Diabetes is a serious and costly health problem in the United States. Perhaps more than any other chronic disease process, diabetes management requires substantial and ongoing self-care activity on the part of the patient or caregiver. For example, people with diabetes often need to test blood glucose several times a day. Many need to know how to administer insulin and to frequently adjust dosages. At the very least, people with diabetes continually contend with lifestyle choices related to the food they eat, the activity they engage in and demands upon their time and energy. Because the self-care needs of the patient with diabetes are significant, nursing care is most effective when it enables the patient to reach an optimal level of independence based upon individual need.
This course is designed for all nurses and behavioral health professionals involved in the care of patients with diabetes.
The purpose of this course is to provide nurses and behavioral health professionals with the information and resources needed to develop proficiency in teaching and caring for the patient with diabetes.
Upon completion of this course, you should be able to:
- Discuss the significance of diabetes in terms of prevalence and costs.
- Outline the pathophysiology of diabetes.
- Identify various classifications of diabetes.
- Recognize the acute complications of diabetes, including hyperglycemia, diabetic ketoacidosis, and hyperosmolar hyperglycemic syndrome.
- Identify the chronic complications of diabetes and the patient education principles related to each.
- Discuss the importance of facilitating diabetes self-care and describe interventions that support it.
- Identify components of effective diabetes self-management education programs.
- Analyze benefits and practices related to blood glucose monitoring.
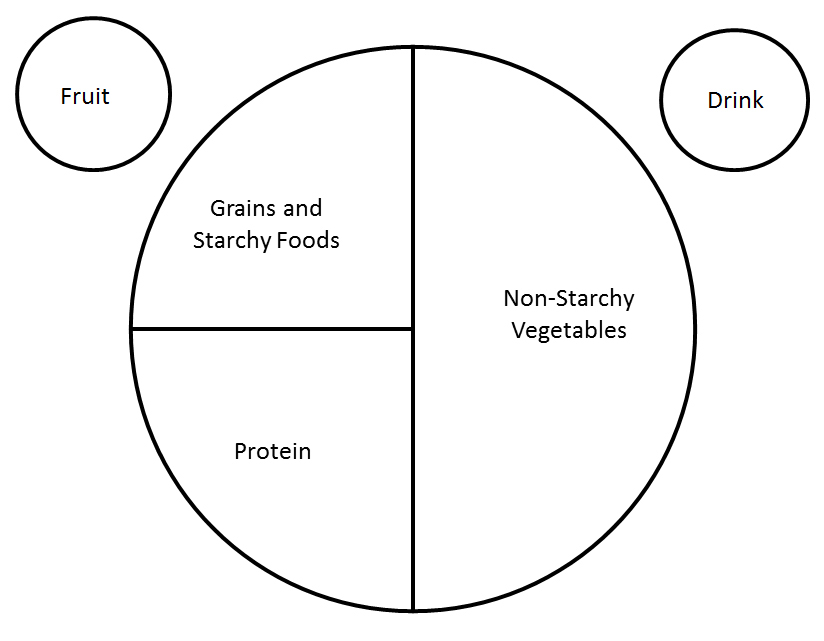
- Describe meal planning methods and nutritional guidelines for people with diabetes.
- Discuss medications for diabetes in terms of mechanism of action, nursing implications, and patient teaching principles.
- Recall the principles and practices of insulin therapy, including measures to prevent and treat hypoglycemia.
- Outline benefits and precautions related to exercise for the person with diabetes.
- Discuss the pathology of the diabetic foot and standards of preventive care.
- Describe the impact of stress on blood glucose control.
- Define cultural competence and discuss its relevance to diabetes care.
Susan Semb, MSN, CDCES, is a retired RN who received her Master's degree in nursing from the University of San Diego. Her nursing experience includes direct patient care, case management, staff development, program development, and health education. She spent the majority of her nursing career working as a diabetes educator in the health education department of a major health maintenance organization. Ms. Semb has also authored other continuing education courses for nurses published by NetCE and contributed to nursing books and other publications. In her retirement, Ms. Semb enjoys travel, line dancing, and pursuing an interest in antiques and vintage items.
Contributing faculty, Susan Semb, MSN, CDCES, has disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
Mary Franks, MSN, APRN, FNP-C
Alice Yick Flanagan, PhD, MSW
The division planners have disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
Sarah Campbell
The Director of Development and Academic Affairs has disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
The purpose of NetCE is to provide challenging curricula to assist healthcare professionals to raise their levels of expertise while fulfilling their continuing education requirements, thereby improving the quality of healthcare.
Our contributing faculty members have taken care to ensure that the information and recommendations are accurate and compatible with the standards generally accepted at the time of publication. The publisher disclaims any liability, loss or damage incurred as a consequence, directly or indirectly, of the use and application of any of the contents. Participants are cautioned about the potential risk of using limited knowledge when integrating new techniques into practice.
It is the policy of NetCE not to accept commercial support. Furthermore, commercial interests are prohibited from distributing or providing access to this activity to learners.
Supported browsers for Windows include Microsoft Internet Explorer 9.0 and up, Mozilla Firefox 3.0 and up, Opera 9.0 and up, and Google Chrome. Supported browsers for Macintosh include Safari, Mozilla Firefox 3.0 and up, Opera 9.0 and up, and Google Chrome. Other operating systems and browsers that include complete implementations of ECMAScript edition 3 and CSS 2.0 may work, but are not supported. Supported browsers must utilize the TLS encryption protocol v1.1 or v1.2 in order to connect to pages that require a secured HTTPS connection. TLS v1.0 is not supported.
The role of implicit biases on healthcare outcomes has become a concern, as there is some evidence that implicit biases contribute to health disparities, professionals' attitudes toward and interactions with patients, quality of care, diagnoses, and treatment decisions. This may produce differences in help-seeking, diagnoses, and ultimately treatments and interventions. Implicit biases may also unwittingly produce professional behaviors, attitudes, and interactions that reduce patients' trust and comfort with their provider, leading to earlier termination of visits and/or reduced adherence and follow-up. Disadvantaged groups are marginalized in the healthcare system and vulnerable on multiple levels; health professionals' implicit biases can further exacerbate these existing disadvantages.
Interventions or strategies designed to reduce implicit bias may be categorized as change-based or control-based. Change-based interventions focus on reducing or changing cognitive associations underlying implicit biases. These interventions might include challenging stereotypes. Conversely, control-based interventions involve reducing the effects of the implicit bias on the individual's behaviors. These strategies include increasing awareness of biased thoughts and responses. The two types of interventions are not mutually exclusive and may be used synergistically.
#94395: Diabetes Care and Patient Education
Diabetes is a serious and costly health problem in the United States. There are an estimated 38.4 million cases in the United States, representing 11.6% of the U.S. population [1; 2]. Diabetes accounts for an overall economic burden of $413 billion annually, including a disproportionate use of hospital inpatient care, outpatient and physician office care, emergency visits, skilled nursing days, and home health visits [2]. In addition to these economic costs, diabetes takes an incalculable toll on the individual in terms of lost productivity, disability, decreased quality of life, and early mortality [1,3,4].
Perhaps more than any other chronic disease process, diabetes management requires substantial and ongoing self-care activity on the part of the patient or caregiver. For example, people with diabetes are often required to test blood glucose several times a day. Many must know how to administer insulin and to adjust dosages frequently. At the very least, people with diabetes continually contend with lifestyle choices related to the food they eat, the activities in which they engage, and the demands upon their time and energy. When people with diabetes receive education resulting in appropriate self-care, clinical outcomes and quality of life are improved [5,6]. Because the self-care needs of the patient with diabetes are significant, nursing care is most effective when it enables the patient to reach an optimal level of independence based on individual need.
A landmark study, published in 1993, reported that improved control of blood glucose could significantly slow the onset and progression of diabetic retinopathy, renal failure, and neuropathy in people with type 1 diabetes [7]. Subsequently, the results of another major study concluded that lowering the blood glucose can reduce these complications in people with type 2 diabetes as well [8]. These studies have also suggested that blood glucose control can also reduce cardiovascular risk in people with diabetes. Other studies and many epidemiologic reports have agreed that the health risks associated with diabetes can be averted with good glycemic control [9].
In spite of significant evidence that controlling blood glucose can improve outcomes in people with diabetes, many still do not adhere to at least some aspect of their treatment regimen. Although some patients attend a formal self-management education program, many people with diabetes have not done so. Even patients who have received quality self-care education face significant challenges with regard to initiating and maintaining the complex behavioral changes that are required for effective disease management.
Diabetes places a substantial burden on the individual, society, and the economy. In the United States, 16.5 million (29.2%) people older than 65 years of age have diabetes, and the numbers are growing [10]. It is projected that one in three Americans born in 2000 will have diabetes over the course of their lives [11]. National statistics indicate that with 38.4 million cases in the United States, 11.6% of the total population has this disease [10]. Approximately 8.5 million individuals with diabetes have not been diagnosed [1,10]. Another 97.6 million people are estimated to have prediabetes, a condition that significantly increases the risk for developing diabetes [10]. Diabetes accounts for substantial loss in overall worker productivity, costing approximately $106 billion in lost productivity in 2018 [10]. Reductions in productivity were associated with absenteeism, decreased efficiency at work, disability, and early death [3]. In addition to economic loss, chronic complications of diabetes can significantly diminish quality of life for the individual, accounting for more new cases of blindness, end-stage renal disease, and lower extremity amputation than any other medical diagnosis [1].
Healthcare utilization by people with diabetes is considerable. Researchers report that people with diagnosed type 1 diabetes incur an average of $14,856 in healthcare expenditures per year, while those with type 2 diabetes acquire approximately $9,677 in expenditures [3]. This equates to healthcare expenditures that are roughly 2.6 times higher than for people without diabetes [4]. Diabetes contributes to longer hospital length of stay and higher rates of physician office and emergency department visits. A substantial amount of healthcare utilization by people with diabetes is associated with the chronic complications of this condition, particularly cardiovascular disease, neurologic symptoms, and renal complications. As sobering as these statistics are, it is predicted that the toll of diabetes will increase, related to higher rates of obesity and increasing cases of type 2 diabetes in children [12].
The prevalence of diabetes is greater in some racial and ethnic populations. Estimated prevalence rates for diabetes among adults 20 years of age and older in the following racial/ethnic groups are [2,10]:
Non-Hispanic White Americans: 6.9%
Asian Americans: 9.1%
Hispanic/Latino Americans: 11.7%
Non-Hispanic Black Americans: 12.1%
Native Americans/Alaska Natives: 13.6%
Rates of diabetes in Native Americans vary among more than 570 federally recognized tribes, bands, pueblos, and villages in the United States. Overall, Native Americans are almost twice as likely as non-Hispanic White Americans to have diagnosed diabetes. In some American Indian and Alaska Native communities, the prevalence of diabetes among adults is as high as 60%. Native Americans in southern Arizona have rates of 22% [13]. The highest rates of diabetes for any population occur in the Pima Indians of Arizona, who have the highest prevalence (50%) in the world [13]. Studies reveal that diabetes is increasing at an alarming rate among young Native Americans and Alaska Natives, causing concern for the impact on future generations [14].
The prevalence of diabetes in non-Hispanic Black Americans (14.0%) is much higher than in non-Hispanic White Americans (8.0%). Non-Hispanic Black American men are 2.2 times more likely to start treatment for end-stage renal disease than non-Hispanic White men [15].
Among the subdivisions of Hispanic groups, diabetes prevalence rates are 9.0% for Cubans, 11.1% for Mexican Americans, and 7.3% for Puerto Ricans. Mexican Americans have higher rates of end-stage renal disease and are 0.64 times more likely to die from diabetes than their non-Hispanic White counterparts [1,16].
Asian Americans are 6% more likely to be diagnosed with diabetes than adults of the total population [17]. Among Asian American adults, the age-adjusted rate of diagnosed diabetes was 7.1% for Chinese, 12.2% for Filipinos, 10.8% for Asian Indians, and 8.9% for other Asians [1].
Diabetes is a disease that affects the body's ability to control and utilize its supply of fuel. When glucose, the body's main fuel source, is not properly regulated, blood glucose levels rise. If high blood glucose levels are sustained over time, abnormalities in the structure of blood vessels and nerves can result. This leads to organ and tissue damage and can have serious consequences affecting the eyes, kidneys, and nerves. Other pathologic processes and additional risk factors are strongly related to the development of cardiovascular disease, which is the leading cause of death in people with diabetes.
Glucose is made available to the body in two ways: from food that has been ingested and through the body's own production of glucose by the liver. Although some tissues and organs can derive energy from other sources, the brain and central nervous system rely almost entirely upon glucose. Because the brain cannot store or synthesize glucose, it depends on a continuous supply of glucose from the circulation and extracts its energy supply on a minute-by-minute basis.
Three organ systems are involved in the regulation and utilization of glucose by the body. They are the liver, the pancreas, and the skeletal muscle tissue. The liver plays two roles in the regulation of blood glucose. One is the storage and release of glucose that has been ingested from the diet; the other is the synthesis of its own glucose supply. (The process of glucose production by the liver is called gluconeogenesis.) Normally, when blood glucose levels are low, the liver releases some of its stored or synthesized glucose and blood levels rise. Conversely, when blood glucose levels are high, the liver stops producing and releasing glucose and blood levels fall.
The pancreas supplies two antagonistic hormones that control glucose metabolism: insulin and glucagon. Insulin allows glucose to enter the cells, where it can be utilized for energy. Glucagon has an action opposite that of insulin. Its role is to maintain blood glucose levels between meals and during the fasting state. When blood glucose levels are high, such as after eating, the secretion of glucagon by the pancreas is inhibited.
Muscle tissue is the third organ system involved in glucose metabolism. As the primary target organ for the action of insulin, the skeletal muscle tissue contains the majority of insulin receptor sites. When insulin binds with receptor sites on the skeletal muscle, the "doors are open" for the entry of glucose into the cell. When muscle tissue receptor sites are not working efficiently, a condition called insulin resistance occurs. Insulin resistance plays a major role in the development of type 2 diabetes.
More recently, the important role that incretin hormones play in glucose regulation has become more clearly understood. Incretins are digestive hormones that are released from the small intestine within minutes of eating in response to the post-meal rise in blood glucose. The incretins help lower blood sugar by stimulating insulin release, slowing gastric emptying, and decreasing glucagon production from the pancreas [18]. Two incretin hormones mediate these actions: glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic peptide (GIP).
Any one of three major abnormalities of metabolism can be responsible for inducing the diabetes disease process. The first is abnormal insulin secretion by the pancreas. In this situation, insulin production by the pancreas is either absent or insufficient to meet the body's needs. Because the role of insulin is to facilitate the passage of glucose into cells, glucose remains unused and continues to circulate in the blood when insulin is either not available or not working efficiently.
Insulin resistance is the second major pathologic process in diabetes. This refers to impairment in the body's ability to utilize insulin. With insulin resistance, blood levels of insulin may be high, but receptor sites for it are not available.
The third major metabolic abnormality in diabetes is related to inappropriate glucose production by the liver. As an organ that can make or store glycogen, the liver plays a major role in regulation of blood glucose levels. In normal physiology the liver can store glycogen and release it as glucose as needed to keep blood glucose in a normal range. Insulin resistance at receptor sites on the liver can prevent it from receiving the signals it needs to stop releasing glucose when blood levels are sufficient. A helpful analogy for this is to think of the affected liver as a leaky faucet. Instead of turning off and on appropriately in response to the body's need for glucose, the liver (i.e., the faucet) releases glucose in a haphazard way without regard to what the body needs at a particular time. When this occurs, blood glucose continues to rise even though levels may already be high.
More recently, other defects in addition to the classic triumvirate have been identified in the pathophysiology of type 2 diabetes. In total, eight organ systems are implicated [19,20]:
Muscles: Failure of glucose uptake in the muscles after carbohydrate ingestion results in postprandial hyperglycemia.
Beta cells of the pancreas: Insulin resistance puts stress on the pancreatic beta cells, and they eventually begin to fail.
Liver: Insulin resistance at the hepatic receptor sites is manifested by glucose overproduction and impaired suppression of hepatic glucose production.
Fat: When the pancreas produces excessive amounts of insulin to compensate for resistance, free fatty acid concentration in the blood increases. This causes a rise in toxic metabolites in the lever, muscles, and pancreatic beta cells, which enhances insulin resistance.
Alpha cells of the pancreas: Insulin resistance in these cells leads to increased fasting glucagon and delayed glucagon suppression.
Gastrointestinal tract: People with type 2 diabetes are deficient in incretins, hormones secreted from the gastrointestinal tract within minutes of eating and that communicate to the pancreas that insulin should be released.
Kidneys: Increased gluconeogenesis and enhanced glucose absorption contribute to hyperglycemia.
Brain: Insulin resistance in the hypothalamus may disrupt glucose homeostasis and contribute to the pathogenesis of type 2 diabetes.
Discoveries regarding the role of diverse body systems in the pathophysiology of type 2 diabetes have spurred the development of multiple drugs to target specific defects. These drugs will be discussed in detail later in this course.
Diabetes encompasses a relatively large and somewhat diverse group of metabolic diseases. The American Diabetes Association (ADA) has classified four different clinical classes of diabetes based upon etiology: type 1, type 2, gestational, and specific types due to other causes [6]. In addition, the ADA has defined categories of increased risk for diabetes, collectively known as "prediabetes." Many of the types of diabetes identified by the ADA are not commonly encountered in nursing practice and are related to rare genetic and immune-mediated syndromes; these fall into the "other causes" category [6]. The common pathologic factors that categorize all of these diseases as diabetes relate to abnormal insulin production, impaired insulin utilization, or both [6].
The vast majority of diabetes cases are either type 1 or type 2 diabetes. Other types of diabetes that may be encountered in routine nursing practice include gestational diabetes and prediabetes. The focus of this course will be on type 1 and type 2 diabetes. Gestational, secondary, and prediabetes will be discussed briefly in this section of the course only.
Prediabetes is the term used for individuals whose glucose levels do not meet the criteria for diabetes yet have abnormal carbohydrate metabolisms [6]. People with prediabetes are defined by the presence of impaired fasting glucose (IFG) and/or impaired glucose tolerance (IGT). Criteria for defining prediabetes are [6]:
Fasting plasma glucose: 100–125 mg/dL (5.6–6.9 mmol/L)
Two-hour postprandial glucose tolerance test (during 75-g oral glucose tolerance test): 140–199 mg/dL (7.8–11.0 mmol/L)
Glycated hemoglobin (HbA1c): 5.7% to 6.4%
According to the Centers for Disease Control and Prevention (CDC), 97.6 million people (38.0% of adults) in the United States have prediabetes [1]. Identifying patients with prediabetes is vital to delaying or preventing the onset of type 2 diabetes. Research has shown that lifestyle management can prevent progression to diabetes. When people with prediabetes follow a healthy diet and engage in 150 minutes of moderate intensity exercise per week, leading to a 5% to 7% loss of body weight, they can reduce their risk for diabetes by roughly 58% [21,22].
Type 1 diabetes results when the person's pancreas cannot produce any of its own insulin for use by the body. If the person with type 1 diabetes does not receive insulin from an outside source (e.g., injections), he or she is likely to develop a life-threatening condition known as ketoacidosis. Patients with type 1 diabetes will always require insulin from an outside source to stay alive.
Although type 1 diabetes is the most common form of diabetes in youth, the traditional paradigms of type 1 diabetes occurring only in children and type 2 diabetes occurring only in adults are no longer accurate, as both diseases occur in both age groups [6]. Children with type 1 diabetes often present with the hallmark symptoms of polyuria/polydipsia; approximately one-half present with diabetic ketoacidosis (DKA). The onset of type 1 diabetes may be more variable in adults [6]. The features most useful in identifying type 1 diabetes include younger age at diagnosis (<35 years) with lower BMI (<25 kg/m2), unintentional weight loss, ketoacidosis, and glucose >360 mg/dL at presentation [6]. Difficulties in distinguishing diabetes type may occur in all age groups at onset; however, the diagnosis becomes more obvious over time in patients with beta cell deficiency [6]. Overweight and obesity are common in children with type 1 diabetes, and diabetes-associated autoantibodies may be present in pediatric patients. The presence of islet autoantibodies has been associated with a faster progression to insulin deficiency [6].
Advances are being made in islet cell transplantation for the treatment or cure of type 1 diabetes. For this procedure, donor cells are harvested from cadavers. For an average-sized person, two donor organs are usually required to reap approximately 1 million islets. Because the islets are very fragile, transplant usually occurs immediately after harvesting. A relatively simple procedure, islet cell transplant involves ultrasound placement of a catheter into the recipient's pancreas through which the islet cells are injected. After a time, the cells attach to blood vessels and begin releasing insulin. A major risk of islet cell transplantation is that anti-rejection drugs are needed to keep the transplanted cells functioning and these drugs can have significant side effects. It is not known how long the islet cells survive after transplant. Because there is an extreme shortage of available donor cells, islet cell transplants are not commonly done [23]. With the approval of islet cell therapy in 2023, islet transplantation is available outside clinical trials to treat certain adults with type 1 diabetes [23].
Pancreas transplantation is another possible way to cure type 1 diabetes. Whole pancreas transplants from cadaver donors or partial pancreas transplants from living relative donors may be used. Compared to islet cell transplant, whole or partial organ transplant is a complicated procedure with all the inherent risks of major surgery. Many times partial pancreas transplant occurs in conjunction with kidney transplant using the same living relative donor. In addition to the risks of major surgery, organ transplant requires the lifelong use of immunosuppressant drugs. Even with these drugs, about one-half of transplanted pancreases are rejected [23].
As stated, the traditional paradigms of type 1 diabetes occurring only in children and type 2 diabetes occurring only in adults are no longer accurate, as both diseases occur in both age groups [6]. Type 2 diabetes is by far the most common type of diabetes, accounting for 90% to 95% of cases [6]. This type of diabetes usually begins in people older than 30 years of age and most commonly occurs in people older than 55 years of age. However, as mentioned earlier, it can occur at younger ages as well. Regardless of age of onset, type 2 diabetes is more likely to occur in those who are overweight.
In the person with type 2 diabetes, the pancreas is able to produce at least some of its own insulin for use by the body. However, the insulin that is produced is either insufficient for the needs of the body or poorly utilized by the tissues. When available insulin is not readily utilized by the tissues, the condition is called insulin resistance.
The need for an outside insulin source is variable in people with type 2 diabetes. Individual cases of type 2 diabetes may be treated with diet therapy, oral medications, insulin, or any combination of these. A patient with type 2 diabetes usually has a pancreas that is able to produce enough of its own insulin to prevent ketoacidosis from occurring. However, these patients may require insulin injections to keep blood glucose levels under control for the prevention of other acute and chronic complications.
Gestational diabetes complicates approximately 10% of all pregnancies [6,24]. For many years, gestational diabetes has been defined as any degree of glucose intolerance first recognized during pregnancy, but this definition has limitations. Many cases of gestational diabetes represent pre-existing hyperglycemia that is first detected by routine screening in pregnancy (though routine screening is not widely performed in nonpregnant women of reproductive age) [6]. Ideally, women with risk factors who are planning pregnancy should be tested for undiagnosed diabetes prior to conception [6]. If not screened preconception, universal early screening before 15 weeks' gestation for undiagnosed diabetes may be considered, particularly in populations with a high prevalence of risk factors, including women of non-Hispanic Black, Hispanic/Latino, and Native American ethnicity, women who are obese, women with a personal history of gestational diabetes, and those with a family history of diabetes [6,25]. Otherwise, testing should be done at between 24 and 28 weeks' gestation, usually with a glucose tolerance test [1,6]. Women with gestational diabetes are at higher risk for hypertensive disorders and cesarean delivery. Fetal complications of gestational diabetes may include neural tube defects, perinatal death, large body size (macrosomia), lower Apgar scores, and childhood obesity [26]. Although most women with gestational diabetes will have normal glucose levels within six weeks postpartum, 35% to 60% will have developed diabetes in the next 10 to 20 years [27,28]. Women with gestational diabetes should be screened for prediabetes or diabetes at 4 to 12 weeks postpartum. Women with a history of gestational diabetes should have lifelong screening for the development of diabetes or prediabetes at least every three years [6]. Maintenance of a healthy body weight and regular physical activity may help prevent the onset of type 2 diabetes in this population [29].
Treatment of gestational diabetes includes close surveillance of mother and fetus due to the increased risks inherent in this type of pregnancy. Maternal fasting and postprandial blood glucose levels are usually checked several times a day. Nutritional management and regular physical activity are considered the first-line therapy. If this alone does not achieve target glucose levels, insulin therapy is usually indicated. Having gestational diabetes does not present any contraindications to breastfeeding. In fact, breastfeeding increases insulin sensitivity in the mother and can protect both mother and baby against diabetes [26].
Secondary diabetes occurs in some individuals due to a variety of medical conditions, including diseases and tumors that affect the liver or pancreas. Secondary diabetes may also occur in susceptible people who take medications that can impair glucose metabolism. Commonly used medications that can induce diabetes include corticosteroids, thyroid preparations, thiazide diuretics, and phenytoin, among others. Secondary diabetes usually resolves when the underlying cause is eliminated.
Patients with secondary diabetes should receive education in the treatment of the primary condition as well as the diabetes. However, focus upon the primary condition by the patient and healthcare providers may fragment diabetes education. Although secondary diabetes is generally expected to resolve, the patient will always be at risk for recurrence.
According to the ADA, criteria for the diagnosis of diabetes are [6]:
HbA1c ≥6.5% OR
Fasting plasma glucose ≥126 mg/dL OR
Two-hour plasma glucose ≥200 mg/dL during an oral glucose tolerance test OR
Random plasma glucose ≥200 mg/dL in a patient exhibiting classic symptoms of hyperglycemia
The glucose molecule is osmotically active and affects the fluid balance of the body. Therefore, an overabundance of glucose can result in hypotonic fluid loss, dehydration, and electrolyte depletion.
The primary symptoms of hyperglycemia are sometimes referred to as the "three polys" of diabetes. They are polydipsia (excessive thirst), polyuria (excessive urination), and polyphagia (excessive hunger). Polydipsia is related to intracellular dehydration, initiated after high levels of glucose in the blood remove water from the cells. Polyuria results when large amounts of glucose in the urine are accompanied by large losses of water. Polyphagia, which is most likely to occur in type 1 diabetes, is due to cellular starvation as stores of carbohydrates, fats, and proteins become depleted. Other signs and symptoms of hyperglycemia in diabetes include blurred vision, weakness, lethargy, and malaise.
Because the onset of type 2 diabetes usually develops slowly, signs and symptoms of hyperglycemia are not usually apparent in the early stages of the disease. Many times, patients with undetected type 2 diabetes are diagnosed after routine blood work, rather than as a result of seeking treatment for symptoms. In type 1 diabetes, however, symptoms of hyperglycemia generally develop suddenly and are more likely to be the chief complaint when medical attention is sought.
Episodic hyperglycemia is not usually considered a medical emergency. In most cases, the patient can manage incidents of hyperglycemia with alterations in diet, medication, or both. On the other hand, severe or prolonged hyperglycemia can be life threatening and may require urgent hospitalization.
The pathophysiology of hyperglycemic emergencies is similar in the two major types of diabetes, although important differences exist. Type 1 diabetes is associated with a life-threatening hyperglycemic complication called diabetic ketoacidosis (DKA). In type 2 diabetes, hyperosmolar hyperglycemic syndrome (HHS) (formerly referred to as hyperosmolar hyperglycemic nonketotic syndrome [HHNS]) refers to extremely high blood glucose requiring emergency treatment. While the pathophysiology of these two conditions is somewhat different, either may result in altered mental status, loss of consciousness, or death.
Ketones are acidic waste products of fat metabolism that can cause serious problems when excessive amounts are in the blood. When the body cannot use glucose for energy, it uses fat, a secondary source of energy. When body fat is utilized for energy, acidic waste products called ketones are formed.
When insulin remains unavailable, blood glucose rises, causing osmotic diuresis and loss of electrolytes. Meanwhile, ketones continue to accumulate as the body utilizes fat for its energy source. This leads to acidosis. The process becomes further complicated as acute renal failure may occur to ward off additional fluid losses. The severe dehydration, electrolyte imbalance, and acidosis associated with DKA will inevitably cause coma and death if left untreated.
People with type 2 diabetes are not prone to ketoacidosis because they usually make enough of their own insulin to prevent excessive breakdown of fat for metabolism. In the person with type 1 diabetes, ketoacidosis can develop rapidly when he or she has a cold, the flu, or other type of infection.
Hyperpnea (deep breathing) is usually present as a sign of DKA, reflecting the pulmonary system's response to acidosis. Acetone breath may occur. Signs of dehydration related to DKA include orthostatic hypotension and poor skin turgor. Acute abdominal pain, tenderness, and diminished or absent bowel sounds are commonly associated with DKA and frequently cause the patient to seek emergent treatment. Changes in mental status occur as the ketosis progresses.
Ketonuria develops as excess ketone bodies are excreted in the urine. Several types of urine dipsticks are available for testing urine ketones. The procedure for testing urine ketones is simple and can easily be taught to patients (Table 1). In order to detect the onset of ketosis in the early stages, patients with type 1 diabetes should test urine ketones when [30,31]:
Blood glucose is consistently elevated (>300 mg/dL).
They are sick with a cold, flu, or other type of infection.
They are experiencing nausea, vomiting, or diarrhea.
They are under extreme stress, physical or mental.
They feel tired, their skin is flushed, or they have difficulty breathing.
PROCEDURE FOR TESTING URINE KETONES: DIPSTICK METHODa
| |||||
| aIndividual ketone testing products may vary. Read the instructions for each product prior to use. Color charts for different products may not be interchangeable. Use only the color chart for a specific product. |
If a patient with type 1 diabetes has blood glucose greater than 300 mg/dL and moderate or greater ketones in the urine, the attending physician should be notified immediately. Immediate emergency treatment is required if the patient with developing DKA is unable to retain oral fluids or if there is an alteration in mental status [31]. Initial treatment of moderate-to-severe DKA normally includes intravenous fluid and electrolyte replacement to correct deficits of sodium, chloride, bicarbonate, potassium, phosphate, magnesium, and nitrogen. The goal of initial therapy is to expand intravascular and extravascular volume and to restore renal perfusion [32].
In cases of mild DKA, when the patient can retain oral fluids and can follow instructions for self-monitoring, medical care over the telephone may prevent hospitalization or an emergency room visit. Efforts should focus on rehydration, restoration of normal blood glucose, and education. Oral rehydration may be accomplished by taking 3–5 ounces of fluid per hour that may be given in small quantities every 20 to 30 minutes. Although taking sugar-free fluids is probably desirable in cases of hyperglycemia, it is more important to prevent or treat the dehydration than the hyperglycemia. Therefore, some programs condone the use of sugar-containing fluids regardless of the blood glucose level. In addition to fluid replacement, patients in mild DKA require supplemental insulin. Education to prevent DKA in the future is also required [31,33].
HHS is a syndrome of severe hyperglycemia and profound dehydration in individuals with type 2 diabetes. Ketosis does not occur in HHS because there is usually enough insulin present to prevent excessive fat metabolism. In the absence of acidosis, the patient with developing HHS does not usually experience the gastrointestinal symptoms (e.g., cramps, abdominal pain, nausea, vomiting) that occur in DKA. Therefore, the patient is less likely to seek medical attention, and extremely high blood glucose levels (usually >800 mg/dL) can result.
HHS generally has a slow and subtle onset, taking place over 24 hours to two weeks. As glucose builds in the blood, it produces a hyperosmolar state. This causes water to be pulled from body cells, including the brain cells, accounting for its signs and symptoms. These include signs of dehydration (e.g., dry skin and mucous membranes, extreme thirst) and signs of decreased mental status, such as lethargy and confusion. Seizures can also result from HHS. There may also be neurologic deficits that mimic stroke, such as unilateral weakness, aphasia, and sensory impairment. In fact, the onset of HHS may be mistaken for a stroke because it most frequently occurs in elderly people and has a slow, progressive onset.
Risk factors for HHS include any condition that results in fluid loss, for example diarrhea or the use of diuretics, especially the thiazides. Decreased fluid intake, infection, illness, and hypertonic tube feeding are other risk factors for HHS. Elderly patients with type 2 diabetes are at high risk for developing HHS, partially due to their diminished thirst sensation, and especially if they live alone or are cognitively impaired.
The primary treatment goal of HHS is fluid replacement and correction of electrolyte deficits. Insulin administration is another important part of treatment for HHS, although glucose levels will not decrease significantly in the dehydrated state. Elderly patients being treated for dehydration should be monitored very carefully for signs and symptoms of fluid overload and congestive heart failure.
Patients with type 2 diabetes and their families should be educated in the prevention and recognition of HHS, especially if the patient is at high risk. Preventive measures include maintenance of adequate hydration and adherence to medications and a meal plan. Proper sick day management and avoidance of medications that can exacerbate hyperglycemia are other effective preventive measures (Table 2).
SAMPLE PATIENT INSTRUCTION SHEET
EAT AND DRINK Follow your regular meal plan if you are able. If you are able to eat your regular meals, drink a cup of a no-calorie fluid every hour while you are awake, such as:
If you are not able to eat your usual meals, drink one cup of no-calorie fluid with one of the following every hour while awake:
REPORT Notify your healthcare provider if you have any of the following:
|
The chronic complications of diabetes have a profound effect on the healthcare system as well as the individual. In the United States, the treatment of these complications cost an estimated $106.3 billion in 2022 [34]. While the economic costs of diabetic complications are enormous, their effect on quality of life for the individual and family can be equally devastating. The CDC reports the impact of chronic complications on Americans with diabetes as [35]:
Leading cause of adult-onset blindness
Leading cause of end-stage renal disease
Significant morbidity and disability due to foot ulcer and lower extremity amputation
Increased risk for cardiovascular disease (two to four times greater in diabetic patient)
Significantly increased risk for nerve disease, periodontal disease, and a host of other health problems
Although statistics related to the chronic complications are grim, patients who keep their blood glucose as close to normal as possible can significantly reduce their risk for diabetes complications. Two landmark studies have clearly demonstrated these findings in individuals with both type 1 and type 2 diabetes. The Diabetes Control and Complications Trial (DCCT), conducted from 1983 to 1993, found that good glycemic control slows the onset and progression of eye, kidney, and nerve disease in people with type 1 diabetes [7]. Researchers continue to follow more than 90% of DCCT participants in a study called the Epidemiology of Diabetes Interventions and Complications (EDIC), assessing the incidence and predictors of cardiovascular disease events (e.g., heart attack, stroke, needed heart surgery) and diabetic complications related to the eye, kidney, and nerves [36]. The EDIC has shown that an individualized eye exam schedule results in fewer eye exams, lower costs, and faster diagnosis and treatment of advanced diabetic eye disease [36]. In 2002, the United Kingdom Prospective Diabetes Study (UKPDS) concluded that retinopathy, nephropathy, and perhaps neuropathy were reduced in patients with type 2 diabetes who maintained good glycemic control [8]. While there was a trend toward improved glycemic control from 1999 to the early 2010s, an analysis of data from adult diabetes participants in the National Health and Nutrition Examination Survey (NHANES) found that between 2007–2010 and 2015–2018, the percentage of adult NHANES participants in whom glycemic control was achieved declined from 57.4% to 50.5% [37].
The chronic complications of diabetes are usually classified as microvascular or macrovascular, according to the type of blood vessel damage that underlies the problem. Microvascular complications include retinopathy, nephropathy, and neuropathy. Macrovascular complications of diabetes are coronary artery disease, cerebral artery disease, and peripheral vascular disease.
Prolonged hyperglycemia leads to changes in the structure of the microscopic vessels that supply the retina of the eye, the glomeruli of the kidney, and both the peripheral and autonomic nerves. Although the pathology that leads to the development of these problems is not well understood, it is believed that there are probably multiple underlying etiologies.
Retinopathy
Persons with all types of diabetes are at risk for developing retinopathy. Persons with type 1 diabetes are more likely to develop proliferative retinopathy, the most devastating type of eye disease affecting people with diabetes. In this disorder, the small vessels of the retina become increasingly permeable and eventually rupture. The ruptured vessels are then replaced by new, very fragile blood vessels that rupture and bleed easily, causing leakage into the vitreous. This is further complicated by the abnormal attachment of these new vessels to the retina. Their presence greatly increases the risk for retinal detachment, furthering the progression to blindness.
Early proliferative retinopathy is usually asymptomatic but can be detected during a dilated eye exam. Early identification of proliferative retinopathy can result in treatment that may prevent or delay the onset of blindness. Standards of care for initial retinopathy screening differ for people with type 1 and type 2 diabetes [6]:
Type 1: Initial dilated and comprehensive eye examination within five years after the onset of diabetes
Type 2: Initial dilated and comprehensive eye examination shortly after the diagnosis of diabetes
Subsequent eye exams for both type 1 and type 2 should be repeated annually. Less frequent exams may be considered following one or more normal exams. More frequent exams are warranted when retinopathy is already present. Women with pre-existing diabetes who are pregnant or who are planning to become pregnant should have a comprehensive eye exam and be counseled on the risk for development or worsening of retinopathy [6]. Pregnant patients who develop retinopathy should be monitored every trimester and for one year postpartum as indicated by the degree of retinopathy [6]. Patient education principles related to the prevention and management of diabetic retinopathy are to inform patients that:
Keeping blood sugar levels as near to normal as possible can reduce the risk of developing retinopathy.
Having uncontrolled high blood pressure can increase the risk for diabetic retinopathy.
Early retinopathy can be present without any symptoms, but early detection and treatment can delay the progression of the disease.
Resources are available for individuals who have visual impairments.
Diabetic Kidney Disease
Diabetic kidney disease most commonly results from damage to the small blood vessels that supply the filtering components of the nephron, known as the glomeruli. Nephropathy occurs in approximately 20% to 40% of people with diabetes [6,38,39]. Risk factors for the development of diabetic nephropathy include hypertension, genetic predisposition, smoking, high dietary protein intake, and chronic high blood sugar. Results of the DCCT and the UKDPS have indicated that the risk for diabetic kidney disease can be reduced by 50% when near-normal blood glucose control is achieved and maintained [7,8,36].
Hypertension significantly accelerates the progression of diabetic nephropathy. Therefore, aggressive blood pressure management is indicated for all patients with diabetes. Angiotensin-converting enzyme (ACE) inhibitor drugs are commonly prescribed to diabetic patients for hypertension because they are effective blood pressure-lowering drugs with few side effects. In addition, ACE inhibitors are often prescribed to patients with diabetes even when they are not hypertensive because the drugs in this class have an independently protective effect on the kidneys, which can prevent the onset or progression of diabetic nephropathy. This means that the renal benefits of ACE inhibitors are above and beyond an effect attributable to blood pressure control alone. In addition to renal benefits, ACE inhibitors have been shown to reduce the risk for heart attack, stroke, and cardiovascular-related death in people with diabetes. Examples of ACE inhibitors include enalapril, fosinopril, lisinopril, and captopril. Another similar class of medication, angiotensin receptor blockers (ARBs), may be used in place of ACE inhibitors for delaying the progression of diabetic nephropathy [6]. A commonly used ARB is losartan.
Standards of care for the detection and prevention of diabetic nephropathy include a yearly screening for the presence of albumin in the urine [6]. This microalbuminuria test detects kidney damage in an earlier stage than the standard dipstick test for gross protein in the urine. Screening also includes measuring serum creatinine at least annually. If chronic kidney disease is present, serum creatinine is used to estimate glomerular filtration rate and stage of the disease [6]. Screening for albumin in the urine should occur up to four times per year, depending on the stage of the kidney disease [6].
Teaching principles related to the prevention and management of diabetic nephropathy include:
Informing patients that uncontrolled high blood pressure can accelerate the development and progression of nephropathy
Instructing patients with overt nephropathy that a high-protein diet may accelerate the progression of the disease
Informing patients that keeping blood glucose as near to normal as possible can reduce the risk of developing nephropathy
Educating patients that using an ACE inhibitor or ARB can delay the progression of nephropathy
Reviewing with patients the signs and symptoms of urinary tract infection and instructing them to seek prompt treatment when they occur
Neuropathy
As much as 50% of people with diabetes have some degree of nervous system damage [40]. Severe diabetic nerve disease is a major contributing factor in the development of problems leading to lower limb amputation. Results from the DCCT have provided evidence that maintaining good glycemic control reduces the risk for neuropathy by 60% [7]. This finding indicates that chronic hyperglycemia plays a significant role in the cause or promotion of nerve damage. All people with diabetes should be assessed for diabetic neuropathy starting at diagnosis of type 2 diabetes and five years after the diagnosis of type 1 diabetes and at least annually thereafter [6].
The most common type of neuropathy affecting persons with diabetes is sensory neuropathy. Distributed in a "stocking-glove" fashion, sensory neuropathy usually affects the feet and, to a lesser degree, the hands. Damage to the sensory nerves is often accompanied by motor nerve injury as well, leading to muscle atrophy and deformity of the affected extremities.
Signs and symptoms associated with sensory neuropathy are variable. In some cases, patients may experience pain, tingling, burning, or a pins-and-needles sensation in the hands and feet. Other symptoms include numbness, loss of feeling, or loss of temperature sensation in the affected areas. Treatment of sensory neuropathy is focused on attaining optimal control of blood glucose, managing pain, and protecting insensate feet from injury.
In addition to sensory nerve damage, people with diabetes are also at risk for various problems affecting the nervous supply to the internal and regulatory organs. Known as autonomic neuropathies, these conditions may occur in all types of diabetes and can affect any system in the body. These problems include cardiovascular impairment leading to orthostatic hypotension and "silent" myocardial ischemia. Gastrointestinal abnormalities include slowed digestion of food in the stomach (gastroparesis), nocturnal diarrhea, and fecal incontinence. Impaired insulin counter regulation may also occur, resulting in unawareness of hypoglycemia and "brittle" diabetes. Autonomic neuropathy affecting the genitourinary system can cause urinary retention and sexual dysfunction [6].
Patient teaching principles related to neuropathy include informing the patient that good glycemic control can prevent or delay the development of neuropathy and that neuropathic pain can sometimes be lessened when blood glucose control is improved. Medicine may be used for pain relief. There are many teaching principles associated with preventive care of the insensate foot. These will be discussed in detail in a later section of this course.
Macrovascular disease refers to changes in the moderate to large-sized arteries and veins that supply the heart, brain, and peripheral tissue. Ultimately, it is manifested by coronary heart disease (myocardial infarction), cerebral vascular disease (stroke), and peripheral artery disease, leading to vascular foot ulcers. Cardiovascular disease is the foremost cause of diabetes-related deaths and the largest contributor to the economic costs of diabetes, resulting in an estimated 20% to 49% of the total annual costs of treating type 2 diabetes [41]. Moreover, people with diabetes are prone to developing both coronary and cerebral vascular disease at an earlier age than people who do not have diabetes.
A number of factors contribute to the development of cardiovascular disease in the general population as well as in people with diabetes. These include hypertension, obesity, smoking, excess saturated fat and trans fat in the diet, and abnormal blood lipids (dyslipidemia). Diabetes is considered an independent risk factor for cardiovascular disease as well, predisposing the person to atherosclerotic macrovascular complications at an earlier age and with greater severity than the individual who does not have diabetes [6].
Because macrovascular disease associated with diabetes accounts for such high morbidity, mortality, and economic burden, preventive care efforts are of utmost importance. Preventive approaches include healthy diet, regular exercise, aggressive treatment of hypertension, smoking cessation, treatment of dyslipidemia, and maintenance of a healthy body weight. Blood pressure should be checked at every routine medical visit. For patients with diabetes and hypertension, blood pressure targets should be individualized. Those at higher cardiovascular risk (i.e., existing or 10-year ASCVD risk ≥15%), a blood pressure target of less than 130/80 mm Hg may be appropriate, if it can be safely attained. Individuals at lower risk of ASCVD (i.e., <15%) may be treated to a target of <140/90 mm Hg [6].
Patients with diabetes have an increased prevalence of lipid abnormalities, contributing to their high risk of ASCVD. A fasting lipid profile should be performed at least once a year and immediately before initiating statin therapy, if statin therapy is indicated [6]. Medication should be initiated for patients whose LDL cholesterol remains greater than 100 mg/dL after lifestyle modification has been instituted. Statins, such as simvastatin, are the preferred first line of therapy for LDL cholesterol lowering and cardioprotection (Table 3). The ADA recommends two statin dosing intensities for use in clinical practice (Table 4) [6]. Meta-analyses, including data from more than 18,000 patients with diabetes from 14 randomized trials of statin therapy, demonstrate a 9% proportional reduction in all-cause mortality and a 13% reduction in vascular mortality for each mmol/L reduction in LDL cholesterol [42].
ADA RECOMMENDATIONS FOR STATIN AND COMBINATION TREATMENT IN PEOPLE WITH DIABETES
| Age | Risk Factors | Statin Intensitya | |||
|---|---|---|---|---|---|
| Younger than 40 years | None | None | |||
| ASCVD risk factor(s)b | Moderate or high | ||||
| ASCVD | High | ||||
| 40 to 75 years | None | Moderate | |||
| ASCVD risk factorsb or ASCVD | High | ||||
| ACS and LDL cholesterol >70 mg/dL (1.3 mmol/L) in patients who cannot tolerate high-dose statins | Moderate plus ezetimibe | ||||
| Older than 75 years | None | Moderate | |||
| ASCVD risk factorsb | Moderate or high | ||||
| ASCVD | High | ||||
| ACS and LDL cholesterol >70 mg/dL (1.3 mmol/L) in patients who cannot tolerate high-dose statins | Moderate plus ezetimibe | ||||
| |||||
ADA RECOMMENDATIONS FOR HIGH-INTENSITY AND MODERATE-INTENSITY STATIN THERAPYa
| High-Intensity Therapyb | Moderate-Intensity Therapyb | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| ||||||||||
If targets are not reached on maximum doses of the statin medication, combination therapy using statins and other lipid-lowering drugs may be considered [6]. Principles of patient education related to macrovascular complications include:
Informing the patient of the risk of accelerated vascular disease in people with diabetes
Assisting the patient in identifying and addressing modifiable risk factors such as smoking, poor diet, sedentary lifestyle, hypertension, dyslipidemia, and obesity
Identifying strategies for reducing calories, trans fat, and saturated fat in meal planning
Instructing the patient about the benefits of a regular physical activity program to cardiovascular health
Educating the patient on the purpose and benefits of medication for blood pressure and lipid management
Telling the patient about community resources that can help him or her achieve a heart-healthy lifestyle (e.g., exercise programs, cooking classes, support groups)
Various skin problems occur more frequently in people with diabetes. Hyperglycemia contributes to dry skin and enhances the growth of certain types of skin infections, including boils, cellulitis, and lower extremity ulcers. Fungal infections often affect the areas of the genitalia, skin folds, and between the toes. In addition, infections usually increase blood glucose levels, thereby increasing insulin requirements. Education related to skin care should include the following:
Bathe daily with mild soap and water. Rinse well to remove residual soap.
Keep skin folds dry.
Maintain adequate nutrition and hydration.
Moisturize skin with an unscented, non-alcohol-based lubricant.
Use sunscreen and good sense to avoid sunburn.
Treat skin injuries promptly and monitor for healing.
Patients with poorly controlled diabetes have a greater susceptibility for the development of dental problems. The most serious of these, periodontal disease, can cause bone destruction and tooth loss. Signs and symptoms of periodontal disease include puffy, red gums that bleed easily, bad breath, and loose or decayed teeth. Patient teaching related to dental care should include instruction to:
Brush and floss teeth at least twice a day.
See a dentist at least every six months and inform the dentist of the diabetes diagnosis.
Seek prompt treatment for any oral problems.
Diabetes self-management education and support (DSMES) is considered an essential element of diabetes care. Furthermore, individuals who actively manage their own diabetes care have better outcomes than those who do not. For these reasons, an educational approach that facilitates informed decision making on the part of the patient is widely advocated [5,6].
Unfortunately, patients can encounter a variety of psychologic and emotional barriers when it comes to effectively managing their diabetes. These barriers include feelings of inadequacy about one's own abilities, unwillingness to make the necessary behavior changes, and ineffective coping strategies. The following sections of this course will discuss the empowerment approach to diabetes education and will cover methods for overcoming related barriers.
Patient empowerment is a widely supported approach to diabetes education. This model assumes that the patient is the person who will experience the consequences of diabetes and, therefore, is the one with primary rights and responsibilities regarding its management. Because the empowerment approach emphasizes the patient's role in decision making, education is aimed at providing information that the patient will need in order to manage his or her own care effectively. Healthcare providers who use the empowerment approach recognize that the ultimate responsibility for making changes that will affect health outcomes is with the patient. Therefore, the role of the healthcare provider is to assess patients' willingness to make changes and to help them set realistic goals.
According to the empowerment model, educators are most effective when they are able to recognize that they cannot and should not try to solve patients' problems for them. Instead, the role of the educator is to facilitate the patients' problem-solving skills and to support a decision-making process that is likely to benefit patients' health status. These skills can be supported by exploring, with the individual, the range of self-care options available and the consequences of each. Educators will discover that some patients are resistant to this type of exploration and should be prepared to accept their own limitations in their ability to effect change [43].
Self-efficacy refers to a person's sense of confidence in his or her own ability to perform a set of behaviors. Theoretically, people who are confident that they are able to do something with success are more likely to perform that behavior. In studies cited on self-efficacy in people with diabetes, it has been demonstrated that those who have a high degree of self-efficacy are more active in self-care, have a better sense of well-being, and have better blood glucose control [44].
Assessment of diabetes self-efficacy can be useful in targeting areas where the patient lacks confidence in the ability to carry out a self-care behavior. Specific self-efficacy questionnaires are sometimes used to make this assessment. One such questionnaire asks respondents how sure they are that they can perform specific diabetes-related behaviors. Sample statements from this type of questionnaire are presented in Table 5. The use of a specific questionnaire for self-efficacy is not always feasible. In that case, asking a few related questions as part of the general assessment can still make an expedient self-efficacy assessment. For example, patients can be asked how confident they feel (on a scale of 1 to 10) about their ability to manage diabetes on a day-to-day basis [44].
SAMPLE STATEMENTS THAT REFLECT SELF-EFFICACY IN PEOPLE WITH DIABETES
|
I feel sure I can:
|
Diabetes self-care requires substantial effort on the part of the patient, which can present a major challenge to those affected. People who develop diabetes are asked to make and maintain major lifestyle changes. These include regularly checking and interpreting blood glucose, planning and engaging in a regular physical activity regimen, and managing complex medication and nutritional regimens. The changes that cause the greatest difficulty tend to be lifestyle modifications, such as eating and physical activity habits, perhaps because they reflect embedded psychologic, social, and cultural influences.
Readiness to change refers to the hypothesis that people move through a series of stages as they give up unhealthy behaviors and adopt health-enhancing behaviors. The Stages of Change Model has been widely used in smoking cessation as well as in DSMES. The researchers identified six stages that people go through as they attempt lifestyle changes. These stages range from precontemplation, during which the patient does not intend to change within the next six months, to maintenance, when healthy behaviors have been practiced for greater than six months. For each stage of change, certain interventions on the part of the healthcare provider are recommended. By employing these interventions, the healthcare provider is able to "meet" the patient within his or her own particular stage of change at a given time [45].
In the precontemplation stage of change, the person is not thinking about changing. Precontemplation represents a time of resistance to change and may be accompanied by denial that there is a problem. During this stage, the patient may actively resist change and avoid responsibility. To the healthcare provider, this patient may seem defensive and be labeled as "noncompliant." Recommended interventions at this stage include helping the patient identify his or her beliefs, feelings, and attitudes in a nonjudgmental way. This can be done by employing reflective listening and empathy. In order to make the transition to the next stage, patients in the precontemplation stage must choose to accept ownership of the problem. At this stage, objective information should be provided based on caring and concern, rather than to prove the patient wrong about his or her feelings.
During the contemplation stage, the patient is less resistant to change, although he or she is still undecided and may be procrastinating. During this time, patients may tentatively seek information as they assess the benefits that the change will bring. Although the prospect of change within the next six months is characteristic, it is common for some patients to remain in this stage for an extended period of time. The role of the healthcare provider at this time is to help increase self-efficacy and to support the patient's efforts in seeking information. Specific interventions include reflective listening, providing empathic feedback, and offering information and resources when appropriate.
The third stage of change is preparation. At this time, patients are ready to take action in the next 30 days and may begin to visualize their future selves and prepare for the change. For example, the patient who wants to lose weight may begin removing unhealthy foods from the home. Strategies for this stage are to formulate an action plan that includes setting goals and enhancing self-efficacy. The role of the healthcare provider at this stage is to provide encouragement, help build confidence, and manage anxiety.
In the action stage, the patient demonstrates a strong commitment to change by modifying his or her behaviors and environment. This is the time when the person actually tries out the new behaviors. Support from others during this time is very important. The role of the healthcare provider is to strengthen the patient's commitment to change.
Maintenance is the stage in which patients have maintained desired behaviors for more than six months. During this time, the healthcare provider's role is to support continued commitment on the part of the patient and to continue to support self-efficacy.
Relapse may occur at any stage of change and can result in a return to any of the earlier stages. Relapse should not be viewed as failure but as part of the ongoing process of growth. Recycling is the process of learning from relapse. When relapse has occurred, the healthcare provider should not demonstrate feelings of disappointment or chagrin. Instead, the healthcare provider's role is to be sensitive and help the patient explore the triggers that related to the relapse. This will help the individual recycle previously made gains and return to a higher level of self-care.
Readiness to change can vary for different behaviors in the same individual. Therefore, each diabetes self-care behavior should be addressed individually with relation to stage of change. For example, the patient may be in the maintenance stage with regard to administering insulin, demonstrating full assimilation of this behavior into his or her lifestyle. At the same time, the patient may be in the precontemplation stage with regard to diet, indicating resistance to adopting more healthy dietary choices.
Readiness to change can be assessed by asking the patient questions about each specific behavior. Stages of change can be identified with reference to the time period in which the patient is operating with regard to a given behavior. For example, in assessing the patient's readiness to perform self-monitoring of blood glucose (SMBG), the following questions may be asked:
"Do you check your own blood sugar?"
If yes: "How long have you been doing this?" (More than six months = Maintenance stage) (Less than six months = Action stage)
If no: "Are you planning to start doing this at some time in the future?" (No = Precontemplation stage)
If yes: "Are you planning to start doing this in the next month?" (Yes = Preparation stage)
If no: "Are you planning to do this in the next six months?" (Yes = Contemplation stage) (No = Precontemplation stage)
Motivational interviewing is used in a variety of healthcare settings to facilitate behavior change. This approach uses therapeutic communication to help people explore the discrepancy between how things are versus how one wishes they would be. This allows patients to examine their own reasons for change and to search for their own solutions. Key concepts of motivational interviewing include [46]:
Facilitating self-efficacy
Exploring the patient's ambivalence about change
Eliciting "change talk"
"Rolling with resistance"
Facilitating self-efficacy acknowledges that the patient has a right not to change. The provider does not impose his or her beliefs or prescribe a particular action. Instead, the provider helps the patient identify his or her own values. While the patient sets goals, the provider helps direct him or her toward realistic options and offers reassurance that they can be met.
Exploring ambivalence helps patients to see that there is a difference in where they are and where they would like to be. For example, a question to help patients explore ambivalence about changing eating habits would be: "I heard you say that you do not like healthy eating, but you came to our healthy eating class. Can you tell me more about what brought you to the class?" This type of questioning can help patients uncover reasons they feel change would benefit them.
Eliciting "change talk" involves looking for statements that signify the patient is no longer happy with the status quo. Mirroring these statements back to the patient reinforces the perceived benefits of behavior change. In order to elicit change talk, listen for "I wish" or "I want" statements and explore them further.
"Rolling with resistance" maintains the patient-centered encounter, facilitates self-efficacy, and demonstrates empathy. Instead of fighting or arguing a point, the practitioner should listen and discuss patients' responses. Resistance by the patient can be an opportunity to elicit change talk.
Coping can be described as the manner in which a person responds to a stressful situation. Ineffective coping mechanisms include apathy, denial, and avoidance behaviors. Other self-destructive coping mechanisms include overeating, smoking, and substance abuse. For the person with diabetes, poor coping skills may be self-destructive, resulting in chronically elevated blood glucose levels and creating increased risk for the development of long-term complications. It has been found that practicing appropriate coping skills can lead to better blood glucose control in the person with diabetes.
Helping the patient identify his or her own beliefs about having diabetes is an important step toward facilitating the development of coping skills. Because beliefs are usually reflected in the thoughts that a person has, healthcare providers can help the patient identify the thoughts that motivate self-care behavior. For example, negative thoughts tend to trigger behavior that is not constructive. The patient may think, and therefore believe, that "Checking blood sugar is useless." This negative thought process can result in failure to monitor blood glucose levels adequately. On the other hand, a positive thought, such as "Checking my blood sugar helps me stay well," would be more likely to result in constructive health-enhancing behavior. Providing the patient with reflective feedback about his or her beliefs may help convert self-limiting thoughts into constructive thoughts. When the patient with diabetes is able to reflect upon his or her beliefs about having the disease, he or she may be able to identify how those thoughts affect health-related behaviors and, ultimately, health status.
Encouraging patients to set concrete and realistic goals can also improve the ability to cope with diabetes. Effective goal setting is based upon the achievements desired by the patient, not what the healthcare provider or others think should be achieved. Asking him or her to write down or describe the things he or she would like to change can identify the patient's goals. Priorities can then be set by asking the patient to decide which one or two of these changes are the most important. The patient should be encouraged to start small and be realistic when setting goals. Importantly, goals focused on behavior are better than goals focused on a specific outcome. For example, a goal to check blood glucose four times a day is better than a goal that specifies a numeric blood glucose result to be attained. Because blood glucose results can be influenced by variables that may be outside the control of the patient, the patient would be less likely to meet this kind of goal. However, when the focus of the goal is on behavior that the patient can control, meeting goals becomes more realistic. Another strategy for successful goal setting is to advise the patient to avoid perfectionism. For example, a goal like, "I will never cheat on my diet" is probably not realistic for most people. A better goal would be, "I will not deviate from my meal plan more than once a week for the next month" [43].
People with strong psychosocial support seem better able to cope with the demands of having diabetes. Support systems can include family, friends, significant others, caregivers, professionals, and other members of the diabetes community. For patients who do not have a readily identifiable support system, effort should be made to help them develop one. Even for those who have a strong social network, fellowship with other people who have diabetes can be valuable. Peer fellowship often evolves from involvement in diabetes support groups, such as those sponsored by local chapters of the ADA and through diabetes education classes.
Patient Y is an African American woman, 62 years of age, who was diagnosed with type 2 diabetes 16 years ago. Her history includes hypertension, which is currently well controlled on medication, body weight 30 lbs above ideal, clinical signs of early renal failure, cardiovascular disease, and early-stage retinopathy. She reports that, "My blood sugar never has been too good, and I don't think it ever will be. Lately it's gotten worse." In your assessment, you note that Patient Y's blood glucose has ranged from 43–383 mg/dL over the previous few months.
Patient Y tells you that she feels confident in her ability to monitor her blood glucose and administer her insulin. She demonstrates that she is able to do this. However, she is concerned about her widely fluctuating blood glucose levels. She says, "Sometimes my sugar's too high, and I don't know what I did to make it high. Other times, it's low, and I get really scared that I'll end up in a coma." She goes on to report that if her blood sugar is less than 100 mg/dL, she will routinely treat herself with a tablespoon of sugar added to 10–12 ounces of orange juice.
Patient Y indicates that she has a good understanding of basic principles of meal planning and that her family is generally supportive of her dietary needs. Her dietary recall reveals that she makes many appropriate food choices when she eats but that her eating pattern is inconsistent. She skips or delays meals in some cases and eats large amounts at other times. In apparent frustration, she states, "It doesn't seem to matter whether I eat right or not."
Patient Y's statements reflect a low level of self-efficacy in some important areas of diabetes self-management. For example, she does not believe that she can achieve good glycemic control, and she lacks confidence in her ability to manage the dietary aspects of her own care. The basis for a therapeutic and empowering relationship with Patient Y will begin when these feelings of frustration and helplessness are acknowledged. You can do this by asking open-ended questions that focus on her feelings. For example, you can ask her, "What is the hardest thing for you right now about dealing with your diabetes?"
If you learn that Patient Y's greatest concern revolves around her fear of experiencing serious hypoglycemia, it will then be an important part of your teaching plan to include instruction on hypoglycemia prevention and management. As you probe further, you discover that the fear Patient Y has surrounding hypoglycemia drives her to take excessive amounts of sugar when she perceives that her blood glucose is too low. You find that, in many cases, she takes large amounts of sugar based upon subjective feelings of "being low," without checking her blood sugar first. You also realize that Patient Y's "comfort zone" for low blood glucose, anything less than 100 mg/dL, is actually quite a bit higher than standard values of 60–70 mg/dL for hypoglycemia. You can see that frequently taking large amounts of sugar seems to result in blood glucose values that rebound to very high levels. This is probably a major contributor to her overall pattern of blood glucose fluctuations. Furthermore, you can presume that Patient Y's irregular pattern of eating is another factor in her erratic glucose pattern, probably accounting for the episodes of true hypoglycemia that she has had.
It is important to teach Patient Y that she can safely prevent and manage hypoglycemia in a way that will help her achieve better overall blood glucose control. In order to gain her trust, the patient's fear of hypoglycemia should be validated by acknowledging that it can be a serious side effect of insulin. You want her to know that keeping her safe is your priority as well.
Once trust has been established, you will want to consider Patient Y's readiness to change the behaviors that seem to be causing poor glycemic control. Following is a scenario of how you might accomplish this:
Nurse: "It sounds like having a serious episode of low blood sugar really worries you."
Patient Y: "I've been to the ER with it before, and they told me you can die if the sugar goes too low."
Nurse: "I can understand why you are afraid of having a hypoglycemic reaction. It certainly can lead to serious problems if not treated. Fortunately, most people can either prevent it or treat it in the early stages. I would like to talk to you about some ways of preventing and treating low blood sugar. There are ways that you should be able to prevent low blood sugar without causing so many highs in between."
Patient Y: "That would be good."
Nurse: "It would involve some changes on your part, including what you do when your blood sugar is low. It would involve not taking quite so much sugar so often. Is this something you'd be interested in hearing about?"
Patient Y: "I can think about it. But I don't want to do anything that will let my blood sugar go too low."
By indicating that she will allow you to provide tentative information, Patient Y demonstrates that she is in the contemplation stage of behavioral change. Your role, therefore, is to offer information, provide empathic feedback, and listen reflectively.
Inform the patient of the standard treatment for hypoglycemia, which is to take 15 grams of fast-acting carbohydrate for blood glucose less than 70 mg/dL. In addition, help Patient Y understand the relationship that her irregular pattern of eating may be having on fluctuations in blood glucose. Instruct her that hypoglycemia can usually be avoided by eating a balance of food types every four to five hours throughout the day.
First, acknowledge and validate the patient's fears. Then, in a nonjudgmental way, you can describe to Patient Y how her behavior seems to contribute to the wide fluctuations in blood glucose levels. You could say: "It would probably be better if you checked your blood sugar to see if it is truly low before eating sugar. Then you will not be causing your blood sugar to rise if it is not necessary. In addition, I don't think you need to take as much sugar as you have been for levels less than 100 mg/dL. It is recommended that you only need to treat for low blood sugar if it is less than 70 mg/dL. Even then, you can probably raise your blood sugar with a smaller amount of sugar, like just the orange juice without the added sugar."
Serve as a mirror for her thoughts and beliefs. For example, you may respond to her ambivalence by saying, "Even though you haven't said you want to try these things right now, I get the feeling you might decide to try it at some point. I'll leave you some written information that you can keep on hand."
As you continue to work with Patient Y, you may discover other areas where she needs further diabetes education. You can continue to help her make appropriate decisions about her own care through an empowering approach. Just as you did with the issue of hypoglycemia, you should continue to acknowledge the patient's priorities, assess her levels of self-efficacy, and address her readiness to change behavior. Proper assessment of these areas will allow for the provision of appropriate and effective interventions.
DSMES and diabetes self-management support (DSMS) for patients with diabetes are defined as [5,6]:
…the ongoing processes of facilitating the knowledge, skill, and ability necessary for diabetes self-care. These processes incorporate the needs, goals, and life experiences of the person with diabetes. The overall objectives of DSME and DSMS are to support well-informed decision making, self-care behaviors, problem-solving, and active collaboration with the healthcare team to improve clinical outcomes, health status, and quality of life in a cost-effective manner.
In general, the goal of diabetes self-management skills training programs is to enable the patient to become the most active participant in his or her own care.
Several studies have demonstrated that self-management training improves self-care behavior, clinical outcomes, and the quality of life for patients with diabetes. Diabetes education and support is also associated with better use of primary and preventive services and lower rates of hospitalization [6]. Further, it has been found that patients who have diabetes education have lower average healthcare costs than those who do not [6,47]. Although experts and research findings agree that DSMES is essential, the U.S. Department of Health and Human Services reported that in 2019 only 55.1% of people with diabetes have ever received any formal education on how to manage their condition. This was indicated as "little or no detectable change" according to Healthy People 2030 objectives [48]. In 2020, a total of 2,158 sites were delivering DSMES services across the United States, with approximately 1 million people participating in the programs [49]. One barrier to diabetes education is access. Although DSMES are offered in 56% of counties across the United States, 62% of rural counties have limited access to these services [49]. Providers of DSMES can help address the lack of access by [5]:
Clarifying the specific population to be served by understanding the community, service area, or regional demographics
Determining that population's DSME needs and identifying resources outside the provider's practice that can assist in ongoing support
Identifying access issues (e.g., socioeconomic or cultural factors, lack of encouragement from other healthcare providers to seek education) and working to overcome them
National standards have been developed for the establishment and maintenance of quality diabetes self-management programs [5,6]. This curriculum includes, but is not limited to, the following components (specific components to be delivered should be based upon an individual needs assessment):
Diabetes disease process and treatment options
Nutrition
Exercise and activity
Medications
Monitoring of blood glucose and use of results
Prevention and treatment of acute complications
Prevention and treatment of chronic complications
Psychosocial adjustment
Developing personal strategies to promote health and behavior change
Additionally, DSMES and DSMS programs are appropriate for individuals with prediabetes as they can help develop and maintain behaviors to prevent or delay the onset of diabetes [5].
While self-management education does provide a foundation for coping with diabetes, knowledge of facts and skills alone is seldom effective in improving diabetes outcomes. Therefore, the didactic elements of a program should be supplemented with additional interventions that support patient empowerment such as goal setting, problem solving, behavioral change strategies, stress management, and other psychosocial issues.
In general, healthcare providers involved with teaching diabetes self-care will encounter vast differences in patient need. For example, a nurse working in a physician's office may be asked to counsel a newly diagnosed patient about the diabetes disease process and the principles of meal planning as therapy. A hospital nurse's orders might be to teach an acutely ill patient, who has previously been controlled on oral medicines, how to draw and inject insulin at home following discharge. Meanwhile, a home health nurse is often asked to see a patient with long-standing diabetes for the purpose of providing a blood glucose meter and assessing the patient's home management of diabetes. Each of these situations requires a different focus for education. Indeed, it may not be feasible, or even advisable, to deliver a complete course in diabetes self-management to all patients. Therefore, it is necessary to assess the learning needs of the individual patient within the context of the teaching situation.
A needs assessment is a systematic way to gather information about experiences, beliefs, and behaviors that the patient has with regard to diabetes self-care. Information gleaned from the needs assessment can then be utilized to develop a teaching plan that meets the individual needs and priorities of the patient. For the nurse, a needs assessment streamlines the teaching process by focusing on the unique needs of the individual. For the patient, the needs assessment is empowering because it addresses his or her perspective of educational need. Thus, an important area to be addressed in a needs assessment is what the patient perceives as the primary learning need. Other areas that should be assessed include current understanding of self-management practices, self-management behaviors that are currently practiced, and relevant psychosocial/cultural factors. Sample questions from a diabetes needs assessment are listed in Table 6.
SAMPLE DIABETES NEEDS ASSESSMENT ITEMS
|
An effective approach to teaching diabetes self-care in adult settings is to employ various principles of adult learning theory. An important principle of adult learning theory is that adults tend to be self-directed learners who feel a need to learn. Asking the patient what he or she feels addresses this principle of adult learning and is the most important issue during the needs assessment.
Focus Teaching on the Patient's Perceived Problems
Determine what the patient feels he or she needs to know and what the perceived problems are. The adult learner will be more likely to acquire new knowledge and skills when teaching is directed toward specific problems rather than toward a comprehensive set of material.
Find Out What the Patient Already Knows
Adults tend to learn better when teaching incorporates prior knowledge and past experiences. When teaching a problem-solving process, for example, ask the patient how he or she has dealt with a similar situation in the past. Build upon this experience to teach new material.
Keep the Patient Active in the Learning Process
Provide opportunities for interaction, questions, and sharing. Teaching is apt to be more effective when the patient's own life experiences can be incorporated into the lesson.
Allow for Self-Directed Learning
Enhance the learner's sense of autonomy by letting him or her make choices about what is being taught. For example, you can allow the patient to choose the mode of learning or the amount of time spent on a particular topic.
Give the Patient a Reason to Learn
Adult learners generally must perceive the benefits of what is being taught. Address this by giving the patient a brief rationale for the content that you are presenting, focusing on the benefits that can result from learning.
The goals of diabetes management are most likely to be met when the patient is able to maintain blood glucose levels as near to normal as possible. (Normal fasting plasma is 70–99 mg/dL.) While "tight control" is desirable for many patients, blood glucose target ranges are determined individually for each patient, taking into account the patient's age, general health status, risk for undetected hypoglycemia, and personal motivation. In general, the goals of treatment for diabetes are to:
Reduce symptoms and promote well-being
Prevent acute complications such as hypoglycemia, HHS, and ketoacidosis
Curtail the onset and progression of chronic complications such as blindness, renal failure, and cardiovascular disease
For some patients with type 2 diabetes, a regimen of regular physical activity and proper nutritional management, along with maintenance of a desirable weight, will be sufficient to attain an optimal level of blood glucose control. For the majority, however, pharmacologic treatment will be necessary. In any case, regular blood glucose monitoring and attention to educational and psychosocial needs are essential interventions. People with diabetes should be provided with blood glucose monitoring devices as indicated by their circumstances, preferences, and treatment. People using continuous glucose monitoring devices should have access to blood glucose monitoring at all times [6].
Results of blood glucose testing are used to assess the effectiveness of therapy and to guide adjustments in the diet, medications, and activity levels of people with diabetes. SMBG is recommended for all patients who use insulin, for many who use oral glucose-lowering medications, and for those who are not achieving glycemic goals [6]. Consistent, uninterrupted access to glucose monitoring devices is associated with improved patient outcomes [6]. Often, nurses are in a position to instruct patients about SMBG in the home, in outpatient settings, and at the bedside in hospitals and skilled nursing facilities.
In 2008, the International Diabetes Federation (IDF) and the SMBG International Working Group convened a workshop to address the use of SMBG in individuals with type 2 diabetes not treated with insulin. In 2025, they published updated recommendations on the standards of diabetes care as they relate to SMBG. The recommendations are based on two levels of care and prevention: optimal care and basic care (Table 7). Optimal care is evidence-based care that would ideally be universally achievable. Basic care is that which is provided in healthcare settings with limited resources [50].
INTERNATIONAL DIABETES FEDERATION RECOMMENDATIONS FOR SELF-MONITORING OF BLOOD GLUCOSE (SMBG)
| Level of Care | Recommended Approach | |||
|---|---|---|---|---|
| Optimal care |
| |||
| Basic care |
|
SMBG is recommended in insulin-treated T2DM but may be useful in other situations. SMBG use (intensity and frequency) should be structured and individualized [50].
A major benefit of SMBG is that it provides feedback about how well treatment goals are being met. By keeping blood glucose levels as near normal as possible over time, people with diabetes can reduce their risk for acute and chronic complications. SMBG can help prevent hypoglycemia and provide information relevant to adjusting food intake, activity level, and medication [6]. Several studies have shown that SMBG is associated with decreased morbidity and mortality in individuals with type 2 diabetes [51,52,53].
SMBG provides the patient with immediate feedback on how daily choices affect blood glucose levels, giving reliable information for problem solving and decision making [6,50]. For example, SMBG may allow patients to determine the effect that particular foods or groups of foods have on blood glucose. This is especially useful for the patient who may occasionally want to eat a food high in sugar. SMBG can provide feedback indicating whether the sugar has caused a rapid and excessively high rise in blood glucose.
SMBG is also beneficial in that it can be utilized to monitor how psychologic and physical stressors influence glycemic responses [50]. Correlating SMBG results with the presence of stressors can help the patient manage them for better glycemic control.
As stated, individuals with diabetes should be provided with blood glucose monitoring devices as indicated by their circumstances, preferences, and treatment. There is no "one-size-fits-all" approach. Any device used for diabetes management works best when accompanied by education, training, and follow-up [6].
Although the benefits of SMBG are substantial, some patients may be reluctant or unable to perform this task. However, the benefits of SMBG greatly outweigh the disadvantages, and healthcare providers should be prepared to help patients overcome these barriers. Specifically, lower neighborhood socioeconomic status, older age, fewer HbA1c tests, and fewer physician visits were associated with lower rates of SMBG [51]. Black race, high glycemic level, obesity, and a lesser number of comorbidities were also identified as risk factors for less frequent monitoring.
For some with diabetes, costs associated with blood glucose testing can create a significant barrier to testing [50]. When patients have to pay out-of-pocket expenses for medical supplies, financial barriers have been shown to reduce the use of SMBG. It is important, therefore, to weigh the potential benefits of SMBG against its cost, especially when the expenditures for SMBG may come at the expense of other treatment modalities (e.g., medication) [50]. Fortunately, this changed for Medicare-eligible patients in 1998, when the cost of tests strips, lancets, and meters became covered expenses for people with type 1 and type 2 diabetes.
Individuals may not want to check their blood glucose on a regular basis because they perceive it to be an inconvenience that encroaches on their lifestyle. Healthcare providers might be able to help such patients overcome this barrier by providing information about how improved blood glucose control can result in feeling better on a day-to-day basis. Further information may be provided regarding how glycemic control reduces the risk for long-term complications, making patients more able to lead productive lives. The perception that SMBG is inconvenient may also be offset if patients are shown how this procedure can allow for greater flexibility in meal planning. By monitoring the effects of various foods and the timing of meals on blood glucose, patients can have more choices with regard to eating [6,50]. Patients who find regular blood glucose monitoring bothersome may be interested in meters that are smaller, faster, and require fewer steps during testing. Some meters allow for "alternate site" testing, in which the patient can collect a blood sample from the forearm or the thenar aspect of the palm, where fewer nerve endings make the procedure less painful. Additionally, the IDF/SMBG Working Group has suggested possible regimens that may be individualized to address the specific needs of each person with diabetes [50].
The task of SMBG may be too complex for some patients, especially those with sensory or cognitive deficits. Careful selection of the type of meter that the patient will use can overcome these limitations in some cases. For example, meters that do not require fine precision with regard to where the blood drop is placed may be most appropriate for patients with visual or motor deficits. "Talking" blood glucose meters are available for people who are visually impaired. For some patients, it will be necessary to teach family or caregivers how to monitor blood glucose. Patients assume their glucose monitor is accurate because it has been cleared by the FDA. However, there is substantial variation in the accuracy of widely used blood glucose monitoring systems, and few studies have compared meters in a head-to-head manner [6]. Inaccurate blood glucose monitoring systems pose a public health problem because their readings serve as a basis for treatment decisions [54]. The Diabetes Technology Society Blood Glucose Monitoring System Surveillance Program provides information on the performance of devices used for blood glucose monitoring (https://www.diabetestechnology.org/surveillance).
The possibility of user error can be another disadvantage of SMBG. Patients with functional limitations may not be able to get accurate results because they do not have the physical ability to perform the test correctly. Other patients may be careless with their technique due to psychologic indifference, a lack of appreciation for the significance of results, or other behavioral factors. User error may be mitigated by observing the patient's technique at the start of care and following up with periodic checks thereafter. By observing the patient's technique on a regular basis, the message is sent that accurate SMBG results are important and worthy of the time it takes. Similarly, the technique demonstrated by caregivers and family members who assist with monitoring should be observed and evaluated as well [6].
Patients vary in terms of their comfort with technology, and the complexity and rapid change of the diabetes technology landscape can be an additional barrier to patient and provider implementation. Patients with more education regarding device use have better outcomes. The need for additional education should be periodically assessed, particularly if outcomes are not being met [6].
The frequency and timing of SMBG are dictated by the needs and goals of the individual patient [6,50]. Some meters provide advice to the user in real time when monitoring glucose levels, whereas others can be used as part of integrated health platforms [6]. For a patient using multiple daily insulin injections or the insulin pump, testing should be done at least three times per day but may need to be done as often as 6 to 10 times daily [6]. Patients on intensive insulin regimens (i.e., multiple-dose or insulin pump therapy) should consider SMBG prior to meals and snacks, occasionally postprandially, at bedtime, prior to exercise, when low blood glucose is suspected, and prior to critical tasks (e.g., driving) [6]. SMBG is also important for patients using oral hypoglycemic medications to monitor and prevent asymptomatic hypoglycemia. The optimal frequency of testing for patients with type 2 diabetes not using insulin is unclear; however, more frequent SMBG (e.g., fasting, before/after meals) may be helpful, as increased frequency has been shown to be inversely correlated with glycemic control [6]. For individuals with non-insulin-treated diabetes, it may be beneficial to perform "focused" SMBG over short periods of time (e.g., five to seven days), both initially and periodically, during the course of their disease, to obtain data to identify glucose patterns that reflect daily glycemic control. The intensity and frequency of SMBG should be individualized to address each individual's specific educational, behavioral, and clinical requirements, specific needs, and goals [50].
As stated, it is critical that the patient and healthcare provider be willing and able to use SMBG appropriately and effectively. The patient should possess the knowledge and skills to accurately perform SMBG and interpret the results to adjust food intake, exercise, or pharmacologic therapy to achieve specific goals [6]. The healthcare provider should ensure that the patient is competent to carry out SMBG on an ongoing basis, and the provider should have the knowledge, skills, and willingness to consistently review results to make necessary adjustments to the treatment plan [50]. The frequency of SMBG should be re-evaluated at each routine visit to ensure its effective use [6].
Guidelines for teaching patients how to use a blood glucose meter include:
Use universal precautions to prevent the transmission of bloodborne pathogens.
Without pricking finger, first demonstrate operation of equipment, such as turning meter on, loading lancing device, and cocking and ejecting lancing device.
Have patient simulate procedure prior to actually pricking finger. May use control solution to do this.
Ask the patient to perform a return demonstration after initially demonstrating the procedure.
Teach about meter coding, control testing, and using the logbook after the patient has learned how to perform the testing procedure.
Explain how to dispose of lancets in an appropriate sharps container.
Evaluate the patient's technique at every opportunity.
Additionally, it is helpful to instruct the patient to obtain blood by pricking the side of his or her fingertip. This avoids puncturing the more sensitive areas of greater innervation.
Blood glucose target ranges should be individualized for the patient. While the overwhelming benefits of tight glycemic control have been demonstrated, this is not necessarily the optimal goal for every patient. For example, an elderly patient living alone may have a higher target range in order to reduce the risk of hypoglycemia. In this case, the risk for an episode of undetected and unassisted hypoglycemia outweighs the benefits of warding off long-term complications.
Although the importance of individualized goals should be emphasized, the following target blood glucose levels can generally be recommended for most adult patients with diabetes [55]:
Before meals: 80–130 mg/dL (5.0–7.2 mmol/L)
After meals: Less than 180 mg/dL (less than 10.0 mmol/L)
When discussing blood glucose monitoring, it is helpful to consider the "four cornerstones" of diabetes management. Any of these four factors can be responsible for influencing blood glucose control at any given time for a particular patient. They are:
Meal planning
Medications (including oral medications and insulin)
Activity levels
Stress management (including psychologic and physical stressors)
If blood glucose results are lower or higher than desired, the patient should be directed to analyze each of these variables to determine which of them has most likely affected the blood glucose at that particular point in time. Following is a list of questions that patients should ask themselves to determine which of the four cornerstones of management is most likely responsible for current blood glucose results:
"Have I exercised more than usual?" (This is more likely to cause low blood sugar.)
"Have I exercised less than usual?" (This is more likely to cause high blood sugar.)
"What medications did I take for diabetes?"
"Did I take the right dose?"
"Did I take it at the right time?"
"Did I inject the right type of insulin?"
"What site did I use?"
"Are any of my medications expired and have they been properly stored?"
"What other medications did I take?" (Sugar-containing cough syrups, thiazide diuretics, and corticosteroids are examples of medications that can cause hyperglycemia.)
"Am I ill?" (Signs and symptoms of infection are most significant.)
"Am I going through a great deal of emotional turmoil right now?"
Analyzing the results of blood glucose testing should also take into consideration multiple factors related to the working order and cleanliness of the meter. This would also include verifying the patient's blood glucose testing technique and the quality of the test strips being used.
Patient J is a man, 60 years of age, with a history of type 2 diabetes. He was brought to the emergency department after his neighbor found him at home with confusion, lethargy, right-side weakness, and slurred speech. Medical exam and work up in the emergency department revealed that Patient J was severely dehydrated and that his blood glucose was 860 mg/dL. He was diagnosed with HHS, an acute complication of type 2 diabetes. He was admitted to the medical unit on an insulin drip and for intravenous fluid and electrolyte replacement.
After Patient J's blood glucose and electrolytes returned to normal levels, his mental status cleared and he was free of any neurologic manifestations. While in the hospital, he was seen by the diabetes educator. He received instruction on diet, insulin administration, and blood glucose monitoring. His discharge plan was to return home on insulin injections with follow-up and teaching by a home healthcare nurse.
Discussion
Patient J's home healthcare nurse will play a crucial role in helping him prevent another episode of HHS and other serious problems associated with poorly controlled diabetes. One of the most important aspects of his care plan will be to teach and instruct him in SMBG. As an essential component of diabetes care, SMBG will enable Patient J and his healthcare team to monitor blood glucose levels and influential factors. Good glycemic control will not only help this patient avoid acute problems like HHS, it should also help him feel better on a daily basis. Good control can also help the patient avoid the devastating long-term complications of diabetes, such as blindness, renal failure, and cardiovascular disease.
Before developing a teaching plan for Patient J, a needs assessment to determine what he already knows about diabetes self-care should be performed. This should include areas of care such as nutrition, insulin administration, and blood glucose monitoring. The needs assessment in this case indicates that the patient is unable to correctly perform SMBG independently. He is assessed as being ready to learn this procedure because he clearly indicates that he is willing to incorporate this behavior into his daily life.
In order to most effectively teach Patient J this procedure, the principles of adult learning should be incorporated into the teaching strategy. Begin by finding out what he perceives as problems or barriers to successfully performing SMBG. This will empower Patient J by engaging him in the learning process. Furthermore, his interest may be stimulated by providing a brief rationale for what is being taught, including the benefits of SMBG. Continue applying principles of adult learning on an ongoing basis by keeping Patient J active in the learning process and providing him plenty of opportunity to interact and ask questions.
After teaching Patient J how and why to monitor his blood glucose, the nurse will ascertain his ability to perform this procedure by asking for a return demonstration using control solution. Once this is completed, finger sticking and bloodletting techniques may be covered, ensuring that he can perform these properly.
After the procedures have been reviewed, it is important to ensure that Patient J has a thorough understanding of how to interpret his blood glucose results. The patient should have an understanding of how to compare his food intake, activity pattern, medications, and daily stress level to blood glucose results using a diary. When he learns how these factors influence blood glucose, he will be better able to achieve and maintain glycemic control while avoiding problems associated with diabetes.
Continuous glucose monitoring allows patients with diabetes to receive immediate feedback on estimated blood glucose levels at any moment. A sensor is inserted under the skin to measure glucose levels in the interstitial fluid, and this information is transmitted to a receiving device, providing a continuous record of estimated blood glucose and the direction and rate of change. Patients engaged in continuous glucose monitoring are still required to complete fingerstick blood tests two to four times per day to calibrate the monitor.
Initially, continuous glucose monitoring was developed so physicians could receive reports, which were then shared with the patient. More recently, continuous glucose monitoring is being used more actively by patients as part of a SMBG program. In type 2 diabetes, continuous glucose monitoring can help target postprandial glucose, the major contributor to HbA1c [6]. A 2016 study demonstrated that continuous glucose monitoring can provide immediate and valuable feedback about the effect of food intake and activity level on glucose levels [56].
In 2015, the U.S. Food and Drug Administration (FDA) approved the first system capable of real-time sharing of data from continuous glucose monitoring with others via telephone [57]. The G4 Platinum (Pediatric) Continuous Glucose Monitoring System was developed for use in children with type 1 diabetes. In 2017, the FDA approved the first continuous glucose monitoring system for adults that does not require blood sample calibration, thus reducing the need for fingerstick testing [58]. The FreeStyle Libre Flash Glucose Monitoring System uses a small sensor wire inserted beneath the skin's surface to continuously measure and monitor glucose levels. In 2020, the FDA approved the next-generation FreeStyle Libre 2, an integrated continuous glucose monitoring system with optional real-time alarms that measure glucose levels every minute [6,59]. In 2022, Abbott introduced the FreeStyle Libre 3. This newest iteration sends data straight to the user's smartphone [60]. In 2018, the FDA approved Guardian Connect for use in persons 14 years of age and older with type 1 or type 2 diabetes. The system works with sensors worn on the upper arm or abdomen and predicts where the patient's glucose levels are heading, then alerts the person 10 minutes to one hour before a high or low level occurs [61]. The Guardian Connect requires two fingersticks per day for calibration. In 2018, the FDA also approved marketing of the Dexcom G6 integrated continuous glucose monitoring system (an upgrade of the Dexcom G5) for determining blood glucose levels in children 2 years of age and older as well as in adults. This is the first system permitted by the agency to be used as part of an integrated system with other compatible medical devices and electronic interfaces (e.g., automated insulin dosing systems, insulin pumps) used for diabetes management [62]. The G6 requires no fingersticks for calibration. The FreeStyle Libre and Dexcom G6 have been designated as integrated continuous glucose monitoring devices, meaning they meet a higher standard established by the FDA and can be reliably integrated with other digitally connected devices, including automated insulin-dosing systems [6].
In 2023, the FDA approved a prescription device that provides real-time glucose values and trends in these levels over time through a mobile app installed on a smart phone or other compatible device (brand name: Eversense E3 CGM System). This system includes a small sensor that is implanted under the skin by the patient's physician. The device can be worn for up to 180 days [63]. In 2024, the FDA expanded its approval for the system designed to function for an entire year. The sensor transmits glucose data every five minutes to a mobile app, allowing users to track their glucose levels in real time [64]. In 2024, the FDA cleared for marketing the first over-the-counter CGM intended for patients 18 years of age and older who do not use insulin (Dexcom Stelo Glucose Biosensor System) [65]. This system uses a wearable sensor, paired with an app on the user's smartphone or other smart device, to continuously measure, record, analyze, and display glucose values. Data from a clinical study provided to the FDA showed that the device performed similarly to other integrated CGMs [65].
Although the clinical benefit of smartphone applications (apps) for diabetes remains unproven, these apps continue to grow in popularity. Healthcare providers should familiarize themselves with available diabetes apps to both support their clinically beneficial features and advantages and advise patients about shortcomings [66]. Smartphones are always within reach, nearly every patient and clinician has one, and they appeal to all age groups. In contrast, traditional diabetes devices (e.g., glucose meters) are frequently left behind (e.g., during social gatherings or work days). Other advantages that smartphones offer include: advanced functionality; useful for performing mundane tasks repetitively without error; and convenient, accurate transfer of diabetes data [66]. The Association of Diabetes Care and Education Specialists (ADCES) provides information on a variety of mobile apps, including those that focus on diabetes management (Resources).
Since January 2018, the Centers for Medicare and Medicaid Services has allowed eligible practitioners to bill for reimbursement for time spent interpreting and collecting health data generated by patients remotely [66].
Although SMBG using a capillary blood sample is indispensable in the day-to-day management of diabetes, results from these tests have some limitations. One such limitation is that results of SMBG reflect the blood glucose for a specific moment in time without giving an indication of overall blood glucose control. The glycated hemoglobin test, more commonly known as the HbA1c, is a laboratory test that uses a venous blood sample to show the average blood glucose over the previous two to three months.
The test works by measuring the amount of glucose that is chemically attached to the red blood cells (RBCs). RBCs that have been exposed to high amounts of glucose over their life span, which is about three months, will have more glucose attached to them. Results of the HbA1c test are expressed as a percentage, reflecting the relative amount of glucose that has been in the blood over the previous two to three months. Based on extensive studies, the ADA recommends a general HbA1c goal of less than 7% to prevent microvascular and macrovascular complications of diabetes [9,67].
The ADA advocates utilizing the "estimated average glucose" (eAG) to report HbA1c results to patients. The eAG correlates HbA1c percentage points with its equivalent in mg/dL. Because glucose meters used in the United States are calibrated in mg/dL, it is believed that reporting results as an eAG will help patients better understand what they mean. For example, for an HbA1c of 7.5%, the eAG is 169 mg/dL. The ADA provides an online calculator for individuals to enter their HbA1c and have the eAG determined [67].
When discrepancies arise between HbA1c levels and the patient's reported SMBG results, further patient education and counseling may be indicated. These discrepancies may reflect poor SMBG technique on the part of the patient, mechanical problems with the meter, or other limitations on the part of the patient. They may also indicate that the patient is falsifying the results of SMBG. In this situation, careful and sensitive probing may uncover problems in coping with diabetes.
Unhealthy diet is a major risk factor for type 2 diabetes; however, nutrition therapy is one of the most challenging aspects of diabetes care [68,69,70]. Diet-related issues are complex, requiring that behavioral, functional, cognitive, and socioeconomic aspects of each patient be considered. In addition, cultural and religious customs play a significant role in a person's ability and desire to adhere to a recommended meal plan.
Many people, both lay and professional, are misinformed about the nutritional management of diabetes. Some would be surprised to learn that there really is no such thing as a "diabetic diet." Furthermore, believing that diabetes can be managed by simply avoiding sugar suggests inadequate information about the dietary management of the disease [71]. Contrary to common belief, ADA guidelines indicate that within the context of healthy eating, a person with diabetes can generally eat the same foods that a person without diabetes can eat. This means that the same principles of good nutrition that apply to the general population also apply to people with diabetes [72].
Because of the complexities associated with diet-related behavior, and because meal planning is so important to diabetes management, medical nutrition therapy provided by a registered dietitian is advocated [6,73,74]. Medical nutrition therapy is defined as nutritional diagnostic, therapy, and counseling services for the purposes of disease management, which are furnished by a registered dietitian or nutrition professional. Medical nutrition therapy delivered by a registered dietician nutritionist is associated with A1c absolute decreases of 1.0% to 1.9% for people with type 1 diabetes and 0.3% to 2.0% for people with type 2 diabetes [6]. Medical nutrition therapy, when provided by a registered dietitian, is reimbursed by the Medicare program [73]. Whenever possible, healthcare providers should be prepared to work with dieticians as part of an interdisciplinary diabetes care team. Frequently, however, access to a dietician is not feasible for patients whose healthcare plans do not cover this service or for those who live in remote geographic areas.
In some settings, a nurse may assume responsibility for teaching dietary management to patients with diabetes. In virtually all cases, nursing care will involve supporting recommendations made by a registered dietitian. The following information is not intended, nor is it able, to replace the team effort that involves the patient, the physician, the dietician, the diabetes educator, and others who are required for optimal management of diabetes. However, because all of these resources are not always available, this information can serve as a guide to start or supplement nutrition education for diabetes care.
The national nutrition policy, outlined by the Dietary Guidelines for Americans, serves as a basis for healthy eating by people with or without diabetes [75]. These guidelines focus on a diet composed primarily of nutrient-dense foods, such as whole grains, fresh fruits, and fresh vegetables. The guidelines also recommend moderation when using sugar, salt, and alcohol and advocate the maintenance of appropriate weight. In the past, the Food Pyramid illustrated dietary recommendations for the public based on intake from various food groups.
In 2011, the U.S. Department of Agriculture replaced the traditional Food Pyramid and the interactive version MyPyramid with a program called Choose My Plate (now simply referred to as "MyPlate") [76]. The ADA recommends that patients with diabetes, their diabetes educators, and/or registered dietitians establish a personalized nutrition plan. To assist in establishing a nutrition plan, the ADA developed a program called the Diabetes Plate Method (formerly Create Your Plate) as a meal planning template for people with diabetes [77].
Although sugar was previously forbidden to those with diabetes, ADA guidelines for its use have been liberalized in recent years. ADA guidelines now allow individuals with diabetes to occasionally substitute sugar-containing foods for other carbohydrates as part of a balanced meal plan, if adequately covered with insulin or other glucose-lowering medication as needed. The rules for sugar were relaxed because there is little scientific evidence to support the assumption that simple sugars aggravate hyperglycemia to a greater degree than starches.
In 2013, the ADA issued a position statement advocating for the individualization of eating plans for persons with diabetes [78]. In 2019, the ADA issued a consensus report on nutrition therapy [79]. In both documents, the ADA contends that there is no "one-size-fits-all" diet for patients with diabetes and nutritional recommendations should be based on personal and cultural preferences, comorbidities, health literacy, food access, and willingness to make behavioral changes [78,79]. Some of the key recommendations in this consensus report are [79]:
A variety of eating patterns are acceptable for persons with diabetes. Healthcare providers should focus on the key factors common among the patterns, including emphasizing nonstarchy vegetables, minimizing added sugars and refined grains, and choosing whole foods over highly processed food, to the extent possible.
Education and support for persons with diabetes who are overweight or obese should include an individualized eating plan in a format that results in an energy deficit in combination with enhanced physical activity to a targeted, recommended 5% weight loss.
Consider lifestyle intervention for people with prediabetes at a healthy weight.
Screen and evaluate people with diabetes/prediabetes during DSMES and medical nutrition therapy encounters for disordered eating.
Exchange Lists
Exchange lists were developed by dieticians in the 1950s to help people with diabetes make daily food choices that would maintain a balance of carbohydrate, protein, and fat from day to day. Any food in one group can be exchanged for another food within the same group. An exchange system can be thought of as a "food budget," giving a certain number of food choices to spend at each meal. Examples of exchanges are shown in Table 8.
GUIDE TO SERVING SIZES FOR MEAL PLANNING
| Category | One Serving Size | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Starches and grains |
| ||||||||
| Vegetables |
| ||||||||
| Fruit |
| ||||||||
| Milk |
| ||||||||
| Meat and other proteins |
| ||||||||
| Fats and oils |
| ||||||||
| Sweets and desserts |
|
In the exchange system, each serving of carbohydrate is equal to 15 grams. Patients are given a list of 15-gram serving sizes of common carbohydrate foods and instructed to consume a specified number of servings from each food group per meal or snack. For example, if three servings of starches and grains are recommended per meal, the patient may select any combination of three of the foods listed in the amount specified for that food group [80].
Carbohydrate Counting
Carbohydrate counting is a method for keeping track of the amount of carbohydrate in each meal or snack. Emphasis is placed on the total amount of carbohydrate in a meal or snack rather than on the source. Limits are set for the maximum amount of carbohydrate that should be consumed for each meal or snack. Foods counted as carbohydrates are starches (including starchy vegetables), sugars, milk, and fruit. Nonstarchy vegetables are so low in carbohydrates that they are generally not included in carbohydrate counting. According to the ADA, evidence suggests that there is not an ideal percentage of calories from carbohydrate, protein, and fat for all people with or at risk for diabetes; therefore, macronutrient distribution should be based on individualized assessment of current eating patterns, preferences, and metabolic goals [79].
Because carbohydrates affect blood glucose levels more than any other type of food, insulin dosages can be adjusted based on the amount of carbohydrate consumed. This provides an opportunity for fine-tuning blood glucose control, while allowing greater flexibility with meal content and timing for those who are able to handle a higher level of self-management. While the opportunity for tight glycemic control cannot be overstated, the abilities and motivation of the individual should be taken into account before recommending carbohydrate-to-insulin ratios as a self-management tool. In general, counseling people on eating patterns that replace foods high in carbohydrate with foods lower in carbohydrate and higher in fat may improve glycemia, triglycerides, and HDL-C [79].
The Diabetes Plate Method
The Diabetes Plate Method is a widely used approach to teaching healthy eating choices and is appropriate for people with diabetes [77,81,82,83]. Its premise is that healthy eating and controlling portion sizes can be simplified by using a visual image of a plate showing the proper amounts of foods to be consumed in a meal (Figure 1). The plate method has been shown to help people with diabetes lose weight, plan meals correctly, improve intake of fruits and vegetables, and reduce the incidence of hypoglycemia without sacrificing glycemic control [83].
The teaching tenets of the Plate Method are [77,84]:
Use a nine-inch dinner plate.
Fill approximately one-half of the plate with nonstarchy vegetables, such as leafy greens, onions, peppers, tomatoes, cucumbers, green beans, broccoli, carrots, cauliflower, and others.
Fill one-fourth of the plate with lower fat protein foods, such as lean cuts of meat, fish, poultry with skin removed, egg whites and egg substitutes, two ounces of reduced-fat cheese, plant-based proteins (e.g., beans, lentils, edamame, tofu, hummus, tempeh), nuts, or spreads (e.g., peanut or almond butter).
Fill one-fourth of the plate with grains and starchy food, such as whole grain breads, brown rice, whole grain pasta, potatoes, pumpkin, corn, or peas.
Add a small piece of fruit, one-half cup fresh frozen or canned fruit, or two tablespoons of dried fruit.
Add a low-calorie drink, such as water, unsweetened tea, or coffee.
The plate method is very helpful as a first step in learning to control portion sizes and to plan healthy meals. It is also helpful for patients who are overwhelmed by too much information and for those who do not like strict regimens. The plate method is also recommended for people of low-literacy and those who have barriers to weighing and measuring foods [77,85].
Two methods can be used to assess recent food intake and dietary patterns. One method is the 24-hour dietary recall, in which the patient is asked to recall everything that was consumed over the past 24 hours. Another method is to ask the patient to keep a food diary. This is a log kept by the patient for a specified number of days in which he or she keeps an ongoing record of everything that is consumed over that time. While food diaries can provide valuable assessment data to the nurse, they can also benefit the patient by providing feedback on current eating patterns. The following case study will demonstrate how information gathered from a 24-hour dietary recall can be used to formulate a dietary teaching plan.
Patient C is a moderately obese White woman, 67 years of age, who has recently been diagnosed with type 2 diabetes. Her physician has recommended dietary modification and a walking program to manage her diabetes and promote weight loss. No diabetes medications have been prescribed at this time. As the nurse working in her physician's office, you are asked to provide Patient C with education on the dietary management of her diabetes. As part of your needs assessment, you ask the patient to provide a 24-hour dietary recall. The results and analysis of the dietary content are reported inTable 9.
24-HOUR DIETARY RECALL FOR PATIENT C
| Breakfast | Black coffee | |||||
| Mid-Morning |
| |||||
| Lunch |
| |||||
| Afternoon | Two chocolate-covered graham cookies | |||||
| Dinner |
| |||||
| Evening | 8 oz low-fat, sugar-sweetened yogurt |
Discussion
After reviewing Patient C's 24-hour dietary recall, you are able to identify areas where you can most appropriately focus teaching about nutrition. You do this by comparing the overall composition of her diet to the general nutritional recommendations. You can see by Patient C's 24-hour dietary recall that she tends to select foods that are high in both fat and sugar. She will need to know that these types of foods add unnecessary calories to her diet and contribute to her obesity. While you can calculate six servings of added fat in her diet (margarine), you also see that her intake contains several sources of "hidden fat," which greatly increase her overall fat intake. Examples of the high-fat foods she consumed are cheese, higher-fat hamburger, french fries, and chocolate-covered cookies. You should inform Patient C that for weight and cardiac-risk reduction, these foods should be consumed less frequently. You can suggest substituting lower-fat versions of these foods. These may include lean hamburger, low-fat or nonfat cheese, and a baked potato instead of fries. She can also reduce her saturated fat intake by choosing nonfat milk and nonfat yogurt. In place of margarine, she could consider using nonfat butter substitute or fat-free sour cream.
Assessment also reveals that Patient C's diet is low in fiber and vegetables and lacking fresh fruits of any kind for the particular day being examined. You can recommend that she begin substituting some of her higher-calorie food choices with fresh fruits or vegetables. This will help her lose weight while increasing her fiber intake. You can teach her about fruit serving sizes so that she does not increase her overall intake of sugar with the addition of fruit to her diet. The benefits of weight control should be emphasized, as some people with type 2 diabetes are able to control their diabetes with weight reduction alone.
Another point revealed by Patient C's dietary report is that most of her caloric intake is concentrated toward the end of the day. She should be advised that her glycemic control could improve if she distributes calorie and carbohydrate intake throughout the day. She can achieve this by eating smaller meals and snacks and spacing them evenly throughout the day. Eating breakfast can have a positive influence on appetite control, food choices, and metabolism, and thus help with weight management. A possible reason for this is that eating breakfast helps the person avoid becoming overly hungry, which can later lead to overeating and poor food choices. It is also believed that eating a healthy breakfast can set the psychologic and behavioral tone for the day, prompting better food choices overall [86].
After providing Patient C with these general guidelines for nutrition, you can begin teaching her about portion control using the plate method. An actual 9-inch dinner plate and food models can be used to help her visualize the amount of foods that she should be eating from each group. The recommended meal plan can be individualized by taking into account the types of foods that the patient is already eating. Then, you can suggest healthier substitutions for those foods so she is not faced with major changes in basic dietary content. To illustrate this concept, each food group will be discussed in turn.
Grains and Starchy Foods
Some of Patient C's starch choices were appropriate, and she can be encouraged to continue these foods in appropriate amounts. These included whole-wheat crackers (encourage lower-fat choices) and the baked potato, assuming appropriate portion size. Both of these starch sources add fiber and other nutrients to the diet. She should be instructed that she could significantly increase her intake of fiber from the potato by consuming its skin. The nurse should help Patient C explore potential substitutions for the less appropriate sources of starch in her diet. For example, a baked or boiled potato, with skin, could be substituted for the french fries, and whole-grain breads should be substituted for white. You can also explore ideas for increasing whole grain intake at breakfast. This can include eating oatmeal, high-fiber sugar-free cold cereals, or whole-grain breads.
Non-Starchy Vegetables
For patients with diabetes, vegetables provide a moderate source of carbohydrate with the benefit of being rich in fiber, vitamins, and minerals. They offer the added benefit of being naturally devoid of fat and very low in calories. Although canned and frozen vegetables may be an acceptable source, fresh produce is desirable.
Like many Americans, Patient C probably does not consume enough fresh vegetables on a daily basis. While one cup of canned green beans partially fulfills her daily serving allowance of vegetables, she could obtain more nutritional value from fresh sources, such as salads and raw produce. These are often higher in fiber and provide more variety of vitamins and minerals. They may also be more satisfying because the serving size for raw vegetables is larger than for cooked. Fresh vegetables also require more chewing and take longer to eat. The ADA recommends at least three to five servings of vegetables per day. This is a minimum requirement, and more is considered better. Non-starchy vegetables do not need to be counted when using the carbohydrate counting method. When following the plate method, half of the plate should be covered with non-starchy vegetables and salad can be added on the side [87].
Fruit
Although fruit is a source of fructose, or fruit sugar, it is not forbidden to individuals with diabetes. There are many health benefits to eating fruit, including its provision of fiber, vitamins, and minerals to the diet. In the case of Patient C, she should be advised to begin reducing the amount of sucrose that she eats and replacing it with three servings of fruit each day. Whole fresh fruit is desired, although unsweetened canned fruit is acceptable. Whole fruits are strongly advised over juice because they offer the benefits of fiber, take longer to ingest, and may be more filling than juice. When instructing the patient about serving sizes of fruit, it should be emphasized that one serving is equal to a small piece of fruit, ½ banana, or 1¼ cup of strawberries.
Milk
Patient C should begin substituting nonfat milk and yogurt for the low-fat types she is currently using. When selecting yogurt, it should be plain or sweetened with a sugar substitute. Sugar-sweetened yogurt typically contains about 30 grams of carbohydrate, which is the same amount that she would get from two servings of milk.
Protein
Because cheese is categorized as a meat/protein, Patient C's 24-hour dietary recall reflects a surplus intake. She should be advised that large quantities of protein in the diet generally add to its fat content, especially if red meats, fried meats, or high-fat cheeses are selected. Although skinless baked chicken represents an appropriate meat choice for Patient C, she should be encouraged to make choices such as these more consistently. Strategies would include reducing portion sizes and consistently selecting poultry and fish over red meat. It should be reinforced that it is desirable to prepare meats by baking, broiling, and boiling. Meats that have been fried or have had fat added should be avoided. Processed meats, such as lunchmeat and hot dogs, should also be avoided due to their high fat and sodium contents. When selecting cheeses, the patient should be advised to choose lower-fat varieties, such as cottage cheese or reduced-fat hard cheeses.
Fat
As discussed, sources of hidden fat should be avoided in the diet. The number of recommended fat servings refers specifically to fat that has been added to food. An example of added fat included in Patient C's diet is the margarine that she used on her bread and potatoes. On a 1,500-calorie diet, four servings of added fat are recommended. Patient C should be instructed in strategies for reducing her overall fat intake, especially from hidden fat sources. She should be advised to read food labels when shopping to guide her in selecting foods lower in fat, especially the saturated and trans fat types. She can also be referred to a number of cookbooks published by the ADA and the American Heart Association that are readily available in bookstores, libraries, and on the Internet. Other suggestions for Patient C may include ideas for seasoning vegetables and potatoes without fat. Examples include using lemon juice, mustard, nonfat salad dressings, hot pepper sauce, garlic, ground pepper, nonfat sour cream, and other herbs and spices instead of fats and oils.
Sugar
Guidelines for the use of sugar by people with diabetes have been discussed. Patient C will need education and support in curtailing her high intake of sugar. She should be advised that although sugar is not absolutely forbidden to her now that she has been diagnosed with diabetes, she would need to learn how to make choices about sugar as part of an overall plan for healthy eating. As part of her meal plan for diabetes, Patient C can occasionally substitute a serving of sugar for a serving of fruit, starch, or milk. An example of an appropriate sugar substitution would be to have a 3-inch cookie in place of an orange. It should be recognized that the nutritional value of the cookie is inferior to that of the orange and therefore should only be an occasional substitution.
Diet, exercise, and self-management education are the foundation of type 2 diabetes treatment. All treatment, including the use of pharmacotherapy, should be individualized. Furthermore, all treatment decisions should be made in conjunction with the patient and should take into account his or her preferences, needs, and values [20].
Pharmacotherapy for diabetes should be started early to prevent or slow progressive beta cell failure. Due to the various physiologic defects that underlie the pathology of diabetes, multiple drugs used in combination may be required to achieve therapeutic goals. Pharmacologic agents may be used alone as monotherapy or in combination with other medications, which may or may not include insulin. In addition to meeting glycemic targets, addressing cardiovascular risk factors is another major focus of therapy [20].
At this time, the only biguanide available in the United States is metformin. Unless contraindicated, metformin is the optimal first-line drug [6]. Metformin is available in generic form and also in an extended-release formulation (Glucophage XR). Metformin has been combined with several other medications, including glipizide (Metaglip) and glyburide (Glucovance), as fixed-combination formulations [18].
Mechanism of Action
The primary action of metformin is to reduce glucose production from the liver [18]. Because metformin does not cause the body to make more insulin, it rarely causes hypoglycemia when used alone. A secondary action of metformin is that it increases insulin sensitivity in the muscle and liver tissue [18]. This provides for better utilization of existing insulin. An added benefit of metformin is its favorable effect on blood lipids. This may contribute to cardiovascular risk reduction in some patients with type 2 diabetes. Metformin is excreted by the kidneys and can accumulate in patients with renal dysfunction [18]. Therefore, it may not be an appropriate choice for all patients.
Nursing Implications and Patient Teaching Principles
Minor but common side effects of metformin include gastrointestinal disturbances such as diarrhea, nausea, and abdominal cramping. Taking metformin with meals can reduce these side effects. Although metformin is unlikely to cause hypoglycemia when taken alone, low blood glucose may still occur when it is taken with insulin or sulfonylurea agents.
Serious side effects are very rare and usually occur in those with impaired renal or liver function. Lactic acidosis is the most serious side effect and can be life-threatening, although it is extremely rare. Because the liver is responsible for removing lactate from the system, patients with a history of heavy alcohol abuse and/or binge drinking should not use metformin. It should be used with caution in patients with congestive heart failure, as an exacerbation of this condition can predispose the patient to lactic acidosis. Metformin should also be temporarily withheld when patients undergo any procedure using iodinated contrast dye due to its excretion by the kidneys.
These oral hypoglycemic medications have been widely used to treat type 2 diabetes since the 1950s. In the past, it was estimated that approximately 40% of people with type 2 diabetes were treated with this class of oral medication, although this has changed significantly, as newer drugs have been introduced. Compared with sulfonylureas, metformin as first-line therapy has beneficial effects on A1c, weight, and cardiovascular mortality. There are little systematic data available for other oral agents as initial therapy for type 2 diabetes [6].
Mechanism of Action
Sulfonylureas act primarily by increasing insulin production from the pancreas. They can be further classified as first- or second-generation hypoglycemic agents. The first-generation agent previously used in the United States is chlorpropamide; however, chlorpropamide and acetohexamide have been discontinued, and tolbutamide and tolazamide are no longer recommended treatment options for type 2 diabetes [18]. Although no first-generation sulfonylurea agents are currently used in the United States, it is important to have an understanding of all medications within this category in the rare case a patient presents with a history of having taken one of these agents. Second-generation sulfonylureas include glipizide, glyburide, and glimepiride, among others [6]. They have largely supplanted the use of first-generation sulfonylureas because they have the convenience of once or twice a day dosing and the potential for fewer adverse effects.
Nursing Implications and Patient Teaching Principles
The primary adverse effect associated with the sulfonylureas is hypoglycemia. Nurses should instruct patients with regard to the risk for hypoglycemia while using these drugs as well as on preventive and treatment measures. The elderly are particularly susceptible to hypoglycemic reactions, largely due to the age-related decline in renal function that slows the excretion of these drugs. Another common adverse effect of medications in this class is weight gain. Other, less common side effects include skin reactions and gastrointestinal disturbances.
Patients should be instructed to take their pills daily, at the same time each day. The standard dose of glipizide is taken three times per day to obtain optimal effect; extended-release glipizide and other sulfonylurea agents are taken only once per day.
The two agents in this class, also referred to as meglitinide derivatives or glinides, are repaglinide, which is a meglitinide, and nateglinide, which is a D-phenylalanine derivative.
Mechanism of Action
Like the sulfonylureas, the nonsulfonylurea secretagogues lower blood glucose by stimulating insulin release from the pancreas. In contrast to the sulfonylureas, these agents are rapidly absorbed and eliminated, with a half-life of approximately 1 to 1.5 hours [18]. When the secretagogue is taken just before meals, the amount of insulin released from the pancreas increases during and just after a meal, mimicking the normal islet cell response to eating. Because of their rapid elimination, these secretagogues do not cause the beta cells of the pancreas to continuously release insulin for long periods of time. Therefore, patients treated with these medications have less risk of hypoglycemia than those treated with sulfonylureas.
Nursing Implications and Patient Teaching Principles
As with the sulfonylureas, adverse effects associated with repaglinide include hypoglycemia and weight gain. However, hypoglycemic episodes related to the use of nonsulfonylurea secretagogues are less frequent and less serious. Other side effects include upper respiratory infection, headache, and inflammation of the nasal and sinus tissue.
Patients taking this agent should be instructed to take their pills 15 to 30 minutes prior to each meal. The number of doses taken is determined by the number of meals eaten. For example, if a meal is missed, the corresponding dose of medication is skipped. Conversely, a dose is added when an extra meal or large snack is taken.
Often described as insulin sensitizers, examples of thiazolidinediones (TZDs) include pioglitazone and rosiglitazone [6]. The first drug in this group, troglitazone, was removed from the market because it was shown to cause serious liver problems in a small number of people [88].
Mechanism of Action
Medications in this class improve the body's ability to use insulin. Insulin action is enhanced by "opening up" the insulin receptors in the liver and skeletal tissues. When this occurs, insulin resistance is reversed and the body is able to utilize circulating insulin more effectively. A secondary action of the insulin sensitizers is that they decrease the production and release of glucose from the liver. Because these agents are not hypoglycemic agents, they will not generally lower blood glucose to levels below normal. When used in combination with insulin or sulfonylureas, the potential for hypoglycemia exists [18].
Nursing Implications and Patient Teaching Principles
In general, the insulin-sensitizing agents are well tolerated by patients. Occasional minor side effects may include headache, dizziness, and edema. A much more serious, but still uncommon, adverse effect of these medications is the elevation of liver enzymes leading to severe hepatocellular injury. Although hepatic injury may be reversible, cases resulting in liver transplantation and/or death have occurred in patients who used troglitazone, a thiazolidinedione medication that has been taken off the market. Pioglitazone and rosiglitazone are associated with a higher level of safety in this regard. Chances of drug-related liver complications can be reduced with proper monitoring. TZDs should not be used in those patients with alanine transaminase values of more than 2.5 times the upper limit [89]. Liver function tests are periodically monitored throughout therapy and should be obtained for all patients at the first symptoms suggestive of liver dysfunction, such as nausea, vomiting, abdominal pain, anorexia, or dark urine [18,88].
In 2006, results from A Diabetes Outcome and Progression Trial (ADOPT), a large, randomized, double-blind, parallel group study, indicated that women taking rosiglitazone had a higher risk for fractures (9.30%) compared to those taking either metformin (5.08%) or glyburide (3.47%). Women taking rosiglitazone were reported to have more fractures of the humerus, hand, and foot. The researchers noted that this increase was not evident in spine or hip fractures or in male patients [90].
Rosiglitazone has been associated with increased risk for angina, myocardial infarction, fluid retention, and worsening of heart failure. The risk for heart attack appears to be higher for those who took rosiglitazone with insulin or nitrates [88]. Therefore, most people who take insulin or nitrates should not take this medication. Furthermore, rosiglitazone is contraindicated in people with heart failure [18,91,92]. In 2007, the FDA concluded that the boxed warning on both rosiglitazone and pioglitazone should be strengthened [93]. In 2010, the FDA issued a Risk Evaluation and Mitigation Strategy (REMS) that severely restricted the use and availability of rosiglitazone. The agency eliminated this REMS and its prescribing and dispensing restriction in 2016; however, despite the restrictions being lifted, the use of rosiglitazone remains very low, and some combination products have been discontinued [94,95,96,97]. In addition to choosing alternative medications for patients with heart failure, patients who use a TZD should be closely monitored for signs and symptoms of heart failure.
Acarbose and miglitol are the medications in this class, which are often described as "starch blockers."
Mechanism of Action
Alpha-glucosidase inhibitors (AGIs) work by slowing the digestion of carbohydrate in the small intestine [18]. This results in decreased postprandial blood glucose levels due to delayed absorption of sugars and starches into the bloodstream.
Nursing Implications and Patient Teaching Principles
Gastrointestinal disturbances are commonly related to the use of starch blockers. These include flatulence, diarrhea, and abdominal pain [88]. In many cases, these side effects are dose-related, are self-limiting with continued use, and may be avoided by starting with low dosages and gradually increasing as tolerated.
Patients should be instructed that pills be taken with the first bite of each main meal [88]. While these drugs alone do not cause hypoglycemia, special instructions should be given to patients who use them in combination with sulfonylureas or insulin. In these cases, patients may encounter a delayed response when trying to treat hypoglycemia caused by other drugs. Because the absorption rate of sucrose is drastically reduced with the administration of AGIs, prolonged hypoglycemia can result when conventional sucrose-containing treatments are administered. In cases when medications causing hypoglycemia are used in combination with an AGI, patients should be given specific instructions on how to treat hypoglycemia. Effective treatment consists of taking three to four glucose tablets, one tube of glucose gel, or 10 to 12 ounces of skim milk.
Recently, there has been a flurry of activity in the development and use of incretin-based therapies for the treatment of type 2 diabetes. As discussed, the two incretin hormones are GLP-1 and GIP. The first FDA-approved incretin mimetic was exenatide, sold under the trade name Byetta or Bydureon (extended-release). Exenatide is available in prefilled injection pens and as a kit containing 2 mg of the drug and a diluent [98,99]. Exenatide injection has been approved for use as monotherapy in the treatment of type 2 diabetes, although it is commonly used in combination therapy.
Since the approval of exenatide, additional GLP-1 receptor agonists have been approved by the FDA for the treatment of diabetes, including dulaglutide and liraglutide [18]. Liraglutide is a daily injection, while dulaglutide is administered weekly [18,100,101]. As with exenatide, these drugs are approved for monotherapy or as an addition to an existing regimen [18]. However, dulaglutide and liraglutide are considered second-line therapies. Another GLP-1 receptor agonist, lixisenatide, received FDA approval in July 2016 [18]. In 2019, the FDA approved semaglutide (Rybelsus), the first oral GLP-1 agent for type 2 diabetes [102]. It is not recommended as first-line therapy and is contraindicated in patients with type 1 diabetes or diabetic ketoacidosis. [102].
GLP-1 receptor agonists, with or without metformin based on glycemic needs, are an appropriate initial therapy for individuals with type 2 diabetes who are either with or at high risk for atherosclerotic cardiovascular disease, heart failure, and/or chronic kidney disease. Among these patients, GLP-1 receptor agonists have demonstrated cardiovascular disease benefit. A GLP-1 receptor agonist is preferred to insulin, when possible, in patients with type 2 diabetes. If insulin is used, combination therapy with a GLP-1 receptor agonist is recommended for greater efficacy and durability of treatment effect [6].
Mechanism of Action
These medications mimic the action of the incretin hormones GLP-1 and GIP, leading to an increase in insulin secretion from the pancreas. An additional beneficial effect is delayed gastric emptying, which increases satiety and promotes weight loss.
Nursing Implications and Patient Teaching Principles
The recommended initial dosage for the exenatide pen preparation is 5 mcg twice daily within one hour prior to a meal [18]. The recommended dosage for the 2-mg kit is once every seven days (weekly); it can be administered at any time of day, with or without meals [18]. Exenatide is not labeled for use with insulin and should not be used in patients with a history or high risk of pancreatitis. If liraglutide is prescribed, the initial dose is 0.6 mg subcutaneously once daily for one week, after which it is increased to 1.2 mg once daily [18]. The dose may be increased to 1.8 mg once daily if optimal glycemic response not achieved with 1.2 mg per day [18].
The recommended dosage for semaglutide is 3 mg once daily for 30 days. This dosage is intended for treatment initiation, not for effective glycemic control. After 30 days on the 3-mg dose, increase to 7 mg once daily. Dose may be increased to 14 mg once daily if additional glycemic control is needed after 30 days on the 7-mg dose. Semaglutide should be taken at least 30 minutes before the first food, beverage, or other oral medications of the day and with no more than 4 ounces of plain water [18]. If a dose is missed, the missed dose should be skipped, and the next dose taken the following day [18,103].
The initial dose of dulaglutide is 0.75–1.5 mg once weekly. It should be administered on the same day each week.
In 2013, the FDA began investigating unpublished new findings by a group of researchers that suggest an increased risk of pancreatitis and pancreatic duct metaplasia in patients with type 2 diabetes treated with incretin mimetics, including exenatide and liraglutide, among others [104]. The most common side effects are nausea, vomiting, and diarrhea. Hypoglycemia can occur if used in conjunction with a sulfonylurea [105]. The medications also contain black-box warnings due to an increased risk for thyroid C-cell tumors [18]. As the incretin mimetics are administered subcutaneously (with the exception of semaglutide oral tablets), patient education regarding proper injection technique, use of the injection pens, and disposal of used pens may be necessary.
Also known as dipeptidyl peptidase-4 (DPP-4) inhibitors or incretin enhancers, medications in this group include sitagliptin, saxagliptin, linagliptin, and alogliptin [6].
Mechanism of Action
DPP-4 is an enzyme that rapidly inactivates the incretin hormones. By inhibiting DPP-4, gliptins prolong active incretin levels, allowing for increased insulin action following the post-meal rise in blood glucose. Unlike incretin mimetics, gliptins do not slow gastric emptying or produce satiety and weight loss [106].
Nursing Implications and Patient Teaching Principles
The gliptins are oral agents taken once a day, with or without food. They are unlikely to cause hypoglycemia because they do not work well when blood glucose is low. Combination therapy with insulin has not been studied, but gliptins may be used with other oral antidiabetic agents. The most common side effects are upper respiratory infection, urinary tract infection, and headache [107,108,109].
Pramlintide acetate is an analog of the human hormone, amylin. It is an injection to be used with mealtime insulin in people with either type 1 or type 2 diabetes.
Mechanism of Action
Like insulin, amylin is a hormone produced from the beta cells of the pancreas and works with insulin to regulate glucose control. Beta cell destruction can result in deficiencies of both of these hormones. As a synthetic version of amylin, pramlintide acetate functions similarly to the native hormone, working in partnership with insulin to control blood glucose. Amylin also slows gastric emptying, decreasing appetite and promoting weight loss. Additionally, amylin suppresses glucagon secretion, leading to decreased post-prandial concentration in the blood [18].
Nursing Implications and Patient Teaching Principles
Pramlintide acetate (Symlin) is to be injected before meals. When used with insulin, pramlintide acetate has been associated with an increased risk for severe insulin-induced hypoglycemia, especially in patients with type 1 diabetes. This usually occurs within three hours of injection [18,110]. Therefore, appropriate patient selection, careful patient education, and insulin dose adjustments are essential. Patients who have hypoglycemic unawareness, poor compliance with blood glucose monitoring, or a history of severe hypoglycemia should not be considered for use of this drug. Patients who use pramlintide acetate should be instructed to monitor pre- and post-meal blood glucose frequently and to reduce their pre-meal short acting insulin by 50% when starting the medication [18,110]. Other common side effects of pramlintide acetate are nausea, vomiting, decreased appetite, and swelling or itching at the injection site.
Canagliflozin, the first in the new class of diabetes medications referred to as sodium-glucose co-transporter 2 (SGLT2) inhibitors, was approved by the FDA in 2013 [18,111]. Two additional agents, dapagliflozin, and empagliflozin were approved in 2014 [18,112,113]. Ertugliflozin was approved in 2017, and bexagliflozin was approved in 2023 [18,114]. These oral medications are taken each morning.
Mechanism of Action
These agents act by inhibiting SGLT2 in the proximal renal tubules, which reduces reabsorption of filtered glucose from the tubular lumen and lowers the renal threshold for glucose. SGLT2 is the main site of filtered glucose reabsorption, and reduction of filtered glucose reabsorption and lowering the renal threshold result in increased urinary excretion of glucose and improved plasma glucose concentrations [18].
Nursing Implications and Patient Teaching Principles
The recommended initial dose of canagliflozin is 100 mg once daily prior to the first meal of the day [18,111]. The dose may be increased up to 300 mg per day, unless the patient has impaired renal function [18]. Dapagliflozin is dosed at 5 mg/day but may be increased to a maximum of 10 mg/day [18,112]. The initial dose of empagliflozin is 10 mg/day, but this may be increased up to 25 mg/day for optimal glycemic control [18,113]. Ertugliflozin is initially dosed at 5 mg once daily but may be increased to 15 mg once daily after 4 to 12 weeks [18]. The daily dose of bexagliflozin is 20 mg [18]. All five agents are approved for use with diet and exercise to improve the control of type 2 diabetes in adult patients. They have been studied for use as monotherapy and in combination with other antidiabetics, including metformin, sulfonylureas, pioglitazone, and insulin [111]. The most common side effects associated with SGLT2 inhibitors are vulvovaginal candidiasis and urinary tract infection [18,111]. In 2018, the FDA issued a warning about rare but serious necrotizing fasciitis of the perineum associated with SGLT2 inhibitor therapy [115].
First approved by the FDA in 2009, only one medication, bromocriptine, in the class of dopamine agonists is approved for the treatment of type 2 diabetes.
Mechanism of Action
Bromocriptine mesylate is a novel formulation of bromocriptine that targets neuroendocrine patterns associated with insulin resistance. As a dopamine D2 receptor agonist, this medication activates dopamine receptors, affecting the circadian clock and its influence on glucose metabolism, insulin resistance, and perhaps cardiovascular pathology [116].
Nursing Implications and Patient Teaching Principles
Bromocriptine mesylate is started at a dose of 0.8 mg orally once daily and increased at weekly intervals in 0.8-mg increments, as tolerated. The usual effective dosage is 1.6–4.8 mg once daily (maximum: 4.8 mg/day). Bromocriptine is quick acting and should be taken within two hours of waking. It should also be taken with food to minimize gastrointestinal effects [18].
Possible adverse effects include nausea, fatigue, rhinitis, headache, and dizziness. These are most likely to occur during initial titration and lasted a median of 14 days in clinical trials [6]. Bromocriptine does not cause hypoglycemia and is not recommended for patients with psychosis or syncopal migraines [6].
With the introduction of new antidiabetic medications, several possible combinations of medications may now be used to treat type 2 diabetes. Combination therapy may include the concurrent use of two or more oral agents, the use of insulin with one or more oral agents, or the use of insulin with pramlintide acetate. The chief benefit of combination therapy is improved glycemic control due to the additive effect of multiple agents acting via different mechanisms. Traditional recommendations have been to use stepwise addition of medications to metformin to maintain A1c at target. The advantage of this is to provide a clear assessment of the positive and negative effects of new drugs and to reduce potential side effects and expense. However, there are data to support initial combination therapy for more rapid attainment of glycemic goals and later combination therapy for longer durability of glycemic effect [6].
Not every possible combination has been adequately studied at this time. Some frequently used and/or well-studied combinations are:
Sulfonylurea with metformin
Sulfonylurea with insulin
Sulfonylurea with an alpha-glucosidase inhibitor
TZD with metformin
TZD with sulfonylurea
TZD with insulin
Metformin with gliptin
Metformin with an SGLT2 inhibitor
Insulin injection therapy was introduced as a treatment for diabetes in 1922. The major adverse effect of insulin therapy is hypoglycemia, and nearly all persons who inject insulin will experience hypoglycemia at some time. Another common adverse effect of insulin therapy is weight gain.
Usual causes of hypoglycemia include an excessive dosage of insulin, insufficient or delayed food intake to match insulin dosage, and/or too much physical activity in proportion to the amount of insulin taken. Symptoms of hypoglycemia may include any or all of the following [117]:
Shaking
Sweating
Weakness or fatigue
Anxiety or irritability
Rapid heartbeat
Headache
Hunger
Treatment of hypoglycemia consists of immediately ingesting 15–20 grams of fast-acting carbohydrate. Table 10 provides a list of foods that contain this amount of carbohydrate, along with patient instructions for treating and preventing hypoglycemia. Foods with high fat content, such as candy bars, cookies, and ice cream, are not recommended for the treatment of hypoglycemia because the fat will delay absorption of the food and slow down the response to treatment.
SAMPLE PATIENT INSTRUCTION SHEET: HYPOGLYCEMIA
|
WHAT SHOULD I DO IF I HAVE HYPOGLYCEMIA?
Note: If your blood sugar is less than 50 mg/dL you may need to consume twice as much of the food that is listed. | ||||
|
WHAT SHOULD I DO AFTER EATING SUGAR?
Eat your regular meals on schedule after treating hypoglycemia. | ||||
|
WHAT IF MY BLOOD SUGAR IS STILL LOW AFTER I EAT SUGAR?
| ||||
|
WHAT IF I BECOME UNCONSCIOUS OR CANNOT EAT?
| ||||
|
HOW CAN I PROTECT MYSELF FROM THE DANGERS OF HYPOGLYCEMIA?
|
An intramuscular injection of glucagon may be required to treat intractable or severe hypoglycemia in situations when the individual requires assistance. The action of glucagon is to raise blood glucose levels by causing the release of stored glucose from the liver. Blood glucose response usually occurs 5 to 20 minutes after injection. Glucagon is available as an emergency kit that contains the glucagon powder in a vial, along with a diluent-filled syringe and needle. This setup allows for rapid reconstitution of the powder and administration of the dissolved medication. One or more doses may be required to elicit a sufficient response from the patient. When consciousness is regained following administration of glucagon, the individual should be given glucose-containing liquids to restore glycogen stores in the liver and to prevent secondary hypoglycemia. Because nausea and vomiting are the most common side effects of glucagon, the patient should be protected from aspiration if convulsions occur and as consciousness resumes.
Insulin concentrations available in the United States include U100 and U500. However, U100 is used by virtually all patients. U500 insulin is a very concentrated form of insulin that is occasionally used in cases of extreme insulin resistance.
Human insulin and its analogs are the only species of insulin available in the United States today, as the manufacture of beef and pork insulins has been discontinued in this country. Human insulins are manufactured by using recombinant-DNA technology and are preferred over animal-derived insulins as they are less likely to produce antigenic reactions.
Insulin type usually refers to the action time of a particular product. This includes peak effect and duration of action. The currently available types of insulin are rapid-acting, short-acting, intermediate-acting, and long-acting.
Rapid-Acting
Examples of rapid-acting insulins are lispro and aspart. Their distinguishing characteristics are rapid onset, peak, and duration times. Aspart begins working about 5 to 15 minutes after injection, with peak action in one to three hours. The onset of action for lispro is 15 to 30 minutes, and peak effect is experienced in 30 minutes to 2.5 hours. Patients are instructed to inject rapid-acting insulin between 15 minutes and immediately prior to taking a meal. Administering sooner can result in profound hypoglycemia.
The major advantage to using rapid-acting insulin is that its action time parallels the action time for most meals. Therefore, when administered at the time that the person begins eating, it will lower blood glucose at the same time that food raises it. In addition, the short duration time means that its action is gone before the next meal begins. This means that less time is spent at high levels and there is less chance of hypoglycemia related to the overlapping build-up with longer-acting insulins.
For patients with diabetes, rapid-acting insulin offers the advantage of greater flexibility in meal and activity planning. Because the injection may be taken as a meal is begun, the user does not have to worry about unexpected delays that could occur during the wait period advised when regular insulin is used. Another advantage is that fewer episodes of nocturnal hypoglycemia are experienced by persons using rapid-acting insulin because the dinnertime dose will normally be out of the system by bedtime.
Short-Acting
Also known as "regular" insulin, this is a clear insulin that is generally used to cover increases in blood glucose associated with the main meals. Onset of action is from 30 minutes to one hour after injection, with peak levels occurring in two to three hours. Persons using regular insulin are instructed to administer a dose between 30 to 45 minutes prior to the meal.
A newer option is inhaled regular insulin administered prior to each meal [118]. In patients who have never taken insulin, the starting dose is 4 units at each meal. However, for persons who have been previously taking injected insulin, the number of units should be calculated based on previous mealtime doses [18]. Inhaled regular insulin carries a black-box warning that acute bronchospasm has been observed in individuals with asthma or chronic obstructive pulmonary disease, and it should not be used in these patients [18,119].
Intermediate-Acting
Neutral protamine Hagedorn (NPH) insulin is a cloudy suspension containing protamine and zinc to prolong the duration of action. Onset of action is one to two hours after administration, with peak action occurring in 4 to 12 hours. Intermediate-acting insulin may remain in the body for up to 24 hours after administration [18]. This type of insulin is frequently mixed with regular insulin and given twice a day.
Long-Acting
Insulin glargine, insulin detemir, and insulin degludec are newer long-acting insulins, providing benefits over their predecessor, Humulin U. The benefit of these agents is their "peakless" action over a 24-hour period, providing a basal pattern of insulin with a lower risk for hypoglycemia. They may be prescribed for once- or twice-daily dosing [18]. Because insulins glargine, detemir, and degludec provide only basal insulin coverage, they are usually used in combination with other insulin preparations or oral agents that will provide mealtime coverage. These insulins cannot be mixed in the same syringe with other insulins [18]. Because glargine is clear insulin with an action profile much different from the rapid- and short-acting insulins, it is dispensed in a vial that is longer and narrower to avoid administration errors. Insulin degludec should not be administered IV or IM or in an insulin infusion pump and should not be used if the solution is viscous or cloudy. The onset of action for both glargine and detemir is about three to eight hours after administration. The onset of action for degludec is about one hour [18].
Fixed Combination
Premixed insulins are available in combinations such as 70% NPH and 30% regular (70/30) and 75% intermediate-acting with 25% rapid-acting (75/25) [6]. Premixed formulas offer convenience to patients and are especially helpful to those who lack the visual, manual, or cognitive skills to mix insulin themselves. The convenience of these formulas sacrifice the potential for optimal blood glucose control, however, as there is less opportunity for flexible dosing based on need. Fixed ratio insulins are usually administered twice a day.
The most commonly used devices for insulin delivery include disposable syringes, insulin pens, and insulin pumps.
Syringes
Disposable plastic syringes are available in several sizes, including 1 cc, 0.5 cc, and 0.3 cc. The 0.5 cc size may be used for dosages of 50 units or less, while the 0.3 cc syringe has the capacity for doses equal to or less than 30 units. Smaller syringes offer several advantages. The major benefit is increased accuracy and reliability when delivering smaller doses because wider line markings are easier to see. Patients should be cautioned to check dosage lines carefully when changing syringes, as some use a scale of one-unit increments while others use a scale of two-unit increments.
Needles of newer syringes are designed for greater comfort to the user. Needles are sharper and thinner than ever before, and they are specially lubricated for comfort. Furthermore, some syringes have shorter needles, which many people find more comfortable. Patients and nurses should keep in mind that changing needle depth could change the rate of insulin absorption. Therefore, patients should consult with their healthcare provider before changing needle length and should monitor blood glucose levels carefully during this time.
The reuse of syringes is a controversial issue. Manufacturers of disposable syringes recommend single use only, while the ADA neither advocates nor prohibits this practice. Reusing needles may benefit some patients financially while helping to reduce medical waste. Recommendations for syringe reuse are intended for people who self-inject and who are capable of safely recapping a needle after each use. People who have poor personal hygiene, are acutely ill, have open wounds on the hands, or have decreased resistance to infection should not reuse their syringes. The ADA provides the following guidelines related to syringe reuse [120,121]:
Store the syringe at room temperature.
Recap the needle after each use.
Replace the syringe when the needle becomes dull or bent or has come into contact with anything other than the skin.
Inspect the skin around injection sites periodically for signs of infection.
Do not cleanse the needle with alcohol; this disrupts the silicone coating intended to make injection more comfortable.
Administration Procedures
The ADA guidelines for preparing a dose of insulin include ensuring that the hands and injection site are clean and that the cap of the insulin vial is wiped with alcohol prior to dosing. When using cloudy insulins, the vial should be gently rolled between the palms of the hands to resuspend the insulin. Injecting an amount of air into each vial that is equal to the dose of insulin is recommended to avoid creating a vacuum within the vial. When mixing two types of insulin in one syringe, the clear insulin should be drawn first. Air bubbles should be eliminated from the syringe to ensure that an accurate dose is administered [120].
Injection sites for insulin include the subcutaneous tissue of the upper arm, the anterior and lateral aspects of the thigh, the buttocks, and the abdomen, excluding a circle of two-inch diameter around the naval. Site selection will influence the absorption rate of the insulin. Absorption rates are fastest at the abdomen, followed by the arms, thighs, and buttocks. Therefore, it is suggested that the rotation of insulin injection sites should take place within the same anatomical area. For example, more consistent blood glucose levels may be achieved by using the abdominal site for all morning injections and the thighs for all evening injections.
Insulin injections are made into the subcutaneous tissue. Routine aspiration for blood prior to injecting the insulin is not necessary. The angle of the needle during injection should be individualized to avoid intramuscular injection. For most people, a subcutaneous injection can be achieved by grasping a fold of skin and injecting at a 90-degree angle. For those who are especially thin, the tissue should be lightly pinched and an injection angle of 45 degrees should be used [120].
Insulin Storage
The ADA recommends following the manufacturers' guidelines for storage of insulin vials currently in use. The patient should always have a spare bottle of insulin available. Vials of insulin that are not in current use should be stored in the refrigerator. Stored in this manner, they should remain potent until the expiration date [120].
Prefilled Syringes
Prefilled syringes are stable for up to 30 days when stored in the refrigerator. This may be beneficial to those who are sight-impaired or do not have the manual dexterity to fill their own syringes. In these cases, family members, friends, and other caregivers may prefill the syringes on a periodic basis. If possible, syringes prefilled with a cloudy insulin should be stored in a vertical position with the needle pointed up to avoid clumping of suspended insulins in the needle. Prefilled syringes should be gently rolled between the palms prior to injection to warm the refrigerated insulin and to resuspend insulin particles [120].
Insulin Pens
Disposable pens and refillable cartridge-type pens are available. Disposable pens are thrown away when empty, while empty cartridges are replaced in the refillable types. These devices allow the patient to dial the recommended dose of insulin and inject using standard technique. Screw-on disposable needles are available for both types of pens. Advantages of insulin pens are the convenience of portability and not having to fill a syringe from a vial. This benefits active people, working people, travelers, and those who do not have the manual dexterity to fill a syringe from a vial. Manufacturer instructions for some types of pens state that in-use (opened) pens should not be stored in the refrigerator. Patients should be referred to individual manufacturer instructions for proper insulin pen storage. Insulin pen aids should be considered for people with dexterity issues or vision impairment [6].
Newer generation insulin pens are reusable injector pens that come with an intuitive smartphone app to help people with diabetes better manage insulin delivery. This smart system calculates and tracks doses and provides helpful reminders, alerts, and reports. Smart insulin pens come either as an add-on to a regular insulin pen or as a reusable form that uses prefilled cartridges instead of vials or disposable pens [122].
Insulin Pumps
Insulin pumps, also referred to as continuous subcutaneous insulin infusion devices, have been available in the United States for more than 40 years [6]. They are the mainstay for management of type 1 diabetes. Insulin pumps are small, battery-operated microcomputers that resemble a standard pager device in size and appearance. Usually worn on the belt, the pump is connected via a small plastic tube to a subcutaneous catheter inserted through the skin into fatty tissue. The pump is programmed to deliver either a continuous infusion of insulin 24 hours a day, known as the "basal dose," or as a surge, known as the "bolus dose." For the bolus dose, the user programs the pump to deliver a bolus infusion of insulin appropriate to the amount of carbohydrate to be ingested [122].
In 2016, the FDA approved the first automated insulin delivery device for individuals 14 years of age and older with type 1 diabetes [123]. The MiniMed 670G, manufactured by Medtronic, is a hybrid closed-looped system that automatically monitors glucose and provides appropriate basal insulin doses. It measures glucose levels every five minutes and automatically administers or withholds insulin, depending on the level of glucose measured. The system includes a sensor that attaches to the user's body; an insulin pump that is strapped to the body; and an infusion patch that is connected to the pump with a catheter that delivers the insulin. The device requires little to no input from the user [123]. Medtronic's newest iteration, the MiniMed 780G system, tracks glucose levels via a smartphone and automatically delivers correction doses of insulin every five minutes [125].
A major advantage of insulin pumps is the opportunity for tight blood glucose control. This is possible because insulin delivery becomes very similar to the normal physiologic pattern. Pumps also offer the benefit of a more normal lifestyle, allowing users more flexibility with meal and activity patterns.
The ADA provides guidelines for the selection of patients appropriate for pump use [6,126]. Candidates should be highly motivated to take a great deal of responsibility for the care of their diabetes on a day-to-day basis. This includes the ability to count carbohydrate grams, to calculate appropriate bolus dosing, to make adjustments for varying activity patterns, and to monitor blood glucose four to seven times per day.
Adaptive Equipment
Several products are available for people with diabetes who are visually impaired or have other functional limitations. Many of these devices are available in local pharmacies that stock diabetes supplies. Others may be mail-ordered or located through the Internet. An annual resource guide is published in Diabetes Forecast, a magazine for people with diabetes that may be located on the Internet or through the ADA. Local chapters of the Braille Institute can also be contacted for assistance in locating adaptive equipment for the visually impaired. Briefly, some of the more commonly used assistive devices are:
Syringe magnifiers that enlarge the measure marks on the barrel of a syringe
Needle guides to help direct the needle into the vial stopper
Vial stabilizers, which can be mounted on a stable surface to hold the vial in place during needle insertion
Insertion aids used to hide the needle from view for those who are needle-phobic or to add bulk to the syringe for those who are unable to hold a fine syringe
Dose-measuring devices that assist the visually impaired person to draw the recommended amount of insulin into a syringe
Talking blood glucose meters, which produce audible test results and have tactile guides for test strip insertion
Patient R is a man, 49 years of age, with a 21-year history of type 1 diabetes. He is blind and lives alone without significant support from family or others. He also suffers from diabetic nephropathy and undergoes outpatient dialysis three times a week. He has been receiving home health nursing services for more than three years to assist with diabetes management.
Although Patient R has expressed appreciation for the support provided by the nurses, he is also resentful of their ongoing presence in his life. He longs for more privacy and more control over his own life and asks if there is any way that he can live more independently while maintaining his medical safety. The home health agency sends a nurse with strong diabetes management skills to Patient R's home to assess his potential for increased independence in the management of his diabetes.
Discussion
In her functional assessment, the nurse learns that, with adequate lighting, Patient R is able to see well enough to read a few words of large print with a magnifying glass. Other significant findings from a comprehensive needs assessment reveals that Patient R is able to:
Verbalize the correct dose and time of insulin injections
Inject insulin from a prefilled syringe safely and correctly
Perform the basic manual steps of blood glucose testing
Interpret blood glucose monitoring results as being high or low
Verbalize the correct action to take for hypoglycemia
Verbalize appropriate management of hyperglycemic emergencies
With these abilities in mind, the nurse is able to begin formulating a plan for Patient R. Although he demonstrates the cognitive and manual abilities needed for self-care, his severe visual limitations must be addressed before he is considered safe to manage these tasks on his own.
One area of challenge for Patient R is related to measuring the insulin dose in the syringe. The nurse's initial approach is to observe the patient while he draws an insulin dose using syringes with the largest increment markings available. Because Patient R is on insulin doses of less than 30 units, he is able to practice using a 0.3-cc syringe. Not surprisingly, he is unable to see these syringe markings well enough to draw an accurate dose. Next, the nurse has Patient R try the same syringe using a magnifier. Even with this adaptive aid, he is still unable to consistently draw an accurate dose. The nurse concludes that it will be necessary to make arrangements for the patient's syringes to be prefilled by a sighted person and stored in the refrigerator for later use.
The nurse then considers the type and amount of insulin that Patient R is using. As a matter of convenience, he is using premixed 70/30 insulin, receiving 14 units in the morning and 7 units in the evening. Because he would be injecting different doses of insulin in the morning and evening, it is necessary to ensure that Patient R is able to distinguish between the two differently dosed prefilled syringes. This is accomplished using two glass jars, dissimilar in size and shape, to store the prefilled syringes. Each jar is then labeled in large letters using a bold black marking pen as "MORN" and "EVE." The nurse avoids using the abbreviations "am" and "pm" because of their similarity. She then works with Patient R on a plan to place a predetermined number of prefilled syringes in each jar, with the capped needles facing upward. The patient shows her where and how the syringes should be stored in the refrigerator to maximize his ease of use and minimize potential error.
Patient R's needs assessment has already determined that he is well versed in insulin administration practices. Therefore, the nurse has only to review those techniques with him and verify his competence by having him give a return demonstration. Part of her review includes reminding him to roll the prefilled insulin syringe gently between his palms prior to injection. She also verifies his ability to select the appropriate dose from the jars in the refrigerator and to select an appropriate injection site. She suggests an injection technique of gently placing the needle on the skin before inserting it, rather than using the conventional dart-like approach. This allows him better control over the site of injection.
The next challenge for Patient R is related to blood glucose monitoring. Although he has a meter that he is comfortable using, he is unable to read the results display accurately. The nurse discusses with him the possibility of trying a talking meter. The patient expresses that, because he is already familiar with his current meter, he would prefer to continue using it with a display magnifier if possible. The problem he perceives, however, is that the magnifying glass he is currently using is not sufficient for this procedure. To address this challenge, the nurse refers Patient R to the local chapter of the Braille Institute. Here, specialists are available to supply him with a prescription magnifier that is adaptable for use with his current meter. After receiving this device, the nurse works with the patient to ensure that he is able to accurately read the results displayed on his meter.
Although Patient R initiated these changes in his care because he desired more independence, the transition period is a time of anxiety on his part. After three years of having the security of a nursing visit twice a day, Patient R begins to question his ability to manage safely with less frequent nursing contacts. His concern is validated by the fact that he lives alone and does not have a significant other. It is important at this point to work with the patient and his physician on a plan for future nursing service that would ensure his safety while affording him the independence that he desires. Because he is socially isolated, it is agreed that Patient R should have face-to-face contact with medical personnel once a day. It is determined that outpatient dialysis appointments would meet this need for three days of each week. For the remaining four days of the week, a nurse would visit him at home. The purpose of these visits would be to perform a skilled assessment of the patient's current status and to ensure his medical safety on a daily basis. These nursing visits would include a review of Patient R's blood glucose results using the memory function of his meter. Syringes would be prefilled as needed. Periodically, the nurse would observe the patient performing his self-care procedures to ensure that changes in his functional ability had not occurred. The nursing service would continue to be available to Patient R 24 hours a day by telephone, with additional nursing visits made as needed. A medical social worker is involved in providing the patient with community resources and helping him obtain a diabetes identification bracelet.
This case demonstrates a problem-solving approach to diabetes self-management that promotes the independence of a visually impaired person with diabetes. While issues of medical safety are always paramount, other factors should be considered when developing a plan of care for the visually impaired patient. These factors include the patient's willingness and ability to become more independent, his baseline knowledge, and experience of diabetes self-care and resources available. In the case of Patient R, a safe and viable plan was developed that resulted in greater independence and promoted his sense of well-being.
Physical activity is considered an important component of any diabetes management program. The primary benefit of exercise to people with diabetes is that it has been found to increase glucose utilization by the tissues, thereby lowering blood glucose concentration [6,127]. In some people with type 2 diabetes, a regular program of physical activity can increase insulin sensitivity to the degree that medications can be reduced or discontinued. Because people with diabetes are at increased risk for heart disease, exercise has the added benefit of its favorable effect on cardiovascular status. The benefits of regular exercise to people with diabetes can be summarized as [127]:
Improved insulin sensitivity
Reduction in body fat and weight
Reduction in incidence of cardiac disease
Improved lipid profile
Increase in high-density lipoproteins
Improved control of hypertension
Improved self-esteem
Reduced psychologic stress
The ADA, along with other authorities, recommends at least 150 minutes of moderate intensity aerobic exercise per week [127,128]. Because reduction in insulin resistance from a single bout of exercise lasts for 24 to 72 hours afterward, there should be no more than two consecutive days without aerobic activity [127]. Research also supports resistance training as an effective exercise for people with diabetes, leading to better glucose control and less insulin resistance among adults with type 2 diabetes [127,129].
It is important to inform patients that assuming a more active lifestyle does not necessarily mean that they must adopt a structured exercise program. Experts advocate the benefits of incorporating moderate-intensity exercise into everyday activities. For example, making it a habit to use stairs instead of an elevator on a regular basis contributes to a more active lifestyle with cardiovascular benefits. Likewise, keeping active by doing such routine tasks as walking the dog, raking leaves, or washing the car can also be beneficial. It is suggested that, if done in increments lasting at least 10 minutes per session, with an accumulation of 30 minutes or more per day, these types of activities per day can increase overall health and fitness [128].
Although physical activity can provide health benefits to a variety of patients, it does carry some potential health risks for people with diabetes, although the risk varies. For adults with type 2 diabetes, the risk of adverse events from low-to-moderate-intensity activity is low. Because no current evidence suggests that any screening protocol beyond usual diabetes care reduces the risk of exercise-induced adverse events in asymptomatic individuals, the ADA states that pre-exercise clearance is unnecessary, except for individuals who plan to increase exercise intensity or who meet higher-risk criteria. These individuals may benefit from pre-exercise checkup and possible exercise stress test. Routine stress testing is not recommended [127]. To ensure a safe and effective exercise regimen, most adults with diabetes may benefit from working with an exercise physiologist or certified fitness professional proficient in diabetes knowledge.
Patients who use insulin or sulfonylureas are at risk for hypoglycemia during or after exercise if proper adjustments are not made. This is due to the effect that exercise has on lowering blood glucose. People who use meal planning alone to control their diabetes are not generally at risk for experiencing exercise-induced hypoglycemia.
Several factors influence the blood glucose response to exercise, including the timing, amount, and intensity of the exercise. Patients at risk for hypoglycemia are advised to carefully monitor their blood glucose before and after exercise to determine their response to a particular activity. Adjustments to medications and/or food intake can then be made prior to exercise based upon these findings.
The risk for exercise-related hypoglycemia can be reduced if the patient follows a consistent pattern of activity, occurring at about the same time every day and of similar intensity. The following instructions to patients will help minimize the risk for developing exercise-induced hypoglycemia:
Monitor blood glucose before and after activity.
Be consistent in the timing of insulin injections and activity.
Take a pre-exercise snack if blood glucose is less than 100 mg/dL.
Carry a fast-acting carbohydrate while exercising.
Wear diabetes identification.
Exercise with someone who knows how to recognize and treat hypoglycemia.
If using insulin, learn to safely make adjustments in dose before exercising.
General recommendations for people with diabetes who exercise include:
Use appropriate footwear: athletic shoes with silica gel or air midsoles and socks of polyester or cotton-polyester blend to prevent blisters.
Monitor feet closely before and after exercise for injury.
Ensure proper hydration. Drink adequate and appropriate fluid two hours before exercise and consume enough fluid during exercise to compensate for losses.
Avoid exercising in extremely hot or cold conditions.
Although most people with diabetes can derive some benefit from exercise, several risk factors may modify their activity plan. The nurse should consult with the physician before discussing an activity plan with patients having any of the identified comorbidities.
Cardiovascular Disease
Silent angina is more common in people with diabetes than the general population. Risk factors include age older than 35 years and diabetes of greater than 10 to 15 years duration. The physician may order a graded exercise test to detect the presence of heart disease before prescribing an exercise program to diabetic patients.
Peripheral Vascular Disease
Patients with this condition, whether of venous or arterial origin, should avoid exercise that may traumatize the foot.
Retinopathy
Patients with proliferative retinopathy should avoid high-resistance exercise, such as lifting heavy weights. They should also avoid activities that produce the Valsalva maneuver and those that require lowering the head below the waist.
Peripheral Neuropathy
Patients with peripheral neuropathy should avoid weight-bearing exercise that can cause orthopedic stress to the foot. They should also avoid activities that may cause mechanical trauma to the skin of the lower extremities. Such activities include prolonged walking, jogging, or step exercises. Recommended exercises for those with peripheral neuropathy may include swimming, bicycling, and chair exercises [127].
Exercise and the Elderly
Elderly people without significant physical limitations can generally participate in the same types of activity as younger people, as long as it is approved by the physician and is modified to meet the needs of the individual. For seniors who are currently sedentary, it is recommended that they add a few minutes of increased activity each day and gradually build up to an accumulated 30 minutes of physical activity. For those without significant functional limitations, this may include light housework and short walks. For seniors who are already moderately active, appropriate exercise may include a paced walking program, low-impact aerobics, or swimming. As with younger people, elderly patients require education about the risks and benefits of exercise and instruction on prevention and treatment of exercise-induced hypoglycemia.
Activity programs can be designed to meet the needs of elderly people who have varying degrees of physical limitation. For example, for a person who is chair-bound, chair exercises may be appropriate. These may include "marching" in place or repetitively reaching toward the ceiling with the arms. Resistance can be added by holding 6-ounce soup cans or paper plates during the exercises. There are several commercially available videotapes for senior chair exercises that include music and demonstrations.
Foot pathology is a common complication of diabetes, and related outcomes frequently include hospitalization, disability, and death. Lower extremity amputation, the most dreaded consequence of diabetic foot disease, will occur in about 20% of individuals with diabetes in their lifetimes. Of those who require below the knee amputation, an estimated 10% will die within two years [130]. In spite of these grim statistics, preventive foot care can significantly reduce the morbidity of diabetic foot disease. Approaches such as patient education, provision of proper footwear, and medical follow up are significant factors in the prevention of foot-related morbidity and mortality in people with diabetes [131,132].
Multiple and complex pathologic processes are involved in the development of diabetic foot disease. The presence of three specific conditions, peripheral sensory neuropathy, vascular disease, and immune deficiency related to elevated blood glucose, is implicated in the majority of cases. These risk factors make the diabetic foot more vulnerable to mechanical stresses that can lead to skin breakdown and poor healing [133]. Diabetic foot amputations are often precipitated by minor preventable foot trauma, such as a blister from poorly fitting shoes or inappropriate care of toenails. If sensory neuropathy is present, the patient may not perceive that an injury has occurred. When the neuropathic wound is complicated by vascular disease, serious problems with wound healing may result. The environment provided by a poorly healing wound then presents significant opportunity for an infectious process to develop. This opportunistic environment can be further complicated by impaired host defenses when blood glucose is elevated.
Although diabetic foot ulcers should always be taken very seriously, proper wound management can heal many foot ulcers. All ulcers should be thoroughly evaluated to determine etiology and course of treatment.
The value of preventive foot care cannot be overestimated. Preventive care includes daily self-foot exams, proper foot care, proper footwear, and regular foot exams by a healthcare professional.
Daily Self-Foot Exam
Patients should be instructed in how to perform a daily foot exam. A return demonstration should be requested to ensure that the patient is able to reach and see the bottoms of the feet. The self-foot exam includes inspection of the tops, bottoms, and sides of each foot and between the toes. A mirror can be used to see less accessible areas of the foot if necessary. Family members or caregivers may need to be involved. Patients should seek prompt professional advice for any foot problems including corns, calluses, open areas, nail deformities, or cracks and fissures in the skin.
Proper Foot Care
Foot care for people with diabetes includes keeping the feet clean and dry and avoiding trauma to intact skin. Feet should be cleansed daily, but not soaked, and dried well, especially between the toes. Unscented, non-alcohol-based moisturizing lotions are recommended to keep the skin soft and supple. Avoiding lotion between the toes prevents excessive moisture build up that could promote the development of fungal infections.
Trauma to the foot can be avoided by wearing well-fitting protective footwear at all times. People with diabetes should be instructed to check the insides of shoes for foreign objects before putting them on. Feet should be inspected immediately after wearing new shoes for areas of pressure or blisters. Clean, well-fitting socks that do not wrinkle or bind are recommended. Other footwear recommendations include [132]:
Shoes should have flexible soles and padded insoles.
Shoes should have plenty of toe room.
Shoe-wearing time should be alternated so that no pair is worn for more than five hours at a time.
New shoes should never be worn for more than one to two hours at a time, and the foot should be inspected immediately after the shoes are removed.
Clinical Foot Exam
The ADA recommends that people with diabetes receive a thorough clinical foot exam by a qualified healthcare professional at least once a year [6]. Patients with high-risk conditions, such as loss of protective sensation, structural abnormalities of the feet, and compromised vascularity, should have their feet examined at every office visit [6].
The annual clinical foot exam should include sensory testing with a monofilament to detect loss of protective sensation. This is a simple and noninvasive method for identifying feet that are at risk for problems that could lead to amputation [6]. The test is done using a monofilament that resembles the bristle of a hairbrush. The monofilament is pressed onto specific areas on the plantar surface of the feet while the patient has his or her eyes closed. The patient then indicates whether or not the monofilament is felt, indicating the presence or absence of protective sensation. When protective sensation has been lost, there is an increased risk for amputation and the patient should be counseled on the importance of vigilant preventive measures. In some cases, custom-fit shoes are required for those who have lost protective sensation [6].
Both physical and psychologic stress can influence blood glucose control. Examples of physical stressors include illness, injury, and fatigue. Psychologic stress is commonly manifested by such feelings as anger, worry, fear, and anxiety.
When asked what it feels like to experience stress, most people would respond with descriptions of feeling nervous, sweaty, or shaky, and perhaps experiencing dry mouth, a pounding heart, or "butterflies in the stomach." These common reactions to stress are known as the "fight or flight response," and they reflect the response of the sympathetic nervous system to stress. Hormones released during the sympathetic stress response make diabetes more difficult to control. These hormones include epinephrine, norepinephrine, glucagon, and growth hormone. Another stress hormone, cortisol, plays an important role in diabetes, as it stimulates glucose production by the liver in addition to increasing insulin resistance. In the person with diabetes, this will have the effect of raising blood glucose.
Physiologic stress, such as concurrent illness, infection, surgery, or trauma, can disrupt homeostasis and lead to loss of blood sugar control in the person with diabetes. All patients with diabetes should be educated with regard to the risks involved during illness. This should include instruction on appropriate sick day management, as previously noted.
While minor illness can usually be managed safely at home through telephone contact with a physician, certain conditions will require the immediate attention of a healthcare provider [6]. These include:
Vomiting or diarrhea for more than six hours
Difficulty breathing
If on insulin: Blood glucose greater than 240 mg/dL that is unresponsive to insulin
If using oral diabetes medications: Blood glucose before meals greater than 240 mg/dL for 24 hours or more
Moderate or large ketones in the urine
Change in mental status
Fever for more than two days
Psychologic stress in general can also have an undesirable effect on blood glucose control, in many of the same ways as physiologic stress. General psychologic stress can be brought on by significant life events, such as the death of a spouse, changing jobs, or dealing with a loved one's illness. It can also be related to other life factors, such as economic hardship, pressures at work, interpersonal relationships, or family dynamics.
One way of mediating the negative effects of stress on health can be to limit the number or intensity of stressors that one experiences. Because this is not always possible, learning how to cope with stress is another way of curbing its adverse effects upon health.
Certain techniques and behaviors can be encouraged to help the patient cope with stress. Keeping a stress diary may help some patients identify events that can trigger the stress response. Patients can use their blood glucose logs to keep track of stressful events and feelings. Correlating these events and feelings with blood glucose results may help the patient monitor the effect of stress on blood glucose control.
Another suggestion for reducing stress is to help patients prioritize the demands in their lives. By doing this, the person may be able to realize that some things are of less importance and can be given up or delegated to someone else. By doing fewer things, it is more likely that the person can address the more important tasks fully and will experience a greater degree of satisfaction.
Directing stress-related energy toward something more positive is also advocated as a technique for reducing stress. Activities that may effectively reduce feelings of stress include engaging in exercise, hobbies, or other pursuits of interest.
Techniques such as progressive relaxation and guided visual imagery are generally accepted as effective stress-reduction methods. Several audio tapes and books are available that provide scripts for delivering these techniques. Furthermore, many professional therapists utilize these methods, and they should be recommended when the patient does not have the resources for dealing with stress on his or her own.
In addition to the general stressors that most people face, people with diabetes experience specific feelings, frustrations, and emotional struggles that can be directly related to having the disease. This so-called "diabetes-burnout" is believed to be very common. Feelings frequently reported by subjects with diabetes have included guilt or anxiety for not always following the treatment plan and worry about the possibility of serious long-term complications. Other feelings related to having diabetes include helplessness, depression, anger, and being overwhelmed. These difficult feelings about diabetes along with poor coping skills are believed to be among the greatest obstacles to satisfactory self-care [43].
"Diabetes distress" is a term used to describe the psychologic effects (worries and fears) of patients with diabetes. It is distinct from other psychologic disorders [6]. It is associated with poorer health and is most common in those who use insulin [134].
As society becomes increasingly diverse, nurses are encountering a wide variety of cultural values and perceptions that influence health behavior in individuals and families. Because culture can have a strong influence on a patient's response to nursing interventions, nurses should be continually aware of these influences. While cultural competence is important in all nursing settings, it has special relevance for the diabetes care provider. This is due to the high prevalence of diabetes among such diverse ethnic groups as Hispanics, Native Americans, non-Hispanic Black Americans, and Pacific Islanders.
Cultural competence means being sensitive to differences in the values and beliefs that are shared by the members of an ethnic, cultural, racial, religious, or lifestyle preference of a group. Components of effective transcultural nursing include communication style, use of personal space, eye contact, and understanding of biologic variations. It is important to keep in mind, however, that there can be great variation among individuals within cultures. Therefore, stereotyping and making assumptions about an individual patient's beliefs based solely upon ethnic identification should be avoided.
In most cases, it is not necessary to develop a thorough understanding of each and every culture encountered in diverse healthcare settings. However, a certain degree of cultural competence can and should be developed. The first step in doing this is to recognize that cultural differences do exist. How these variations impact diabetes self-management can be explored in the diabetes needs assessment. This may include a sensitive exploration of the person's healthcare practices and the role of family members. Other culturally impacted areas may include beliefs about illness, diet, the role of the patient in self-care, gender roles, religious rituals, and communication styles.
Dietary preferences, meal preparation practices, and the symbolism of food represent an especially important area for the diabetes healthcare provider. When giving diet instructions, efforts should be made to consider the food preferences of the cultural group. Nutritional resources that are especially designed for members of different cultural groups are available from the ADA and the Academy of Nutrition and Dietetics.
Cultural competence includes recognizing that cultural healthcare practices may differ from one's own beliefs about how an illness should be treated. Furthermore, cultural influences may not always be consistent with healthcare recommendations. This may be especially true with diabetes, as this disease requires significant behavioral adaptations. For example, an Hispanic American woman with diabetes may experience a conflict between her cultural gender role and dietary recommendations made by a healthcare provider. For many Hispanic Americans, a valued role for the woman is to prepare large traditional meals for the family. Americanized versions of many of these traditional foods, however, are high in fat and calories and are not recommended for people with diabetes. Therefore, the woman may experience a conflict between her cultural values and those of the mainstream healthcare system.
Nursing competencies related to teaching diabetes self-management have been the focus of this continuing education course. A comprehensive set of examples that can be utilized by nurses in a variety of clinical practice settings has been presented.
Diabetes disease management has been discussed in terms of four cornerstones of care: nutrition, medications, activity, and stress management. These have been presented along with related aspects of blood glucose control and monitoring. A detailed discussion of the diabetes disease process has included the acute and chronic complications of the disease and the clinical aspects of care. This clinical overview has been provided to establish a solid clinical foundation for teaching patients diabetes self-management skills.
Equally important to the clinical aspects of diabetes care, the vital role of the nurse as teacher has been addressed. In a holistic approach to diabetes care, the principles of adult learning have been presented. In this context, nurses can present clinical knowledge to patients in a way that will empower them to become informed decision-makers.
To complete the holistic approach to diabetes care, this course has addressed such frequently encountered psychosocial issues as coping, self-efficacy, readiness to change, and stress. The aim has been to provide information that will help nurses link the clinical competencies of diabetes care with psychosocial interventions. When coupled with sensitivity toward individual and cultural characteristics, this approach to the patient will enable the nurse to provide diabetes care that encompasses the needs of the total person.
| Academy of Nutrition and Dietetics |
| 1-800-877-1600 |
| https://www.eatright.org |
| American Association of Diabetes Care and Education Specialists |
| 1-800-338-3633 |
| https://www.diabeteseducator.org |
| American Diabetes Association |
| 1-800-342-2383 |
| https://www.diabetes.org |
1. Centers for Disease Control and Prevention. National Diabetes Statistics Report. Available at https://www.cdc.gov/diabetes/php/data-research/index.html. Last accessed November 3, 2025.
2. Centers for Disease Control and Prevention. About the Division of Diabetes Translation. Available at https://www.cdc.gov/nccdphp/divisions-offices/about-the-division-of-diabetes-translation.html?CDC_AAref_Val=https://www.cdc.gov/chronicdisease/resources/publications/aag/diabetes.htm. Last accessed November 3, 2025.
3. Dall TM, Zhang Y, Chen YJ, Quick WW, Yang WG, Fogli J. The economic burden of diabetes. Health Aff (Millwood). 2010;29(2):297-303.
4. American Diabetes Association. New American Diabetes Association Report Finds Annual Costs of Diabetes to be $412.9 Billion. Available at https://diabetes.org/newsroom/press-releases/new-american-diabetes-association-report-finds-annual-costs-diabetes-be. Last accessed November 3, 2025.
5. Davis J, Fischl AH, Beck J, et al. 2022 National standards for diabetes self-management education and support. Diabetes Care. 2022;45(2):484-494.
6. American Diabetes Association. Standards of care in diabetes—2025. Diabetes Care. 2025;48(Suppl 1):S1-S344.
7. Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977-986.
8. American Diabetes Association. Implications of the United Kingdom prospective diabetes study. Diabetes Care. 2002;25(Suppl 1):S28-S32.
9. Skyler JS, Bergenstal R, Bonow RO, et al. Intensive glycemic control and the prevention of cardiovascular events: implications of the ACCORD, ADVANCE, and VA diabetes trials. Circulation. 2009;119(2):351-357.
10. American Diabetes Association. Statistics About Diabetes. Available at https://diabetes.org/about-diabetes/statistics/about-diabetes. Last accessed November 3, 2025.
11. Narayan KM, Boyle JP, Thompson TJ, Sorensen SW, Williamson DF. Lifetime risk for diabetes mellitus in the United States. JAMA. 2003;290(14):1884-1890.
12. Fradkin J, Rodgers GP. The economic imperative to conquer diabetes. Diabetes Care. 2008;31(3):624-625.
13. National Indian Council on Aging, Inc. Diabetes Still Highest Among AI/AN. Available at https://www.nicoa.org/diabetes-still-highest-among-ai-an/#. Last accessed November 3, 2025.
14. Roberts H, Jiles R, Mokdad A, Beckles G. Rios-Burrows N. Trend analysis of diagnosed diabetes prevalence among American Indian/Alaska Native young adults—United States, 1994–2007. Ethnicity Disease. 2009;19:276-279.
15. U.S. Department of Health and Human Services, Office of Minority Health. Diabetes and Black/African Americans. Available at https://minorityhealth.hhs.gov/diabetes-and-blackafrican-americans. Last accessed November 3, 2025.
16. U.S. Department of Health and Human Services, Office of Minority Health. Diabetes and Hispanic/Latino Americans. Available at https://minorityhealth.hhs.gov/diabetes-and-hispaniclatino-americans. Last accessed November 3, 2025.
17. U.S. Department of Health and Human Services, Office of Minority Health. Diabetes and Asian Americans. Available at https://minorityhealth.hhs.gov/diabetes-and-asian-americans. Last accessed November 3, 2025.
18. LexiDrug. Available at https://online.lexi.com/lco/action/login. Last accessed November 3, 2025.
19. DeFronzo RA, Eldor R, Abdul-Ghani M. Pathophysiologic approach to therapy in patients with newly diagnosed type 2 diabetes. Diabetes Care. 2013;36(Suppl 2):S127-S138.
20. Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2012;35(6):1364-1379.
21. Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Eng J Med. 2002;346(6):393-403.
22. National Diabetes Prevention Program. Preventing Type 2 Diabetes with the Lifestyle Change Program. Available at https://www.cdc.gov/diabetes-prevention/lifestyle-change-program/?CDC_AAref_Val=https://www.cdc.gov/diabetes/prevention/why-participate.html. Last accessed November 3, 2025.
23. National Institute of Diabetes and Digestive and Kidney Diseases. Pancreatic Islet Transplantation. Available at https://www.niddk.nih.gov/health-information/diabetes/overview/insulin-medicines-treatments/pancreatic-islet-transplantation. Last accessed November 3, 2025.
24. American Diabetes Association. Gestational Diabetes. Available at https://www.diabetes.org/diabetes/gestational-diabetes. Last accessed November 3, 2025.
25. Centers for Disease Control and Prevention. Diabetes Risk Factors: Gestational Diabetes. Available at https://www.cdc.gov/diabetes/risk-factors/?CDC_AAref_Val=https://www.cdc.gov/diabetes/basics/risk-factors.html. Last accessed November 3, 2025
27. Noctor E, Crowe C, Carmody LA, et al. Abnormal glucose tolerance post-gestational diabetes mellitus as defined by the International Association of Diabetes and Pregnancy Study Groups criteria. Eur J Endocrinol. 2016;175:287-297.
28. Kim C, Newton KM, Knopp RH. Gestational diabetes and the incidence of type 2 diabetes: a systematic review. Diabetes Care. 2002;25:1862-1868.
29. American Diabetes Association. How to Treat Gestational Diabetes. Available at https://diabetes.org/living-with-diabetes/pregnancy/gestational-diabetes/how-to-treat-gestational-diabetes. Last accessed November 3, 2025.
30. American Diabetes Association. Diabetes and DKA (Ketoacidosis). Available at https://diabetes.org/about-diabetes/complications/ketoacidosis-dka/dka-ketoacidosis-ketones. Last accessed November 3, 2025.
31. Centers for Disease Control and Prevention. Diabetic Ketoacidosis. Available at https://www.cdc.gov/diabetes/about/diabetic-ketoacidosis.html?CDC_AAref_Val=https://www.cdc.gov/diabetes/basics/diabetic-ketoacidosis.html. Last accessed November 3, 2025.
32. Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN. Hyperglycemic crises in adult patients with diabetes. Diabetes Care. 2009;32(7):1335-1343.
33. Davidson MB, Scwartz S. Hyperglycemia. In: Franz MJ (ed). A Core Curriculum for Diabetes Education: Diabetes and Complications. 5th ed. Chicago, IL: American Association of Diabetes Educators; 2003.
34. American Diabetes Association. Economic costs of diabetes in the U.S. in 2022. Diabetes Care. 2022;47(1):26-43.
35. Centers for Disease Control and Prevention. Diabetes Complications. Available at https://www.cdc.gov/diabetes/complications/?CDC_AAref_Val=https://www.cdc.gov/diabetes/managing/problems.html. Last accessed November 3, 2025.
36. National Institute of Diabetes and Digestive and Kidney Diseases. Blood Glucose Control Studies for Type 1 Diabetes: DCCT and EDIC. Available at https://www.niddk.nih.gov/about-niddk/research-areas/diabetes/blood-glucose-control-studies-type-1-diabetes-dcct-edic. Last accessed November 3, 2025.
37. Fang M, Wang D, Coresh J, Selvin E. Trends in diabetes treatment and control in U.S. adults, 1999-2018. New Engl J Med. 2021;384:2219-2228.
39. Sharma AM, Weir MR. The role of angiotensin receptor blockers in diabetic nephropathy. Postgrad Med. 2011;123(3):109-121.
40. Mayo Clinic. Diabetic Neuropathy. Available at https://www.mayoclinic.org/diseases-conditions/diabetic-neuropathy/symptoms-causes/syc-20371580#. Last accessed November 3, 2025.
41. Dal Canto E, Ceriello A, Ryden L, et al. Diabetes as a cardiovascular risk factor: an overview of global trends of macro and micro vascular complications. Eur J Preventive Cardiol. 2019;26(2):25-32.
42. Kearney PM, Blackwell L, Collins R, et al. Cholesterol Treatment Trialists' (CTT) Collaborators. Efficacy of cholesterol-lowering therapy in 18,686 people with diabetes in 14 randomized trials of statins: a meta-analysis. Lancet. 2008;371(9607):117-125.
43. Polonsky WH. Diabetes Burnout: What to Do When You Can't Take It Anymore. Alexandria, VA: American Diabetes Association; 1999.
44. Rubin RR, Napora JP. Psychosocial assessment. In: Franz MJ (ed). A Core Curriculum for Diabetes Education: Diabetes and Complications. 5th ed. Chicago, IL: American Association of Diabetes Educators; 2003.
45. Prochaska JO, DiClemente CC. Common processes of self-change in smoking, weight control, and psychological distress. In: Shiffman S (ed). Coping and Substance Abuse: A Conceptual Framework. New York, NY: Academic Press; 1985: 345-363.
47. Duncan I, Birkmeyer C, Coughlin S, Li QE, Sherr D, Boren S. Assessing the value of diabetes education. Diabetes Educ. 2009;35(5):752-760.
48. U.S. Department of health and Human Services. Healthy People 2030. Available at https://health.gov/healthypeople. Last accessed November 3, 2025.
49. Centers for Disease Control and Prevention. Diabetes Self-Management Education and Support. [Archive]. Available at https://archive.cdc.gov/#/details?q=https://www.cdc.gov/diabetes/library/reports/reportcard/diabetes-self-management-education-support.html&start=0&rows=10&url=https://www.cdc.gov/diabetes/library/reports/reportcard/diabetes-self-management-education-support.html. Last accessed November 3, 2025.
50. International Diabetes Federation. IDF Global Clinical Practice Recommendations for managing Type 2 Diabetes 2025. Available at https://idf.org/media/uploads/2025/04/IDF_Rec_2025.pdf. Last accessed November 3, 2025.
51. Martin S, Schneider B, Heinnemann L, et al. Self-monitoring of blood glucose in type 2 diabetes and long-term outcome: an epidemiological cohort study. Diabetologia. 2006;49(2):271-278.
52. Saudek CD, Derr RL, Kalyani RR. Assessing glycemia in diabetes using self-monitoring blood glucose and hemoglobin A1c. JAMA. 2006;295(14):1688-1697.
53. Malanda UL, Welschen LMC, Riphagen II, Dekker JM. Self-monitoring of blood glucose in patients with type 2 diabetes mellitus who are not using insulin. Cochrane Database Syst Rev. 2012;(1):CD005060.
54. DTS Blood Glucose Monitoring System Surveillance Program. Available at https://www.diabetestechnology.org/surveillance.shtml. Last accessed November 3, 2025.
55. American Diabetes Association. Check Your Blood Glucose: Diabetes Testing and Monitoring. Available at https://diabetes.org/living-with-diabetes/treatment-care/checking-your-blood-sugar. Last accessed November 3, 2025.
56. Cox DJ, Taylor AG, Moncrief M, et al. Continuous glucose monitoring in the self-management of type 2 diabetes: a paradigm shift. Diabetes Care. 2016;39(5):e71-e73.
57. U.S. Food and Drug Administration. Archive: Press Release. FDA Approves Pediatric Use of Dexcom's G4 Platinum Continuous Glucose Monitoring System. Available at https://wayback.archive-it.org/7993/20170112222919/http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm384495.htm. Last accessed November 3, 2025.
58. Kapstone Medical. Resource Center. FDA Approves First Continuous Glucose Monitoring System Not Requiring Blood Sample Calibration. Available at https://www.kapstonemedical.com/resource-center/blog/fda-approves-first-continuous-glucose-monitoring-system-not-requiring-blood-sample-calibration. Last accessed November 3, 2025.
59. Abbott. Abbott's Freestyle Libre 2 ICGM Cleared in U.S. for Adults and Children with Diabetes, Achieving Highest Level of Accuracy and Performance Standards. Available at https://abbott.mediaroom.com/2020-06-15-Abbotts-FreeStyle-R-Libre-2-iCGM-Cleared-in-U-S-for-Adults-and-Children-with-Diabetes-Achieving-Highest-Level-of-Accuracy-and-Performance-Standards. Last accessed November 3, 2025.
60. Black E. Abbott Has a New Glucose Monitor for Diabetics – It's So Small I Forgot I Was Wearing It. Available at https://www.cnbc.com/2022/10/14/review-abbott-freestyle-libre-3-cgm-for-diabetics-.html. Last accessed November 3, 2025.
61. Tucker ME. FDA Approves New 'Smart' Continuous Glucose Monitor for Diabetes. Available at https://www.medscape.com/viewarticle/893851. Last accessed November 3, 2025.
62. PR Newswire. FDA Authorizes First Fully Interoperable Continuous Glucose Monitoring System, Streamlines Review Pathway for Similar Devices. Available at https://www.prnewswire.com/news-releases/fda-authorizes-first-fully-interoperable-continuous-glucose-monitoring-system-streamlines-review-pathway-for-similar-devices-300620505.html. Last accessed November 3, 2025.
63. U.S. Food and Drug Administration. Eversense E3 Continuous Glucose Monitoring (CGM) System – P160048/S021. Available at https://www.fda.gov/medical-devices/recently-approved-devices/eversense-e3-continuous-glucose-monitoring-cgm-system-p160048s021. Last accessed November 3, 2025.
64. Cardiometabolic Health Congress. FDA Approves First Year-Long Continuous Glucose Monitoring Sensor for Diabetes. Available at https://www.cardiometabolichealth.org/fda-approves-first-year-long-continuous-glucose-monitoring-sensor-for-diabetes. Last accessed November 3, 2025.
65. U.S. Food and Drug Administration. FDA News Release: FDA Clears First Over-the-Counter Continuous Glucose Monitor. Available at https://www.fda.gov/news-events/press-announcements/fda-clears-first-over-counter-continuous-glucose-monitor#. Last accessed November 3, 2025.
66. Doyle-Delgado K, Chamberlain JJ. Use of diabetes-related applications and digital health tools by people with diabetes and their health care providers. Clin Diabetes. 2020;38(5):449-461.
67. American Diabetes Association. A1C and eAG. Available at https://diabetes.org/a1c-eag-conversion-calculator. Last accessed November 3, 2025.
68. GBD 2016 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1345-1422.
69. Pan A, Lin X, Hemler E, Hu FB. Diet and cardiovascular disease: advances and challenges in population-based studies. Cell Metab. 2018;27(3):489-496.
70. Ley SH, Hamdy O, Mohan V, Hu FB. Prevention and management of type 2 diabetes: dietary components and nutritional strategies. Lancet. 2014;383(9933):1999-2007.
71. Joslin Diabetes. What Impacts Glucose Levels in Your Diet. Available at https://www.joslin.org/patient-care/diabetes-education/diabetes-learning-center/what-impacts-glucose-levels-your-diet. Last accessed November 3, 2025.
72. American Diabetes Association, Bantle JP, Wylie-Rosett J, et al. Nutrition recommendations and interventions for diabetes: a position statement of the American Diabetes Association. Diabetes Care. 2008;31(Suppl 1):S61-S78.
73. Morris SF, Wylie-Rosett J. Medical nutrition therapy: a key to diabetes management and prevention. Clinical Diabetes. 2010;28(1):12-18.
74. Franz MJ, Powers MA, Leontos C, et al. The evidence for medical nutrition therapy for type 1 and type 2 diabetes in adults. J Am Diet Assoc. 2010;110(12):1852-1889.
75. DGA. Dietary Guidelines for Americans, 2020-2025 and Online Materials. Available at https://www.dietaryguidelines.gov/resources/2020-2025-dietary-guidelines-online-materials. Last accessed November 3, 2025.
76. U.S. Department of Agriculture MyPlate. Eat Healthy With MyPlate. Available at https://www.myplate.gov/. Last accessed November 3, 2025.
77. American Diabetes Association. Nutrition for Life: Diabetes Plate Method. Available at https://professional.diabetes.org/sites/dpro/files/2023-12/plan_your_plate.pdf. Last accessed November 3, 2025.
78. Evert AB, Boucher JL, Cypress M, et al. Nutrition therapy recommendations for the management of adults with diabetes. Diabetes Care. 2013;36(11):3821-3842.
79. Evert AB, Dennison M, Gardner CD, et al. Nutrition therapy for adults with diabetes or prediabetes: a consensus report. Diabetes Care. 2019;42(5):731-754.
80. Mayo Clinic. Tips for Prediabetes and Diabetes Meal Planning. Available at https://newsnetwork.mayoclinic.org/discussion/tips-for-prediabetes-and-diabetes-meal-planning/. Last accessed November 3, 2025.
81. Pedersen SD, Kang J, Kline GA. Portion control plate for weight loss in obese patients with type 2 diabetes mellitus: a controlled clinical trial. Arch Intern Med. 2007;167(12):1277-1283.
82. Rizor H, Smith M, Thomas K, Harker J, Rich M. Have you tried the Idaho plate method? DCE Newsflash. 1996;17:18-20.
84. University of Idaho. Healthy Diabetes Plate, 2nd Edition. Available at https://marketplace.uidaho.edu/C20272_ustores/web/product_detail.jsp?PRODUCTID=2675. Last accessed November 3, 2025.
85. Idaho Plate Method. Plate Method. Available at http://www.platemethod.com. Last accessed November 3, 2025.
86. Seagle HM, Strain GW, Makris A, Reeves RS, American Dietetic Association. Position of the American Dietetic Association: weight management. J Am Diet Assoc. 2009;109(2):330-346.
87. American Diabetes Association. Non-Starchy Vegetables for Blood Glucose Control. Available at https://diabetes.org/food-nutrition/reading-food-labels/non-starchy-vegetables. Last accessed November 3, 2025.
88. American Diabetes Association. Oral and Injectable Medications for Type 2 Diabetes. Available at https://diabetes.org/health-wellness/medication/oral-other-injectable-diabetes-medications. Last accessed November 3, 2025.
89. Joslin Diabetes Center. Clinical Guideline for Management of Adults with Diabetes. Available at https://joslin.org/-/media/files/joslin/joslin-clinical-guidelines-for-management-of-adults-with-diabetes.pdf. Last accessed November 3, 2025.
90. Kahn SE, Haffner SM, Heise MA, et al. Glycemic durability of rosiglitazone, metformin, or glyburide monotherapy. N Engl J Med. 2006;355(23):2427-2443.
91. GlaxoSmithKline. Highlights of Prescribing Information: Avandia. Available at https://www.gsksource.com/pharma/content/dam/GlaxoSmithKline/US/en/Prescribing_Information/Avandia/pdf/AVANDIA-PI-MG.PDF. Last accessed November 3, 2025.
92. Hiatt WR, Kaul S, Smith RJ. The cardiovascular safety of diabetes drugs: insights from the rosiglitazone experience. NEJM. 2013;369(14):1285-1287.
94. Wallach JD, Wang K, Zhang AD, et al. Updating insights into rosiglitazone and cardiovascular risk through shared data: individual patient and summary level meta-analyses. BMJ. 2020;368:I7078.
95. U.S. Food and Drug Administration. FDA Drug Safety Communication: Updated Risk Evaluation and Mitigation Strategy (REMS) to Restrict Access to Rosiglitazone-containing Medicines including Avandia, Avandamet, and Avandaryl. Available at https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-updated-risk-evaluation-and-mitigation-strategy-rems-restrict-access. Last accessed November 3, 2025.
96. U.S. Food and Drug Administration. FDA Drug Safety Communication: FDA Requires Removal of Some Prescribing and Dispensing Restrictions for Rosiglitazone-containing Diabetes Medicines. Available at https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-requires-removal-some-prescribing-and-dispensing-restrictions. Last accessed November 3, 2025.
97. U.S. Food and Drug Administration. FDA Drug Safety Communication: FDA Eliminates the Risk Evaluation and Mitigation Strategy (REMS) for Rosiglitazone-Containing Diabetes Medicines. Available at https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-eliminates-risk-evaluation-and-mitigation-strategy-rems. Last accessed November 3, 2025.
99. Daily Med. Available at https://dailymed.nlm.nih.gov/dailymed/index.cfm. Last accessed October 15, 2025.
100. U.S. Food and Drug Administration. Archive: Press Release. FDA Approves Tanzeum to Treat Type 2 Diabetes. Available at https://wayback.archive-it.org/7993/20170112023843/http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm393289.htm. Last accessed November 3, 2025.
101. U.S. Food and Drug Administration. Archive: Press Release. FDA Approves Trulicity to Treat Type 2 Diabetes. Available at https://wayback.archive-it.org/7993/20170112023822/http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm415180.htm. Last accessed November 3, 2025.
102. U.S. Pharmacist. FDA Approves First Oral GLP-1 for Use in Type 2 Diabetes. Available at https://www.uspharmacist.com/article/fda-approves-first-oral-glp1-for-use-in-type-2-diabetes. Last accessed November 3, 2025.
103. U.S. Food and Drug Administration. Highlights of Prescribing Information. Rybelsus (semaglutide). Available at https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/213051s000lbl.pdf. Last accessed November 3, 2025.
104. U.S. Food and Drug Administration. Archive: FDA Drug Safety Podcast. FDA Investigating Reports of Possible Increased Risk of Pancreatitis and Pre-Cancerous Findings of the Pancreas from Incretin Mimetic Drugs for Type 2 Diabetes. Available at https://wayback.archive-it.org/7993/20170722185812/https://www.fda.gov/Drugs/DrugSafety/ucm343187.htm. Last accessed November 3, 2025.
105. Buse JB, Henry RR, Han J, et al. Effects of exenatide (exendin 4) on glycemic control and weight over 30 weeks in sulfonylurea treated patients with type 2 diabetes. Diabetes Care. 2004;27:2628-2635.
106. Campbell RK, Miller S. New therapeutic horizons: mapping the future of glycemic control with incretin-based therapies. Diabetes Educ. 2009;35(5):731-734, 738-740, 742-744.
107. Merck & Co. Medication Guide: Januvia. Available at https://www.merck.com/product/usa/pi_circulars/j/januvia/januvia_mg.pdf. Last accessed November 3, 2025.
108. Bristol-Myers Squibb. Onglyza. Available at https://www.onglyza.com. Last accessed November 3, 2025.
109. U.S. Food and Drug Administration. Archive: Press Release. FDA Approves Three New Drug Treatments for Type 2 Diabetes. Available at https://wayback.archive-it.org/7993/20170112023907/http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm336942.htm. Last accessed November 3, 2025.
110. DailyMed. SymlinPen. Available at https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=4aea30ff-eb0d-45c1-b114-3127966328ff. Last accessed November 3, 2025.
111. U.S. Food and Drug Administration. Archive: Press Release. FDA Approves Invokana to Treat Type 2 Diabetes. Available at https://wayback.archive-it.org/7993/20170112023858/http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm345848.htm. Last accessed November 3, 2025.
112. U.S. Food and Drug Administration. Archive: Press Release. FDA Approves Farxiga to Treat Type 2 Diabetes. Available at https://wayback.archive-it.org/7993/20170112023850/http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm380829.htm. Last accessed November 3, 2025.
113. U.S. Food and Drug Administration. Archive: Press Release. FDA Approves Jardiance to Treat Type 2 Diabetes. Available at https://wayback.archive-it.org/7993/20170112023827/http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm407637.htm. Last accessed November 3, 2025.
114. Pfizer. FDA Approves SGLT2 Inhibitor STEGLATRO (ertugliflozin) and Fixed-Dose Combination STEGLUJAN (ertugliflozin and sitagliptin) for Adults with Type 2 Diabetes. Available at https://www.pfizer.com/news/press-release/press-release-detail/fda_approves_sglt2_inhibitor_steglatro_ertugliflozin_and_fixed_dose_combination_steglujan_ertugliflozin_and_sitagliptin_for_adults_with_type_2_diabetes. Last accessed November 3, 2025.
115. U.S. Food and Drug Administration. Archive: Safety Announcement. FDA Warns about Rare Occurrences of a Serious Infection of the Genital Area with SGLT2 Inhibitors for Diabetes. Available at https://wayback.archive-it.org/7993/20190207173939/https://www.fda.gov/Drugs/DrugSafety/ucm617360.htm. Last accessed November 3, 2025.
116. Fonseca V. Oxford American Endocrinology Library: Improving Patient Care. New York, NY: Oxford University Press; 2009.
117. American Diabetes Association. Low Blood Glucose (Hypoglycemia). Available at https://diabetes.org/living-with-diabetes/hypoglycemia-low-blood-glucose. Last accessed November 3, 2025.
118. U.S. Food and Drug Administration. Archive: Press Release. FDA Approves Afrezza to Treat Diabetes. Available at https://wayback.archive-it.org/7993/20170112222845/http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm403122.htm. Last accessed November 3, 2025.
119. U.S. Food and Drug Administration. Highlights of Prescribing Information. Afrezza. Available at https://www.accessdata.fda.gov/drugsatfda_docs/label/2014/022472lbl.pdf. Last accessed November 3, 2025.
120. American Diabetes Association. Insulin administration. Diabetes Care. 2003;26(Suppl 1):S121-S124.
121. American Diabetes Association. Insulin Storage and Syringe Safety. Available at https://diabetes.org/health-wellness/medication/insulin-storage-and-syringe-safety. Last accessed November 3, 2025.
122. American Diabetes Association. Devices and Technology: Better Blood Glucose Meters and More. Available at https://diabetes.org/about-diabetes/devices-technology. Last accessed November 3, 2025.
123. U.S. Food and Drug Administration. Archive: Press Release. FDA Approves First Automated Insulin Delivery Device for Type 1 Diabetes. Available at https://wayback.archive-it.org/7993/20170111083713/http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm522974.htm. Last accessed November 3, 2025.
124. Medtronic. The MiniMed 770G System Discontinuation. Available at https://www.medtronicdiabetes.com/products/minimed-770g-insulin-pump-system. last accessed November 3, 2025.
125. Medtronic. Minimed. Available at https://www.medtronicdiabetes.com/products/minimed-780g-insulin-pump-system. last accessed November 3, 2025.
126. American Diabetes Association. Continuous subcutaneous insulin infusion. Diabetes Care. 2004;27(Suppl 1):S110.
127. Colberg SR, Sigal RJ, Yardley JE, et al. Physical activity/exercise and 2 diabetes: a position statement from the American Diabetes Association. Diabetes Care. 2016;39(11):2065-2079.
128. Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39(8):1423-1434.
129. Mavros Y, Kay S, Anderberg KA, et al. Changes in insulin resistance and HbA1c are related to exercise-mediated changes in body composition in adults with type 2 diabetes: interim outcomes from the GREAT2DO trial. Diabetes Care. 2013;36(8):2372-2379.
130. McDermott K, Fang M, Boulton AJM, Selvin E, Hicks CW. Etiology, epidemiology, and disparities in the burden of diabetic foot ulcers. Diabetes Care. 202346(1):209-221.
132. American Diabetes Association. Preventive foot care in diabetes. Diabetes Care. 2004;27(Suppl 1):S63-S64.
133. Bronze MS. Diabetic Foot Infections. Available at https://emedicine.medscape.com/article/237378-overview. Last accessed November 3, 2025.
Mention of commercial products does not indicate endorsement.