when two parties, such as a supervisor/supervisee, are engaging in a mutually respectful, trusting interaction, working toward a goal or benefit.
In the text The Heart and Soul of Change: What Works in Psychotherapy, Duncan, Miller, Wampold, and Hubbard assert that the collaborative, therapeutic alliance between client and clinician (and perhaps by extension the supervisee and supervisor) is a primary factor in determining successful therapy outcomes and is more important than the specific execution of therapeutic protocols [19]. They also stressed that obtaining continuous client feedback throughout the therapeutic process is critical to enhancing client care. When this literature is examined as a whole, it is clear that little difference exists among the specific factors (e.g., technical elements) of researched therapeutic therapies. Rather, there are a series of four common factors among these therapies that seem to be contributing to change. These common factors are: the clients and their extra-therapeutic factors (e.g., what they bring to the table in therapy and situations out of the control of the clinician); models and techniques that work to engage and inspire an individual client; the therapeutic relationship/alliance; and therapist factors. Interestingly, these four common factors were first proposed and published by psychiatrist Saul Rosenzweig in 1936, predating the work of Rogers and Yalom [20]. Rosenzweig, who grew discouraged with the "therapy wars" waging around him at the time, asserted the fields need to focus on the factors that all good therapies have in common instead of fighting over what is superior about a specific approach or technique. By respecting the common factors and focusing on these simple, humanistic elements, therapists can best meet people where they are coming in to therapy.
Respecting the common factors, as a therapist or a supervisor, does not give one permission to throw competence to the wind and abandon theory, technique, or model altogether. Rather, it is important to reconceptualize their meanings to the overall helping process. According to Duncan, Miller, Wampold, and Hubbard [19]:
…We conclude that what happens (when a client is confronting negative schema, addressing family boundaries, or interpreting transference) is less important than the degree to which any particular activity is consistent with the therapist's beliefs and values (allegiances) while concurrently fostering the client's hope (expectations). Allegiance and expectancy are two sides of the same coin: the faith of both the therapist and the client in the restorative power and credibility of the therapy's rationale and related rituals. Though rarely viewed this way, models and techniques work best when they engage and inspire the participants.
Norcross arrived at similar conclusions in Psychotherapy Relationships that Work: Therapist Contributions and Responsiveness to Patients [21]. Using a collection of empirical research as part of an American Psychological Association Task Force, Norcross concluded that the therapy relationship, together with discrete method, influences treatment outcomes. Norcross further concluded that therapists can hone these relational elements and that it is their responsibility to tailor these skills to the needs of individual patients. Thus, the relationship should drive the theory, not the other way around, which is concomitant to Yalom's contentions.
The next step is applying these principles to the practice of clinical supervision. By accepting that the same person-centered concepts used with clients can be applied to supervisees, a better connection (or relational alliance) may be established. There are many ways to conduct supervision, just as there are a myriad of ways to conduct psychotherapy; the great common thread is to appeal to the most basic components of personhood. Supervisees are, above anything else, humans, and embracing this humanity as opposed to their status as a supervisee helps them to grow to their fullest potential. Supervision is a process that supervisees can view as a punitive chore, and many who have had negative experiences with supervisors have viewed it as such. So, consider how the field can be changed by taking an institution that is often dreaded and approaching it as a safe container in which growth can occur and potential can be explored.
In addition, there is a potential to achieve tremendous progress by focusing on commonalities as opposed to divisive differences. This humanistic principle is evident in Rosenzweig's common factors. Supervisors can teach those they supervise and work with them to implement understanding into their work. However, it can be beneficial to address this idea of focusing on what the various approaches to supervision have in common in order to best meet supervisees where they are in the supervisory process. Powell captured the spirit of Rosenzweig's common factors in psychotherapy with his five common components of supervision [6]. Powell noted that there are many definitions of what constitutes supervision in the various helping professions, so it is important to look at the commonalities in these various definitions. To review, these five common elements are:
An experienced supervisor
Actual clients in clinical settings
"Do no harm"/welfare of both clients and the supervisee
Monitoring performance through direct or indirect observation
The goal of changing the counselor's behavior
These common elements show that various models can work, as long as they meet these criteria. Just as it is important for therapists to have a variety of different models or techniques on hand in order to engage and inspire clients, it is important for supervisors to have a variety of ways to work with a supervisee. This logic is the ultimate representation of clinical common sense; just as no two clients are alike, no two supervisees are alike. Embracing this logic is a hallmark of putting person-centered supervision into action.
Powell writes about the importance of non-malfeasance, or doing no harm, to both clients and supervisees [6]. Considering the emotional welfare of the supervisee in addition to that of the client represents a person-centered value that clinical supervisors often neglect, especially those who are overly administrative in their mindsets or those who see it as their duty to shape a new generation of therapists in their image. Respecting the individual dignity of a supervisee is not only a person-centered concept, it is a way to put non-malfeasance into action.
Putting the person-centered value of empathy into action as a supervisor is based on remembering what it was like to be supervised. It also entails being willing to step into the shoes of a supervisee and consider what he or she may be going through at any point in professional formation. As will be discussed in the next session, there are ways to build empathy and cultivate putting it into action. Although some supervisors and counselors may naturally be more empathetic than others, empathy is an action word, and as a person-centered value, it can be practiced and built.
Fostering critical thinking and putting the person-centered principles covered thus far into action is the next step in building a supervisory practice. To best do this, this section will explore case studies of four very different supervisees in the helping professions and consider the supervisory strategies for each person, depending on context. The supervisees are Ms. V, Mr. B, Ms. T, and Mr. N.
Ms. V is a white, heterosexual woman, 26 years of age. Assigned to a public mental health agency, she is in the internship phase of a Master's degree program in clinical counseling at a small, Christian university. Ms. V opted to go to graduate school immediately after finishing her Bachelor's degree in psychology. Her initial motivation for studying psychology was to help people, and she chose to do this despite the protests of her upper middle-class parents, who believed that there was no "future" (financially) in the psychotherapeutic professions. Partially to ease their protests and partially to "get on" with a career, she entered graduate school. Ms. V has found working with clients to be quite a struggle. She went into the field with every good intention of helping people, and she believed it was part of her spiritual path. However, the first time a client from a background different to hers, a tall, African American man on welfare, towered over her and told her that she "didn't know what she was talking about," Ms. V melted down and spent the rest of the day in her office crying. She called off from her site duties for the rest of the week, citing illness. At this point, Ms. V is wondering if a career in counseling is really the best fit for her because of her discouraging experiences working with clients. Yet the thought of going through a Master's degree program and not using it, especially when her parents paid and supported her through the program, is a shaming prospect to her. At this point, she is at a juncture and feels trapped.
Mr. B is a homosexual man, 38 years of age, of multiple ethnicities. (His mother was born to a Jamaican father and a white mother, and his father was of Dominican origin.) Mr. B is recovering from a substance use disorder (heroin and alcohol), having amassed three years of clean time in his chosen twelve-step program. A machinist in his first profession, Mr. B was not able to maintain employment because of unreliability in showing up. After trying rehabilitation programs several times, unsuccessfully, his last attempt seemed to stick, following his diagnosis with hepatitis C. Taking an open mind to recovery, Mr. B discovered a new life for himself, and he especially found that working with others gave him a renewed sense of purpose in life. At two years sober, he decided to complete an associate degree program in chemical dependency counseling at his community college. Mr. B loves school and loves working as a chemical dependency counseling intern at his community's correctional treatment facility. He has every intention of going on to complete his Bachelor's degree and perhaps a Master's degree, but he is not sure if he is "smart" enough to handle the writing component of this advanced education. The clients at the facility connect with Mr. B's easy, natural style, partially because it is very clear that he has been to the dark places that they have been.
Ms. T is an African American woman, 50 years of age, who completed her Master's degree in social work two years ago. Ms. T was grandfathered into being a licensed social worker in her state before formal licensure laws came into effect; she worked her way up the ranks in the medical social work department at a hospital near her hometown. Around 40 years of age, she became restless in the "paper pushing" culture of her hospital and decided it was time to make some changes. She thought about going to school for another profession, like nursing, but ultimately decided to complete a Bachelor's degree in social work and stay on for her Master's. She enjoys working with clients in an individual manner, conducting therapy; she feels that she has a great deal to share because of her rich life experience. Ms. T is the mother of three, the grandmother of five, and lost one of her grandchildren in a fatal car accident. Ms. T's father worked with Medgar Evers during the Civil Rights movement, and Ms. T was raised with a strong commitment to social justice. Despite liking her clinical job at a company near her hometown, Ms. T experiences frustrations. For instance, she never thought that there would be as much paperwork in clinical life as there was in medical social work. She finds juggling her schedule, with the mixture of clinical and administrative demands, to be a challenge. She also finds working with some of the younger counselors from a more privileged background to be a struggle, as she sees them as being "out of touch" with what their clients go through. Moreover, Ms. T's clinical supervisor is 18 years younger than her, and Ms. T often has resentment in having to take direction from her.
Mr. N is a self-described "family man," 52 years of age and of Polish Jewish descent. His parents were refugees following the Second World War and immigrated to the United States in the 1940s. Education was highly valued in his family growing up, and Mr. N immediately went to college, finishing a Bachelor's and Master's degree in social work. Mr. N established a career working with Jewish family services in a major American city as a clinical social worker, and he genuinely enjoyed his work. At 45 years of age, Mr. N was compelled to return to college and complete a PhD. His brother is a medical doctor and his sister is a lawyer, and even though he is successful in his own right, he was always made to feel like the underachiever in the family for not living up to his full potential. At the advice of his agency director, Mr. N decided to pursue a PhD in psychology, not in social work, as completing the degree would make him eligible for a psychology license. This new license would make Mr. N eligible to do forensic and educational evaluations that could be quite lucrative in his state; after all, his agency always "contracted out" such services. However, completing a PhD in psychology means that Mr. N would have to complete another internship with a licensed psychologist. He has a friend who is willing to conduct the supervision, monitoring his existing hours at Jewish family services, in addition to mentoring him through other evaluation-based tasks that he must learn. About halfway through the program, Mr. N finds he is growing weary of being supervised again and wishes that he would have chosen to complete a PhD in social work instead.
The idea of "stepping into the shoes" of another to better appreciate his or her perspective is the hallmark of putting empathy in to practice. We are encouraged, as professionals, to do it with clients, and many do it quite well, but it is important to consider this with supervisees as well. Engaging in such a practice is an effective way to build competence as a person-centered supervisor. There are simple ways to practice this art. For instance, take one of the four cases introduced at the beginning of this section. As a supervisor, which case would you be most likely to struggle supervising? Reread that case and then take a moment to reflect and ask yourself, "What is he or she really going through? If I had to put myself in his or her shoes for a day, how would I respond?" Often, supervisors most struggle with supervisees whose shoes they "resist" stepping in to. This simple exercise, inspired by guided imagery, is one of the best ways to practice exploring one's potential for empathy and what blocks exist that keep you from being as effective a person-centered supervisor as possible. In some cases, resistance is more than about dissimilarity to one's own life or fear-based (e.g., fear being in a position in life in which more schooling and more supervision is necessary). However, if one is able to honor and access this sense of trepidation, he or she may be able to connect to what Rothschild and Rand called somatic empathy [22]. Somatic empathy is about noting and honoring physical reactions to a person or a situation, recognizing that this response is likely mirroring what that person is experiencing. A sense of trepidation and visceral uneasiness at the thought of having to be in a supervisee's position gives a supervisor a better understanding of the trepidation and uneasiness he or she is likely experiencing in the work context. So much of empathy is being attuned to visceral, body-level clues. Instead of ignoring them, these responses can be used to better work with others.
Doing brief guided imagery meditations in order to "step into the shoes" of supervisees, as described previously, is one option for developing one's ability to be empathetic and build on existing capacity for empathy and unconditional positive regard that may already exist as a therapist. Even if one is a very empathetic therapist who is capable of putting person-centered principles into action with clients, it is still important to do these exercises to evaluate capacity for practicing these principles with supervisees. Even though the principles are similar, the context differs, which is why it is important to practice building empathetic capacity with supervisees. For instance, all of the administrative and legal/ethical responsibilities associated with supervision may result in a sense of nervousness or pressure to "do it right." In this new context, empathetic capacities can be significantly altered. Thus, doing these "step into their shoes" types of exercises can help to better appreciate the perspective of your supervisee, and it may be worthwhile for you to notice how the context or pressures of "being a supervisor" affect one's supervisory practice.
Constant correction and criticism from a supervisor are generally ineffective. However, if you value the supervisee and welcome his or her newness as something "fresh," as something to be welcomed as opposed to something to be feared, a supportive relationship in which corrective feedback is much more likely to be received will be created. Many have experienced success with this logic in working with clients.
Being corrected can be difficult enough, but being insulted or shamed during the process can be a dehumanizing, discouraging experience. Using the cases that opened this section, think about how being called a "novice counselor" might affect someone like Ms. V or Mr. B. Although they are relatively new to the helping professions, such a phrase, used pejoratively, might break the spirit of someone who is new and doubting his or her skills in the first place. Moreover, the practice of "keeping people in their place" is not kind, from a humanistic perspective, and can do harm to the new supervisee. Promoting a climate of supportive growth, as opposed to enforcing perceived hierarchical differences or reminding supervisees of their newness to the field, is a necessary part of practicing person-centered supervision.
Supervisees often feel that their supervisor holds their future in their hands, whether it be for internships to get a license or while licensed in order to become independently licensed. They may be scared that sharing personal experiences will be used against them later, or they may be reticent to seek additional help, fearing it will damage the relational alliance. Simply appreciating that supervisees may see you this way and making a conscious choice not to exploit that dynamic is putting humanistic empathy into action within the supervisory relationship. Although in cases of unethical or downright inappropriate behavior it may be necessary to use leverage as a supervisor to bring about change in the supervisee's behavior, these uses of leverage should be implemented only in exceptional cases. A supervisee, in regular circumstances, should not be made to fear that you, as the supervisor, can destroy them over a personality conflict or power struggle.
Another potent way to building empathetic capacities, whether for working with clients or supervisees, is to quite literally remember what it was like. Ineffective supervisors may be either so jaded or so caught up in being an "expert" that they forget what it was like to be a developing professional in need of supervision. It is important to call upon our past memories of what it was like to be "supervised," whether it was in a human services capacity or in another job. Even negative experiences will inform your choices as a supervisor, giving insight into what not to do.
Just as there are negatives to learn from, positive experiences can enrich and inspire us. Perhaps in your experiences as a supervisee, you felt supported in your continued growth as an independent counselor. As a result of feeling supported, supervisees actively seek out clinical supervision, even when they are not technically required to receive it regularly. Being supported and empowered, no matter one's age, specialty, or status in life, is the optimal environment for supervision, both clinical and administrative. It is a simple matter of "golden rule" logic: treat others how you would like to be treated.
The skills of stepping into the shoes of another and remembering one's own experiences are two critical ways to build one's ability to be empathetic and to put it into practice in the supervisory relationship. The person-centered principle of meeting people where they are, which is an art often practiced with clients, can also be applied in the supervisory relationship, in addition to embracing simple elements of kindness, like the golden rule. In this section of the course, we will begin to build upon these basics of person-centered logic to develop strategies that work in both supervision and clinical consultation. These are meant to be suggestions only, and supervisors are encouraged to incorporate tools into their own unique practices.
"Imbuing fear" is the notion of being too afraid to do something, and this often happens with people trained in a new approach to therapy, especially with something that can seem complicated, like eye movement desensitization and reprocessing (EMDR) [23]. If trainers and instructors overload people with information, trainees can become afraid, fearing that if they miss one step, they will somehow mess up the whole therapy or do grave harm to a client. Although the desire to "do no harm" is noble, by focusing too much on little details, people can miss the big picture of therapy, such as how fostering a safe, therapeutic context is most likely to promote a healthy environment for therapy.
The same is true in supervision. Supervisees may become overwhelmed if they are bombarded with negative feedback and too many things to work on at once. Letting the supervisee know what is being done right (fostering confidence) and giving him or her no more than two or three things to work on at a time will result in the best outcomes. This can be accomplished in many ways, but one useful tool is what is referred to as the "compliment sandwich." In the "compliment sandwich," share with supervisees something that they are doing right, then insert an area of improvement, and then end with a compliment. While this approach may seem too soft to some, especially those of a more militaristic or direct temperament, it can be successful.
Often, people are so used to getting criticized that being praised and empowered in a genuine way becomes an effective supervisory technique. Shaming and criticism can make people defensive, especially if it causes them to doubt their own abilities or competencies. Recognizing this dynamic is part of what fostering confidence is all about. Working with new counselors who are very raw and seem to need a great deal of work can make the art of fostering confidence difficult, but it can be done. Even starting with a singular strength and building upon it will get farther than focusing only on all of the areas that need improvement. When working with supervisees, make it a point to tell them what they are doing that is positive and beneficial to those that they serve. A simple "You can do it!" can go a long way.
Trouble can arise if a supervisor focuses on the specifics of a technique and imbues fear by focusing on everything that can go wrong and being militant about following the letter of the law. By not focusing so much on the technique and what can go wrong, people are in a better place to learn, and this is a person-centered idea. As clinicians, we stress the importance of helping clients find their senses of self-efficacy and empowerment, so why would we not impart this same attitude of discovery and exploration with supervisees? Of course, correction may also be necessary. Remember the parallel of the dance: they are leading, you are following, but you have the right at any time to say "halt" if something seems amiss. Staying with the dance analogy, should a good partner criticize you and constantly make suggestions, or cheer you on for the good job that you are doing?
Let's apply this idea to the case of Ms. V, the young counselor who feels overwhelmed as an intern with agency work. How would she feel if, after criticizing herself already due to frustrating interactions with clients, her supervisor simply harped on her for everything that she was doing wrong? Part of a supervisor's job may entail evaluating areas of further training Ms. V should pursue, or perhaps it may require suggesting that Ms. V seek out some of her own therapy in order to work through her blocking issues. However, think of how much more smoothly broaching these issues will be if Ms. V knows her supervisor cares about her as a person. Here is an example of how a person-centered supervisory interaction could play out:
Supervisor: V, I got your email about the session you had with L (client in question) and that it took a toll on you. How can I best help you with this?
Ms. V: I don't know. I just feel in over my head.
Supervisor: Okay…Can you help me understand a little bit more about what you mean by "over your head"?
Ms. V: I mean, I have thought about it…I've really been thinking about it for the last several days, and I think he's right. I mean, what do I really know about real life? I'm just a privileged little white girl who has a degree.
Supervisor: Wow, that's heavy…Is that what L said?
Ms. V: More or less.
Supervisor: And you've been thinking about this for the last several days since it happened?
Ms. V: That's all I've been able to think about.
Supervisor: Wow, that's heavy stuff, V. I'm sorry that you've been beating yourself up about this issue. I just want to assure you that you are not alone here. We have all been told off or talked down to by clients at one point or another during our careers.
Ms. V: Really?
Supervisor: Absolutely.
Ms. V: It just seems to come so easy for so many people.
Supervisor: I hear that it can seem that way. You may have heard that cliché before that everyone who's an expert at something was once a beginner. That applies here, too, V.
Ms. V: I just feel like I'm not cut out for this.
Supervisor: Can you tell me more about that?
Ms. V: Well, yeah. I mean, the people that we're dealing with here in the city. I've just never had to deal with this kind of pain before. I can't even imagine what it's like to be on welfare, or to have parents that ran off on you, or to be addicted to drugs. I want to help people, but I just don't know what to say.
Supervisor: I hear that. What seemed to bother you the most about what L said to you?
Ms. V: I don't think it was what he said as much as how he said it. Just that he towered over me and I felt paralyzed to say or do anything. I get that I can never really understand what's going on in his life, but he was so harsh about it.
Supervisor: Interesting. There are a couple of ways we can approach this. We can look at what about this interaction with L triggered things for you. Or we might re-examine what you remember saying in the conversation that seemed to set L off. You tell me, V, where do you need to go with this?
In many cases supervisors face a choice of going by the book, or following their intuition. Some people are "by the book" and more interested in following the letter of the law, and others have more of a free-spirited, intuitive, experiential orientation. Some want to see an empirical research study to inform every intervention, while others are content with the feedback that they receive from clients or others. Others approach decision making in the human services with a combination of these approaches: the letter and the spirit, the logic and the intuition, the research and the experience. All vantage points can be helpful in the human services professions, and this applies to supervision as well.
Of course, all supervisees are different, so the approaches used with them must differ in order to be truly person-centered and meet people where they are. Although some may request technical instruction and specific feedback, many supervisees are looking for an experience richer than the technical elements that they can read in a text. Textbooks are full of information about what to do in theory, but guidance from an experienced supervisor gives a better understanding of the art of counseling and how to handle tricky scenarios that clinical life entails.
As a supervisor, it is important to give your supervisees options. An experienced clinician can respond to supervisees' questions regarding complex scenarios by presenting what the textbook says to do and what he or she would actually do (if they differ), providing information on both perspectives on the matter. Offering choice is the very essence of empowerment.
Some experts argue that the field, as a whole, would be enriched if practitioners candidly shared what they actually do, as opposed to what the standards state [23]. Offering supervisees choices on how to handle a situation, just like the supervisor gave Ms. V a choice on where she wanted to go with her supervisory session following the difficult encounter with a client, is paramount, especially if a person-centered approach to supervision is desired. Here's an example of how this choice dynamic may play out with a different supervisee, Mr. B:
Supervisor: So, what would you like to work on today?
Mr. B: Well, I'm struggling. When I was in treatment all of those times that didn't work, I used to get pretty nasty with counselors when they brought up the idea of going to AA or NA meetings. Then, I got clean in a 12-step program and it all clicked, as you know from my story. So now when I talk with clients about meetings or using 12-step language, they're getting smart with me the same way that I used to get with counselors. And it's frustrating me like crazy. I just want to shake them sometimes and tell them that they're going to keep failing until they get into a program.
Supervisor: I see. Well, I can relate to some extent. It can be a struggle when you feel that, as a person, you worked hard and something really clicked for you, and you just don't see why others won't get it too.
Mr. B: Yeah, that's a big part of what's going on. I didn't think it would bother me so much.
Supervisor: What do you think you need to do to address it?
Mr. B: I mean, meetings are the only way for a person to get clean. How can I make them see that?
Supervisor: Well, let me share this with you. Technically, if we look at what the studies in the field say about getting sober, we know that meetings aren't the only way to get and stay clean, although they are certainly one of the most popular and effective ways. Again, that's what the field as a whole teaches, so we need to respect that. But what this treatment center has learned through experience and feedback is that meetings seem to work the best for the most people who come through our doors…if they want to stay sober long-term.
Mr. B: I don't know if I buy that. About what "the field" says.
Supervisor: I'm not saying you have to buy it, B. I'm just sharing the information with you. What you do with it is up to you. I'm just asking you to keep an open mind to it and think about how sharing both sides with a client, like I just shared with you, might be helpful.
Outcomes, or clear data/evidence to show whether or not (or to what extent) a certain intervention is effective, are an important component of evaluation in the psychotherapeutic professions. Certain agencies and accrediting bodies place more value on outcomes data than others. Regardless of what one's opinion about tracking formal outcomes, consider that reviewing a treatment plan to see if something is working to help a client reach his or her goals is a way of measuring and evaluating outcomes. Clinicians must be able to demonstrate which interventions work, not only to the entities (like third-party payers) who are supporting treatment, but to clients so that they stay engaged. Some clinicians are advocates of tracking outcomes on an agency-by-agency and case-by-case level to most effectively determine whether or not an approach is working [19]. However, the thought of asking a client "How am I doing?" scares many clinicians, because they fear they might not be able to handle what the client shares. Although it can be frightening, consider how setting an honest culture of feedback within the therapeutic context can foster a more interactive therapeutic alliance. Setting the culture of feedback consists of assuring the supervisee that he or she will not be punished for sharing honest reactions and following through with this commitment.
The same commitment to setting a culture of feedback can be practiced within the supervisory relationship as well. Because of the precarious power dynamic that may exist between supervisee and supervisor, following through on this commitment to non-retaliation becomes imperative to achieving and maintaining this healthy feedback culture. A supervisor can simply obtain feedback by asking at the end of each session or every few sessions. Some examples include, "How useful was the session for you today?" or "Is there anything I could have done differently today that might help better next time?" The fact that a supervisor asks these questions can help to forge the professional relationship.
Supervisors can also elicit this feedback within a session, on a micro level. When sharing a suggestion or offering guidance to a supervisee, ask if the suggestion feels right or is helpful. If a culture of feedback has been promoted within a solid relational alliance, this feedback will be reliable. Consider how a dialogue in this approach might play out between Ms. T, another case outlined previously, and her supervisor:
Ms. T: I find that J (a client on Ms. T's case load) is frustrating me more and more. I don't know if she's just rubbing me the wrong way or if I'm doing something wrong.
Supervisor: What seems to be the source of the frustration?
Ms. T: Well, she comes into session, always with a catastrophe, just chattering and chattering away and I can't get a word in edgewise.
Supervisor: Hmm…Did you ever deal with these chatty types when you were working at the hospital?
Ms. T: Sure, but it never seemed to be this bad. And I never have this sense, like I had with J, that she's expecting me to fix things for her. And I mean, how can I fix things for her? She won't let me suggest anything.
Supervisor: Well, that is a very good point. Just to look at it though, did you ever do anything with your clients at the hospital that seemed to get them on track?
Ms. T: Well, it's little, but I usually found that the "take a deep breath" line would work, even if I was interrupting them to suggest they take a breath.
Supervisor: I think that you're on to something, T. In my work, I really praise the benefit that breath and using the body can have with clients. So let me share with you something I've tried before with clients like J.
Ms. T: Okay.
Supervisor: Clearly, there is some type of relationship established because J keeps coming back for sessions and seems to trust you. So, the next time that she comes in, after you get the initial hellos out of the way, be assertive. Ask if she is willing to try something different to start this session. Ask her if she would be willing to just do some breathing for the first 5 minutes of the session, before you do any talking.
Ms. T: Interesting. You think that would work?
Supervisor: I've tried it before with some success with those chatty types of clients or those who want to analyze everything.
Ms. T: What if she resists?
Supervisor: That's definitely a possibility. Whenever a client puts up a protest, a common line that I use is, "Would you be willing to try it? It's something different than what we've been doing and I have a feeling it may work better for you." Make her realize that you are interested in trying every possible option to help her.
Ms. T: That's a good point. I never thought of it that way.
Supervisor: How is this suggestion we just discussed resting for you?
Ms. T: I like it. It feels good, and it's certainly worth a try.
At one time or another, you have likely asked a client, "What is this really about?" For instance, a client may be having an intense reaction to what seems to be a petty stressor, but it becomes clear after observing some deep, visceral level distress that something else is going on. Perhaps that "petty" work stressor is a reminder of a stressful dynamic with an abusive parent. Within the context of a working, therapeutic alliance, asking a client to examine the underlying cause of distress can be a powerful intervention, and it can be in clinical supervision as well. However, one should not use this strategy with a supervisee who is new or with whom you have not formed a working relational alliance yet. This question can backfire if the supervisee ends up resenting it. But, if the alliance is established, this simply placed question can open up a world of new discovery. Let's revisit the supervisee case of Ms. V and the dialogue explored in an earlier session about her struggles with her client, L, and see how the approach of asking what the distress is really about may work with her. Remember that the conversation left off with the supervisor giving Ms. V an option about what she most needed to address:
Ms. V: I don't think it was what he said as much as how he said it. Just that he towered over me and I felt paralyzed to say or do anything. I get that I can never really understand what's going on in his life, but he was so harsh about it.
Supervisor: Interesting. There are a couple of ways we can approach this. We can look at what about this interaction with L triggered things for you. Or we might re-examine what you remember saying in the conversation that seemed to set L off. You tell me, V, where do you need to go with this?
Ms. V: I'm not sure.
Supervisor: Well, just take a minute then. You can close your eyes and get silent if you need. Ask yourself where you most need to go today.
Ms. V: Okay. (She briefly pauses) It's the way he just got up and stood over me. I felt very unsafe.
Supervisor: Okay, V. That's very honest. If I can ask, being towered over like that and not feeling safe, what is that really about?
Ms. V: Wow, I didn't think of that parallel. Whenever my parents doubted my opinion on something, especially about my career choice and field of study in college…whenever I fought them on anything, they would stand up, even if we were at the dinner table. It's like it was their way of making me feel small. Even if we were all standing during an argument, it would seem like they became 10-foot-tall giants when they started to argue.
Supervisor: How interesting. Is there a chance that your interaction with L triggered this dynamic with you?
Ms. V: Oh, absolutely. And I think it hit me even harder because my parents never really wanted me to go into this field in the first place, even though they financially supported my education. It's like L telling me I don't know what I'm doing is hitting me even harder because that sounds like something they would say.
Supervisor: That's really fascinating, V. Is this something you're comfortable continuing to talk about with me or do you feel you may want to address it with someone else?
As a point of clarification, a supervisor, even a person-centered one, should never become the supervisee's therapist; obvious complications can arise with a dual relationship. However, it is inevitable that a supervisor will explore some issues of emotional significance with a supervisee, especially if these issues are triggered by on-the-job issues or if these issues impact one's ability to do the job. If it is clear that using the "what's this about" or other exploratory approaches opens up more than the supervisory relationship is designed to contain, it then becomes the supervisor's responsibility to explore the supervisee's potential need for clinical services of his or her own. That exploration is what the last line of this dialogue leads to. This idea will be explored further later in this course.
A rupture is a break or a disturbance that causes impairment in flow or function. Ruptures can occur in every kind of relational alliance, whether it is a personal relationship, a romantic relationship, a therapeutic relationship, or a supervisory relationship [24]. A rupture occurs when something goes wrong, for whatever reason, in a relationship. Unless it's addressed in some manner, it can permanently alter the relationship and have an impact on its success or failure. Even if the original rupture is significant, if it is addressed effectively, it can positively impact the relationship overall.
Ruptures can happen in supervisory relationships for a variety of reasons. What is most important for supervisors to accept is that if they played a role in causing the rupture by offending or otherwise causing friction with a supervisee, they take responsibility and address it immediately. Just like the "golden rule" logic can go a long way, so too does the simple act of admitting when one is wrong. Many supervisors or managers are reticent to do this, feeling that it will make them look weak or that admitting fault can undermine authority. However, nothing creates more respect for those in power than when they can admit that they are wrong and correct a mistake.
Part of a supervisor's responsibility is being able to recognize what his or her part is in a situation and what part the supervisee may play. Of course, supervisors are not always in the wrong in the case of the breach and it is not totally their job to fix the rupture. However, it is their responsibility, if they know that a rupture exists, to bring it to light and attempt to elicit a repair with the supervisee, even if he or she is are clearly in the wrong. Consider how this dynamic might play out for the supervisor working with Mr. N, the PhD psychology student/social worker introduced earlier:
Supervisor: N, I need to ask how you feel things are going with our supervision sessions.
Mr. N: Oh, fine.
Supervisor: Fine?
Mr. N: Yup, no complaints. You're doing a good job, if that's what you want to know.
Supervisor: Thanks, N. Bringing this up with you is a bit tricky, because we've had a collegial relationship, and I'd like to think friendship, for many years now.
Mr. N: Uh, oh. I feel a lecture. What's the problem?
Supervisor: Now, don't jump to conclusions. There's just something I feel I need to address. According to the terms of our supervisory agreement for your psychology license, I need to meet with you in person at least once a week for our session. I've noticed that you've been showing up at least 15 minutes late to almost all of our sessions, and you're skipping a few of our meetings, which doesn't seem to be like you at all.
Mr. N: It's no big deal. I'm just really busy juggling my work at family services, my course work, coming here, and doing some of the new evaluation tasks I'm being asked to complete. I thought you understood this.
Supervisor: I'm sensitive to the position you're in. I'm just starting to feel like the time I'm setting aside doesn't matter to you or that these sessions are more of a chore for you than anything.
Mr. N: Well, to be perfectly honest with you, they kind of are. It's one more thing I have to do.
Supervisor: I can appreciate that. Is there any part of you that is resenting being supervised?
Mr. N: Well, it's kind of tricky, yes. I know there are some different tasks as a psychologist that I have to learn, but in essence, I'm just doing the same thing I've always done as an independent social worker.
Supervisor: I understand. But I would be dishonest with you if I kept pretending that everything was okay here. Above all, I want to make sure that you're alright and to see if there's anything I can reasonably do here to make this situation more beneficial for you.
Mr. N: Is it okay if I think about that and get back to you?
Supervisor: Absolutely. If I were in your situation and needed to go through supervision all over again to get a new license, I would probably be a little salty, too, so know that I can relate. I just hope we can figure out a way to move forward that works for both of us.
The psychotherapeutic professions are greatly focused on models. Models are used to explain how a certain phenomenon is supposed to unfold or how a certain aspect of behavior should be reshaped. Although models or technical explanations can be useful, the tendency to obsess over fully grasping a model or trying to fit clients and supervisees to specific models is not. Models and theories tend to develop independently of each other over time to explain a particular phenomenon that professionals seek to understand. Skinner once stated that assigning a level to an individual "does violence to the nature of the development process" [25]. This is true; development is a multidimensional process. Appreciating the developing clinician in such a way is optimal in the person-centered approach to clinical supervision.
In supervising clinicians, navigating developmental appropriateness becomes an even more complex task. Consider the four cases introduced earlier in this course. According to traditional, Ericksonian development, Ms. V is at a different stage of development than the other three, and one could argue that Ms. T and Mr. N are perhaps transitioning between two developmental stages at these points in their careers. Consider how approaching Ms. V about issues might be different than how you would approach Mr. N, for instance. To revisit the common sense logic that resonates throughout this course, person-centered supervision is all about appreciating where a person is coming from and meeting that person where he or she is.
In this section, some accepted stages of counselor development used by the helping professions will be examined in order to have some type of guide, although these stages should be taken as a guide only, not an absolute teaching. In the spirit of flexibility, an alternate construct to conventional development models, stages of changes theory, and motivational enhancement will also be provided. These same approaches for motivational enhancement used with clients can be as valuable in working with supervisees, regardless of where they are on any developmental spectrum.
The purpose of this section is not to explain developmental models in general, like those of Erickson or Loevinger. However, if existing knowledge of these models helps one's work with supervisees, they can certainly be used. Some of the popularly accepted models of counselor development that exist in the various human services professions include [26,27,28,29,30]:
Counselor dependent upon the supervisor
Autonomy-dependence conflicts with the supervisor
Higher level of counselor self-confidence/autonomy in action
Counselor acts with a high level of personal autonomy, which includes awareness of a continuing need for personal and professional development
Inception (e.g., insecurity, dependency, inadequacy)
Skill development (i.e., move from dependency to autonomy/adequacy)
Consolidation (e.g., self-confidence, individuation)
Mutuality (e.g., creativity, independent practice)
Nondirective expert guidance
Adoption of client/content-centered approach
Relationship-centered approach
Therapist-centered supervision
Preconformist stage: One-on-one supervision needed
Conformist stage: Group supervision and continuous feedback needed
Self-awareness/post-conformist stage: Supervisor becomes a colleague and peer
These models are a sampling of available proposed models to explain counselor development. A common theme in all of these models is perhaps captured in a statement from Hogan's work: "The overall aim of supervision is to foster growth toward independence, moving the clinical trainee from student, to colleague, to expert" [25]. Supervisors are essentially guiding a new professional's growth through a process. Person-centered supervision acknowledges that each clinical professional's process, although one of growth, is unique to that person.
The approach of motivational interviewing can be incorporated into supervisory practice much as it is used in psychotherapy. As the name of this approach suggests, motivational interviewing is about asking a series of questions to enhance an individual's overall drive toward change, a shift from confrontational or directive approaches to counseling [31]. Motivational interviewing assumes that all people have within them the abilities and the skills they need to change. Mental health professionals can help people realize this potential so they can manifest change for themselves. Motivational interviewing, as a strategic approach, works well alongside many theories and techniques in counseling. It is ultimately very effective because the conclusions that one draws from oneself that lead to change are more likely to persist in the long-term than changes that feel forced by outside entities. Because motivational interviewing steers away from specific direction or confrontation, it is person-centered in its aims. The substance abuse field increasingly regards motivational interviewing as the best approach to working with resistant clients. Consider how using an approach that works with clients may also apply to work with supervisees, especially supervisees who may be resistant to supervision.
Many professionals resent being supervised, and these resentments can take on a variety of shapes. The time commitment is often a first barrier for busy professionals. Older professionals like Ms. T and Mr. N who have been working in human services in some capacity for many years but are moving into a new area of service within the professions are likely to feel some level of resentment. This resentment can be more significant if they are being supervised by younger professionals, contingent, of course, upon personal variables. Professionals like Mr. B may be more likely to experience this resentment or be resistant if they feel they know more about "real recovery," obtained through life experiences, compared to a supervisor who has learned only through formal training. Super students like Ms. V may be prone to entering an internship or work site feeling that she knows it all and could be sensitive to correction. Inferiority fears, which may be present in all four cases for a variety of reasons, can also be a major reason for resisting supervision and the corrective feedback that comes with it.
Consider the three major principles of motivational interviewing described by Miller and Rollnick [31]:
Collaboration: Counseling involves a partnership that honors the client's expertise and perspectives. The counselor provides an atmosphere that is conductive rather than coercive to change.
Evocation: The resources and motivation for change are presumed to reside within the client. Intrinsic motivation for change is enhanced by drawing on the client's own perceptions, goals, and values.
Autonomy: The counselor affirms the client's right and capacity for self-direction and facilitates informed choice.
This is another example in which the word "counseling" can be replaced with the word "supervision," the word "counselor" can be replaced with the word "supervisor," and the word "client" can be replaced with the word "supervisee."
Perhaps these principles make sense in terms of working with a supervisee, but the next step is putting them into action in the supervisory relationship in working with resistant supervisees. Miller and Rollnick suggest for resistant clients [31]:
Express empathy.
Develop discrepancy.
Roll with resistance.
Support self-efficacy.
Clearly, empathy is of massive importance, and much of this course has been devoted to discussing it. If empathy is present on the part of the supervisor, all of the other skills can flow much more successfully. Developing discrepancy is an alternate, more positive way to look at confrontation. Instead of directly confronting a behavior that should be changed, point out a discrepancy and allow the supervisee to arrive at his or her own conclusion. Consider how Ms. V's supervisor might implement this skill:
Supervisor: V, help me understand. On one hand, you believe L when he accused you of knowing nothing about real life, yet on the other hand you share that you know what it's like to be towered over and looked down upon by your parents. Isn't that real life?
Rolling with resistance is perhaps the most well-known component of motivational interviewing. It is commensurate to the age-old parenting advice of choose your battles. Supervisors are likely to create a defensive climate if they confront every resistance that a supervisee presents or if they inundate a supervisee with an excessive amount of negative feedback. By accepting that initial resistance is part of the change process, supervisors can take the first successful step in working with a resistant supervisee.
Supporting self-efficacy is a strengths-based concept. This skill can be put into place by taking the positive coaching approach to supervision described previously.
The ethical duties of supervisors are somewhat more complex than those of other practitioners. In this role, there must be a coexisting consideration for the welfare of both supervisees and clients [32]. Among the many relevant issues, five are central to supervisor ethics: competency, confidentiality, informed consent, dual relationships, and duty to warn.
Various professional organizations' ethical codes contain information regarding supervisory function and will be cited and/or discussed in the following sections. Although an organization's ethical code only specifically governs the practice of their members, the ethical principles in each are a good reference for all supervisors (Appendix).
Competency is the ethical duty to practice in one's areas of knowledge and abilities. This consists of limiting practice to professional competencies (including multicultural competency) and improving personal knowledge when a deficit is recognized in order to better assist clients and supervisees. The competencies of supervisees must also be known and managed effectively. The National Board of Certified Counselors (NBCC) Code of Ethics states that those "who provide clinical supervision services shall intervene in situations where supervisees are impaired or incompetent and thus place client(s) at risk" [10].
A large part of supervisory function is to monitor client welfare and supervisee clinical performance and professional development [11]. This can be accomplished by meeting regularly with supervisees to review case notes and clinical work or through live observations. Feedback should be given to supervisees on scheduled dates and at appropriate occasions throughout the year [10].
Competency and confidentiality are arguably the two most important ethical principles pertaining to the helping professions. They are also the cornerstone of the Hippocratic Oath, from which all modern ethical codes trace their lineage. The following is translated from the Oath: "Whatever I see or hear in the lives of my patients, whether in connection with my professional practice or not, which ought not to be spoken of outside, I will keep secret, as considering all such things to be private" [33].
Although they are somewhat different concepts, confidentiality and the right to privacy are closely related. The supervisor/supervisee relationship is unique in that confidential information is shared between practitioners. To respect a client's right to privacy and to maintain confidentiality, it is recommended that only the most pertinent case information (as deemed necessary for the purposes of supervision and/or consultation) be exchanged between professionals [10,32]. For example, only a client's first name should be shared and other identifying information should remain undisclosed (e.g., demographics). The NBCC Code of Ethics states that practitioners "shall respect client's privacy and shall solicit only information that contributes to the identified counseling goals" [10]. Remember that this also applies to supervisors.
Supervisors have the responsibility of ensuring that clients are informed about all aspects of therapy/interventions, including the appropriateness of services, what to expect during and from the services, the limitations of confidentiality, and supervision procedures. Supervisors also have the responsibility of informing supervisees about: the supervision process, including the potential for dual relationships, limitations of confidentiality, and performance standards and reviews; procedures for responding to emergencies and absences; legal and ethical standards related to the profession; how to express concerns regarding the supervision process; and due process appeals of supervisory actions or decisions [10,11,32].
The development of nonsexual/nontherapeutic dual relationships in clinical or educational settings is often inevitable [32]. Shared professional experiences naturally draw some individuals closer. However, even a nonsexual relationship contains a power imbalance that can lead to preferential treatment or exploitation of a supervisee or supervisor. Of course, dual relationships with a sexual component (e.g., sexual attraction, consensual sexual, intimate romantic) also include a power imbalance and generally have a greater likelihood of producing harm and negative outcomes than good or even acceptable outcomes [32]. Supervisors must be aware of this power imbalance.
Professional ethical codes explicitly forbid romantic or sexual relationships between a supervisor/supervisee. For example, the NBCC Code of Ethics states that certified counselors "who act as counselor educators, field placement or clinical supervisors shall not engage in sexual or romantic intimacy with current students or supervisees. They shall not engage in any form of sexual or romantic intimacy with former students or supervisees for two years from the date of last supervision contact" [10]. Similarly, the National Association of Social Workers (NASW) Code of Ethics states that "social workers who function as supervisors or educators should not engage in sexual activities or contact (including verbal, written, electronic, or physical contact) with supervisees, students, trainees, or other colleagues over whom they exercise professional authority" [34]. The American Counseling Association (ACA) Code of Ethics also prohibits sexual or romantic interactions and relationships [11].
The ACA Code discusses the existence of nonsexual dual relationships as being potentially beneficial to both parties, but also suggests remaining aware of the power imbalance [11]:
Counseling supervisors clearly define and maintain ethical professional, personal, and social relationships with their supervisees. Supervisors consider the risks and benefits of extending current supervisory relationships in any form beyond conventional parameters. In extending these boundaries, supervisors take appropriate professional precautions to ensure that judgment is not impaired and that no harm occurs.
As discussed, it is also important to avoid taking on the role of a supervisee's counselor or therapist. Referrals may be helpful in these cases.
A practitioner has the duty to prevent harm to both clients and to other members of society; this can conflict with the ethical principle of confidentiality. The NBCC Code of Ethics sums up the duty very concisely: "[Certified counselors], recognizing the potential for harm, shall not share information that is obtained through the counseling process without specific written consent by the client or legal guardian except to prevent clear, imminent danger to the client or others or when required to do so by a court order" [10]. The "danger" may include threats of suicide, violence, or others, such as disclosure of a communicable, life-threatening disease that the client may spread either with or without intent to harm [11].
An ethical decision must be made whether to breach confidentiality when an expression of intent to commit harm to an individual or their property has been made by a client, in which case a supervisor may be consulted regarding the validity of an expressed threat. Supervisors have the duty to inform and remind supervisees of their ethical and legal obligations to warn potential victims [32]. Supervisors are also legally liable if they have knowledge of imminent, foreseeable danger and they do not make a reasonable attempt to warn potential victims or confirm that a warning has been made by the supervisee.
Seeking to embrace person-centered concepts in one's work as a supervisor is a good first step to carrying out ethical supervision. So much of ethics is about embracing common sense principles and knowing when and how to collaborate with others. There are two issues that are often mentioned in discussions of the ethics of supervision that are worth addressing here, especially to consider how empathetic, common sense principles may help when navigating an ethical conundrum.
In clinical life, supervisors are usually asked to fulfill two roles: that of administrative supervisor, concerned with managerial issues of the agency, and that of clinical supervisor, concerned with issues of clinical growth and formation. A supervisee may show great promise as a clinician, but the same supervisee may be abysmal at administrative tasks like paperwork and time management. How does one resolve the conflicts of acting in both capacities for this supervisee?
One possible option is to divide the supervisory sessions to allow time for each facet, setting clear boundaries and expectations. For example, the first 30 to 45 minutes of the session could be devoted to clinical case discussion and clinical development/formation issues. The rest of the session can then be used to address administrative matters like productivity, meetings, or paperwork concerns. By creating this clear separation, you can promote the idea that what is said during the clinical portion of the session will not be used against a supervisee administratively. Commitment to keeping issues as separate as possible so supervisees do not feel like any sensitive issues they disclose in their case discussions will be used against them is also paramount.
Another dual relationship issue that may manifest, causing ethical dilemmas, is if a friend serves as a supervisor or if a supervisee becomes too close of a friend. Consider Mr. N's case, introduced earlier. Out of convenience, he asked a friend to supervise him, and this ended up potentially causing problems in the relational alliance. Unless the circumstances are truly unique, this is an arrangement that is probably best avoided; too many dual relationship issues may become apparent.
Supervisors often become friendly with supervisees, and forging a friendly connection is a normal part of the human experience. However, it is advised that supervisors reserve forging a friendship outside of the confines of a work setting until the formal period of clinical supervision ends. If one remains an administrative supervisor to a person who is considered as a friend, seek consultation if necessary about how to negotiate dual relationship issues.
As the wording suggests, self-care simply involves taking care of oneself. However, in the helping professionals, self-care carries a more potent meaning. Because those in these professions spend so much time and energy taking care of other people, it is imperative that they make time and energy to take care of themselves. The psychotherapeutic professions are placing increasing importance on the role of therapist self-care to shield against burnout and vicarious traumatization, which improves one's ability to better serve clients. Honoring self-care is an ethical imperative for therapists to embrace [35,36]. This idea makes a great deal of sense; healthier people make healthier, more effective therapists, which will have a positive effect on the people they are entrusted to serve. Thus, it becomes important to discuss self-care as a supervision issue, especially if a supervisor identifies that a supervisee's lack of self-care seems to be impacting his or her job performance.
An extensive study from the field of nursing suggests that effective clinical supervision has a positive impact on assuaging reported levels of burnout in supervisees [37]. This finding would make equal sense if the same phenomenon was investigated in the helping professions. If one-on-one, or even group, supervision time exists as a forum in which to vent emotional or technical frustrations connected to the job, it is clear that quality supervision time can be part of a supervisee's self-care regimen. The imperative, as discussed in previous sessions, is that the supervisee feels safe to engage in such a catharsis without fear of administrative retribution.
Simply having the opportunity to sit down with someone more experienced who is in a solid position to share experience, strength, hope, and perspective can be very helpful to supervisees, resulting in clinicians who are better prepared for their jobs. Supervisors and mentors, within the context of a solid, relational alliance, can make small yet powerful suggestions on how a supervisee can better take care of his or her self. One such suggestion is to prioritize self-care time, and some have recommended that self-care be allotted at least three hours per week. Although seemingly a paradox, the more time we allot to take care of ourselves, the more time we will inevitably have to complete necessary tasks. In addition, taking time for self-care will allow one to be more mentally present and thus more efficient.
The concept of self-care can be explored in each of the supervisory cases discussed previously. Assuming that a solid, relational alliance is in place, these cases will explore ways that a supervisor can make suggestions to a supervisee on improving self-care measures.
There are many ways to introduce self-care strategies to a supervisee in a manner that does not cross into the realm of therapy. Appreciating the context of their situation and their life is absolutely vital. If supervisees are resistant, it may help to bring up that self-care for the helper is ultimately a quality-of-service issue and an ethical imperative [36].
Supervisor: I can see that this whole situation with L has brought up a lot of things for you. What do you feel you need to do to best take care of yourself in the wake of all of this?
Ms. V: I don't know…Drop out of the counseling program? (Laughs)
Supervisor: Take a moment and ask yourself if that's what you really want.
Ms. V: Of course not. I still really want to be a counselor.
Supervisor: Okay, if I may be so bold, let me ask you this. When's the last time you went through your own counseling?
Ms. V: Well, I saw one of the campus counseling center professionals when I was an undergraduate, but since then, nothing.
Supervisor: Would you consider perhaps getting some counseling for yourself again, especially since we've concluded that this situation with L triggered a lot of personal stuff for you?
Ms. V: Am I allowed?
Supervisor: Well, you couldn't do it here, but I have a list of some providers. I can refer you to people that I trust to work with other professionals. Rest assured, V, if you are going to work in this field, there is no shame in getting your own therapy. A mentor of mine told me once that to be a good therapist, you ought to have a good therapist!
Ms. V: That makes me feel better. And you're right; it's probably a good idea.
Mr. B: I'm not going to lie—it's been a rough week for me.
Supervisor: Yeah, the patients seem to be getting you down.
Mr. B: For sure.
Supervisor: If I can ask, how are you doing with getting to your own meetings?
Mr. B: (Laughs) What, are you trying to bust me?
Supervisor: No, B, and I'm certainly not trying to play your sponsor. I just know that in working with professionals in the field who are also in recovery, it becomes so important for you to keep working your own program, maybe even amping it up a bit. This is a stressful field, as you are learning.
Mr. B: Well, before I started school, I was routinely doing four to five meetings a week. My sponsor told me I should never slip below three, and I've been pretty good with that overall. But since I've started working here, there are weeks where it seems to go down to two plus a phone call to my sponsor.
Supervisor: B, recovery is not something you can get by osmosis, which I hope you are learning. It's a great idea to think that by working around recovery so much we will pick some of it up for ourselves, and we can. But I have seen countless people burnout or even relapse when they replace working their own program with working in the field.
Mr. B: Those are good points.
Supervisor: Are you willing to talk to your sponsor about the matter further?
Mr. B: Absolutely.
Ms. T: It's been a rough week. There must be a full moon out or something!
Supervisor: I hear you, T. It's been stressful for me, too. Anything I can do to help?
Ms. T: I don't think so. It's just been that every client on my case load this week seems to be in crisis and I'm behind on paperwork. And to make matters worse, my husband is sick, my dog is sick, the grandkids are coming to visit next week, and the church benefit auction that I'm on the committee for is happening the week after.
Supervisor: Wow, I'd say that's a lot on your plate.
Ms. T: Yeah.
Supervisor: T, if I can be frank…when's the last time you've done something nice for yourself?
Ms. T: (Laughs) Oh, you would have to play shrink and ask me that.
Supervisor: T, I'm not asking you to do therapy with me. I just get concerned sometimes that you are so many things to so many people. I would hate to see you burn out.
Ms. T: Well, point taken.
Supervisor: Let me put it to you this way: If one of your clients came in and told you how stressed they were, if one of your clients told you what you just told me, how would respond to the client?
Ms. T: I'd tell them to go get a massage or something! Or at least spend some time each night chilling out and taking a bath.
Supervisor: Both excellent ideas. Have you done that lately?
Ms. T: No.
Supervisor: Would you consider it?
Ms. T: (Laughs) Well, you got me there, and you're probably right. I'll make it a point to get in the tub tonight after work.
Supervisor: N, I know that we've talked about some difficult matters with our professional and personal relationship here. Is there anything else I can do to help?
Mr. N: You can tell the state board to cut back on the hours for supervision requirements.
Supervisor: I know that's an issue for you; I hear that clearly. But I also know that you are one of the best social workers in this area, and you work with clients who are in situations like this all the time—having to tough something out that they don't really want to do.
Mr. N: So, what are you saying?
Supervisor: I'm just putting this out there. What would you tell a client who was on parole or probation who didn't want to put in the necessary requirements?
Mr. N: I would work with them on practicing acceptance.
Supervisor: Yup, that's what I was getting at. And do you have a favorite strategy that you like to use for practicing acceptance?
Mr. N: Well, prayer and meditation. (Laughs) Okay, I see what you're getting at here.
The National Institute for Occupational Safety and Health summarizes the essentials of a self-care plan as [38]:
Balance between work and family or personal life
A support network of friends and coworkers
A relaxed and positive outlook
This is a basic framework that can be shared with supervisees, consultees, and trainees if they are feeling stuck on how to make commitments to self-care. When seeing these three components of the framework, people can usually identify which area needs the most work. Using the case scenarios from the previous section, it seems that Ms. V most needs support, so the second area would be a place for emphasis. Mr. B may have deficits in all three, but because of his commitment to 12-step recovery, his supervisor suggests that he amplify the second area as well. For Ms. T, the first area is the main focus, and for Mr. N, it was area three.
In most cases, formal self-care plans are not necessary. Typically, self-care discussions can be integrated into our supervisory sessions. However, if a supervisee continues to struggle with implementing the basics of self-care with this more casual approach, working together on a formal plan, even putting it into the language of a contract, may be warranted (Figure 1).
Putting the plan down on paper and having both the supervisee and the supervisor sign it can add that heightened degree of accountability. And if a person has an accountability partner for self-care plans, he or she is much more likely to follow through with them. Active clinical supervisors should consider accessing the National Institute for Occupational Safety and Health's online manual Stress at Work for more ideas on how to create an environment at the work place that supports self-care [38]. The ideas in this guide are especially relevant for those in the dual role of being a clinical and administrative supervisor. This manual is available online at https://www.cdc.gov/niosh/docs/99-101/pdfs/99-101.pdf.
Supervision is the ultimate form of leadership within the helping professions. Treating supervisees as people, not as things, is the essence of person-centered supervision, a concept extensively explored in this course.
The course began with the basic foundations of defining supervision within the helping professions, and then advanced to integrating ideas from person-centered approaches to helping others to fully describe person-centered supervision. Specific skills for developing empathy in supervisory work with others were explored, using supervisee case studies to guide the discussion and reflective exercises to help integrate and personalize the learning. Other common supervisory issues were examined, including counselor development, working with resistant supervisees, legal and ethical issues, and self-care as a supervision issue.
Person-centered supervision is not a new model or a radical approach to clinical supervision. Rather, person-centered supervision is an approach, a mindset that can be implemented alongside any other existing models or techniques used in supervision. This approach embraces the notion that practicing some common sense logic and honoring supervisees as people, in the same way one would honor clients, is the best way to reach them. Person-centeredness can bring about the high-quality formation necessary in the helping professions.
Autonomy: a principle of motivational interviewing affirming one's right and capacity for self-direction and informed choice.
Clinical supervision: a relationship in the helping professions that implies a simultaneous managerial and mentorship component. Per Falender and Shafranske, clinical supervision is "a distinct professional activity in which education and training aimed at developing science-informed practice are facilitated through a collaborative, interpersonal process. It involves observation, evaluation, feedback, the facilitation of supervisee self-assessment, and the acquisition of instruction and skills by instruction, modeling, and mutual problem solving" [7].
Collaboration: a principle of motivational interviewing involving a partnership that honors the client's/supervisee's expertise and perspectives.
"Compliment sandwich": sharing with students or supervisees something that they are doing right, then inserting an area of improvement, and ending with a compliment.
Congruence: a Rogerian, person-centered term meaning that the supervisee and supervisor are on the "same page" in terms of goals and direction for the supervisory relationship.
Consultation: collaborating with a specialist who is called upon for his or her expert advice in the field, for instance, in matters of assessment, diagnosis, or treatment planning.
Empathy: derived from Greek roots meaning "in" and "feeling;" coined as a philosophical concept in 1858 by a German philosopher. According to Stedman's Medical Dictionary, it is defined as "direct identification with, understanding of, and vicarious experience of another person's situation, feelings, and motives" [12].
Evocation: a principle of motivational interviewing that the resources and motivation for change are presumed to reside within the client/supervisee. Intrinsic motivation for change is enhanced by drawing on the supervisee's own perceptions, goals, and values.
Feedback: commentary about performance, either positive or negative, delivered with the intention of helping a person to better grow or improve in his or her work. Therapists can receive feedback from clients, supervisees can receive feedback from supervisors, and supervisors can receive feedback from their supervisees.
Formation: a spiritual term often used in seminaries and monastic life to describe the process by which a person responding to his or her vocation (or "calling") learns how to live their calling to the fullest.
Motivational interviewing: an approach to counseling/change attributed to Miller and Rollnick that advocates asking a series of questions to enhance a person's overall drive toward change; represents a shift from confrontational or directive approaches to counseling [31].
Non-malfeasance: the ethical principle of doing no harm.
Relational alliance: when two parties, such as a supervisor/supervisee, are engaging in a mutually respectful, trusting interaction, working toward a goal or benefit.
Rupture: a break or a disturbance that causes impairment in flow or function in a relational alliance.
Self-care: in the helping professions, time and energy to care for oneself.
Somatic empathy: noticing physical responses to a person or a situation that are likely mirroring what that person is experiencing.
Supervision: in a general sense, one party is overseeing another.
Unconditional positive regard: a Rogerian, person-centered term meaning fundamental, total acceptance of the person, regardless of what he or she does or has done.
The codes of ethics of various professional associations form the framework for clinical practice and supervision. The following sections contain excerpts from various codes of ethics that pertain to supervisors specifically. Professionals are encouraged to become familiar with their state and national codes, rules, and regulations.
Several sections in the NBCC's Code of Ethics have applicability to supervisors and supervisees [10]. According to the Code:
Nationally certified counselors (NCCs) who act as counselor educators, field placement or clinical supervisors shall not engage in sexual or romantic intimacy with current students or supervisees. They shall not engage in any form of sexual or romantic intimacy with former students or supervisees for two years from the date of last supervision contact.
NCCs who provide clinical supervision services shall keep accurate records of supervision goals and progress and consider all information gained in supervision as confidential except to prevent clear, imminent danger to the client or others or when legally required to do so by a court or government agency order. In cases in which the supervisor receives a court or governmental agency order requiring the production of supervision records, the NCC shall make reasonable attempts to promptly notify the supervisee. In cases in which the supervisee is a student of a counselor education program, the supervisor shall release supervision records consistent with the terms of the arrangement with the counselor education program.
NCCs who provide clinical supervision services shall intervene in situations where supervisees are impaired or incompetent and thus place client(s) at risk.
NCCs who provide clinical supervision services shall not have multiple relationships with supervisees that may interfere with supervisors' professional judgment or exploit supervisees. Supervisors shall not supervise relatives.
NCCs who provide supervision services shall present supervisees with feedback according to a schedule with identified evaluation dates as well as on appropriate occasions throughout the process.
NCCs shall promote the welfare of supervisees by discussing ethical practices relating to supervision as well as the legal standards that regulate the practice of counseling.
NCCs who provide supervision services shall establish with their supervisees procedures for responding to crisis situations or expressing concerns regarding the supervision process. This information shall be provided in verbal and written formats.
NCCs who provide supervision services shall present accurate written information to supervisees regarding the NCC's credentials as well as information regarding the process of supervision. This information shall include any conditions of supervision, supervision goals, case management procedures, confidentiality and its limitations, appraisal methods and timing of evaluations.
NCCs shall include all electronic communications exchanged with clients and supervisees, including those through digital technology and social media methods, as a part of the record, even when strictly related to clerical issues such as change of contact information or scheduling appointments. All electronic therapeutic communication methods shall use encryption and password security.
NCCs who provide supervision services to supervisee's who have more than one supervisor (e.g., field placement and university) shall exchange contact information and communicate regularly about the shared supervisee's performance.
NCCs who act as university, field placement, or clinical supervisors shall ensure that supervisees provide accurate information to clients about the supervisee's professional status (e.g., intern, licensed, etc.)
NCCs who act as university, field placement, or clinical supervisors shall require that supervisees provide the supervising NCC's name, credentials, and contact information to the supervisee's clients.
The ACA Code of Ethics contains sections dealing specifically with supervisor competence, relationships, responsibilities, and processes [11]. The following is an excerpt of these sections:
Prior to offering supervision services, counselors are trained in supervision methods and techniques. Counselors who offer supervision services regularly pursue continuing education activities, including both counseling and supervision topics and skills.
Counseling supervisors are aware of and address the role of multiculturalism/diversity in the supervisory relationship.
When using technology in supervision, counselor supervisors are competent in the use of those technologies. Supervisors take the necessary precautions to protect the confidentiality of all information transmitted through any electronic means.
Counseling supervisors clearly define and maintain ethical professional, personal, and social relationships with their supervisees. Supervisors consider the risks and benefits of extending current supervisory relationships in any form beyond conventional parameters. In extending these boundaries, supervisors take appropriate professional precautions to ensure that judgment is not impaired and that no harm occurs.
Sexual or romantic interactions or relationships with current supervisees are prohibited. This prohibition applies to both in-person and electronic interactions or relationships.
Counseling supervisors do not condone or subject supervisees to sexual harassment.
Supervisors are prohibited from engaging in supervisory relationships with individuals with whom they have an inability to remain objective.
Supervisors are responsible for incorporating into their supervision the principles of informed consent and participation. Supervisors inform supervisees of the policies and procedures to which supervisors are to adhere and the mechanisms for due process appeal of individual supervisor actions. The issues unique to the use of distance supervision are to be included in the documentation as necessary.
Supervisors establish and communicate to supervisees procedures for contacting supervisors or, in their absence, alternative on-call supervisors to assist in handling crises.
Supervisors make their supervisees aware of professional and ethical standards and legal responsibilities.
Supervisors or supervisees have the right to terminate the supervisory relationship with adequate notice. Reasons for considering termination are discussed, and both parties work to resolve differences. When termination is warranted, supervisors make appropriate referrals to possible alternative supervisors.
Students and supervisees have a responsibility to understand and follow the ACA Code of Ethics. Students and supervisees have the same obligation to clients as those required of professional counselors.
Students and supervisees monitor themselves for signs of impairment from their own physical, mental, or emotional problems and refrain from offering or providing professional services when such impairment is likely to harm a client or others. They notify their faculty and/or supervisors and seek assistance for problems that reach the level of professional impairment, and, if necessary, they limit, suspend, or terminate their professional responsibilities until it is determined that they may safely resume their work.
Before providing counseling services, students and supervisees disclose their status as supervisees and explain how this status affects the limits of confidentiality. Supervisors ensure that clients are aware of the services rendered and the qualifications of the students and supervisees rendering those services. Students and supervisees obtain client permission before they use any information concerning the counseling relationship in the training process.
In 2013, the NASW and the Association of Social Work Boards (ASWB) developed and published the Best Practice Standards in Social Work Supervision [39]. This guideline provides information on a wide range of issues that may arise during social work supervision, and many of the ethical standards are derived from the NASW's Code of Ethics, specifically the following precepts [34]:
3.01(a) Social workers who provide supervision or consultation (whether in-person or remotely) should have the necessary knowledge and skill to supervise or consult appropriately and should do so only within their areas of knowledge and competence.
3.01(b) Social workers who provide supervision or consultation are responsible for setting clear, appropriate, and culturally sensitive boundaries.
3.01(c) Social workers should not engage in any dual or multiple relationships with supervisees in which there is a risk of exploitation of or potential harm to the supervisee, including dual relationships that may arise while using social networking sites or other electronic media.
3.01(d) Social workers who provide supervision should evaluate supervisee' performance in a manner that is fair and respectful.
The following standards are excerpted from the Best Practice Standards in Social Work Supervision sections dealing with ethical issues and dilemmas in clinical social work supervision [39]:
Supervisors have the responsibility to address any confusion that supervisees may encounter as a result of ethical demands. A supervisor should be aware of the differences between professional ethics, core values, and personal moral beliefs and help the supervisee to distinguish these elements when making practice decisions. Supervisors can use the supervisory relationship as a training ground for ethical discretion, analysis, and decision-making.
Supervisors help supervisees learn ethical decision-making, a process that is both cognitive and emotional. Supervisors should discuss and model the process of identifying and exploring problems, looking at issues, values, principles, and regulations. Supervisors and their supervisees should discuss possible consequences, as well as costs and benefits, of certain actions. They should explore what actions best achieve fairness, justice, and respect for others, make a decision about actions to be taken, and evaluate them after implementation. When a supervisee makes an ethical mistake, he or she, with the assistance of the supervisor, should try to ameliorate any damage and learn how to avoid that mistake in the future. If appropriate or required by the jurisdiction, the violation may have to be reported to the licensing board.
The supervisory relationship is an excellent forum for supervisees to learn about boundaries with clients. Ethical issues related directly to supervision include the nature of the professional responsibility to the supervisee, appropriate boundaries, and responsibilities when dealing with incompetent or unethical behavior. Becoming involved in a romantic or familial relationship with a supervisee is an ethical violation and should be strictly avoided because it creates marked role conflict that can fatally undermine the supervisory relationship. If the supervisor recognizes a potential boundary issue with a supervisee, he or she should acknowledge it, assess how the boundary issue has affected supervision, and resolve the conflict. Although the supervisory relationship is between professionals, supervisors usually have more power in the relationship than supervisees. To avoid boundary problems and conflicts of interest with a supervisee, the ethical supervisor must accept his or her power and be comfortable in using that authority to ensure accountability and protect clients. Other ethical considerations include the following:
A supervisor should always focus on the goals of supervision and the nature of the supervisory relationship and avoid providing psychotherapy services to the supervisee.
Supervisors working with more than one supervisee should see each supervisee as an individual and adapt to that supervisee's needs. At the same time, supervisors must be fair and consistent when providing supervision to multiple supervisees.
Supervisors should be discreet in sharing personal information and not allow it to become the focus of supervision. When personal information is disclosed, it should be brief and support the goals of supervision. Supervisors should explain their comments and rationale to help supervisees gain understanding of appropriate techniques to use in the interview process with clients.
Supervisors make supervisees aware of safety issues and train them how to respond to workplace conflict, respond to threats and harassment, protect property, and deal with assaults and their emotional aftermath. Supervisors help supervisees plan for safety in the office and in the community by learning non-violent response strategies and appropriate ways to respond to crises.
The social work supervisor should decide whether an alternative practice, a non-traditional social work intervention, is the best modality of treatment for a supervisee to use with a client. When a supervisee uses an alternative practice, the supervisor should have expertise of that practice and ensure that the supervisee has the prerequisite training and knowledge to perform the alternative practice. In situations in which the supervisor does not have the skills to provide the alternative practice, it may be necessary to involve a second supervisor. In such cases, the two supervisors should work closely together to avoid conflicts and ensure effective use of the alternative practice for the client.
Social work supervisors share responsibilities for the services provided to clients. Liability of supervisors has been determined by the courts and includes direct liability related to negligent or inadequate supervision and vicarious liability related to negligent conduct by supervisees.
Supervisors and supervisees should both have professional liability insurance. In an agency setting, a supervisor's potential liability is affected by his or her level of responsibility and authority. Supervisors should familiarize themselves with the scope of their responsibility and authority, which may be specified in an agency written policy manual, the supervisor's job description, or a written contractual agreement.
The requirements and expectations of a supervisor's position also may affect liability, especially in situations in which the supervisor may have competing demands and is unable to adequately perform his or her supervisory functions. Such situations may present legal challenges.
1. Spence SH, Wilson J, Kavanagh D, Strong J, Worrall L. Clinical supervision in four mental health professions: a review of the evidence. Behaviour Change. 2001;18(3):135-155.
2. Kadushin A, Harkness D. Supervision in Social Work. 5th ed. New York, NY: Columbia University Press; 2014.
3. Munson CE. Handbook of Clinical Social Worker Supervision. 3rd ed. New York, NY: Routledge; 2001.
4. Pack M. Clinical supervision: an interdisciplinary review of literature with implications for effective practice in social work. Reflective Practice. 2009;10(5):657-668.
5. Corey G, Haynes R, Moulton P, Muratori M. Clinical Supervision in the Helping Professions: A Practical Guide. 2nd ed. Alexandria, VA: The American Counseling Association; 2010.
6. Powell DJ. Clinical Supervision in Alcohol and Drug Abuse Counseling. 2nd ed. San Francisco, CA: Jossey-Bass; 2004.
7. Falender CA, Shafranske EP. Clinical Supervision: A Competency-Based Approach. Washington, DC: The American Psychological Association; 2004.
8. Hawkins P, Shohet R. Supervision in the Helping Professions. 4th ed. New York, NY: Open University Press/The McGraw Hill Companies; 2012.
9. Sears RW, Rudisill JR, Mason-Sears C. Consultation Skills for Mental Health Professionals. Hoboken, NJ: John Wiley & Sons; 2006.
10. National Board for Certified Counselors. NBCC Code of Ethics. Available at https://www.nbcc.org/Ethics. Last accessed March 20, 2022.
11. American Counseling Association. ACA Code of Ethics. Available at https://www.counseling.org/Resources/aca-code-of-ethics.pdf. Last accessed March 20, 2022.
12. 12. Stedman's Medical Dictionary. 29th ed. Philadelphia, PA: Lippincot, Williams, and Wilkins; 2013.
13. Weiner IB, Craighead WE (eds). The Corsini Encyclopedia of Psychology. Hoboken, NJ: Wiley; 2009.
14. Yalom I, Lesczc M. The Theory and Practice of Group Therapy. 5th ed. New York, NY: Basic Books; 2005.
15. Yalom I. The Gift of Therapy: An Open Letter to a New Generation of Therapists and Their Patients. London: Piatkus; 2009.
16. Horvath AO, Luborsky L. The role of the therapeutic alliance in psychotherapy. J Consult Clin Psychol. 1993;61(4):561-573.
17. Barber JP, Connolly MB, Crits-Christoph P, Gladis L, Siqueland L. Alliance predicts patients' outcome beyond in-treatment change in symptoms. J Consult Clin Psychol. 2000;68(6):1027-1032.
18. Flückiger C, Del Re AC, Wampold BE, Symonds D, Horvath AO. How central is the alliance in psychotherapy? A multilevel longitudinal meta-analysis. J Couns Psychol. 2012;59(1):10-17.
19. Duncan BL, Miller SD, Wampold BE, Hubble MA (eds). The Heart and Soul of Change: Delivering What Works in Therapy. 2nd ed. Washington, DC: American Psychological Association; 2009.
20. Rosenzweig S. Some implicit common factors in diverse methods of psychotherapy. Am J Orthopsychiatry. 1936;6(3):412-415.
21. Norcross JC (ed). Psychotherapy Relationships that Work: Evidence-Based Responsiveness. New York, NY: Oxford University Press; 2011.
22. Rothschild B, Rand M. Help for the Helper: The Psychology of Compassion Fatigue and Vicarious Trauma. New York, NY: W.W. Norton & Co.; 2006.
23. Marich J. EMDR Made Simple: 4 Approaches for Using EMDR with Every Client. Eau Claire, WI: Premiere Education and Media; 2011.
24. Dworkin M, Errebo N. Rupture and repair in the EMDR client/clinician relationship: now moments and moments of meeting. Journal of EMDR Practice and Research. 2010;4(3):113-123.
26. Hogan RA. Issues and approaches in supervision. Psychotherapy: Theory, Research, and Practice. 1964;1(3):139-141.
27. Hess AK. Growth in supervision: stages of supervisee and supervisor development. In: Kaslow FW (ed). Supervision and Training: Models, Dilemmas, and Challenges. New York, NY: Haworth Press; 1986; 51-67.
29. Rice DG. Supervision of cotherapy. In: Kaslow FW (ed). Supervision and Training: Models, Dilemmas, and Challenges. New York, NY: Haworth Press; 1986; 119-142.
30. D'Andrea M. Person-process model of supervision: a developmental approach. In: Bradley LJ (ed). Counselor Supervision. 4th ed. Philadelphia, PA: Brunner-Routledge; 2010.
31. Miller WR, Rollnick S. Motivational Interviewing: Helping People Change. 3rd ed. New York, NY: Guilford Press; 2012.
32. Syracuse University. Ethical and Legal Issues in Supervision. Available at https://soe.syr.edu/departments/academic/counseling-human-services/modules/supervision/. Last accessed March 20, 2022.
33. National Institutes of Health. Greek Medicine: The Hippocratic Oath. Available at https://www.nlm.nih.gov/hmd/greek/greek_oath.html. Last accessed March 20, 2022.
34. National Association of Social Workers. NASW Code of Ethics. Available at https://www.socialworkers.org/About/Ethics/Code-of-Ethics/Code-of-Ethics-English. Last accessed March 20, 2022.
35. Barnett JE. Positive ethics, risk management, and defensive practice. The Maryland Psychologist. 2007;53(1):30-31.
36. Norcross JC, Guy JD Jr. Leaving it at the Office: A Guide to Psychotherapist Self-Care. 2nd ed. New York, NY: The Guilford Press; 2018.
37. Edwards D, Burnard P, Hannigan B, et al. Clinical supervision and burnout: the influence of clinical supervision for community mental health nurses. J Clin Nurs. 2006;15(8):1007-1015.
Mention of commercial products does not indicate endorsement.