Acupoint therapies have existed for thousands of years and are commonly practiced around the world. Patients may seek clarification regarding the various acupoint techniques used today, including information on safety and effectiveness. Healthcare professionals should be well informed about these practices so that they can provide evidence-based recommendations on the use of these treatments.
This course is designed for healthcare professionals whose patients are using or are interested in using acupoint and/or acupressure therapies.
The purpose of this course is to provide healthcare professionals in all practice settings the knowledge necessary to increase their understanding of acupoint and acupressure therapies.
Upon completion of this course, you should be able to:
- Describe the principles from traditional Chinese medicine (TCM) that guide the practice of acupuncture and some related acupoint therapies.
- Outline the various techniques of and available evidence regarding acupuncture.
- Discuss the approaches to and evidence of moxibustion.
- Review available research and techniques of acupressure.
- Identify uses and safety concerns of transcutaneous electrical acustimulation (TEAS).
- Compare and contrast the various acupoint techniques in terms of clinical uses and safety.
Chelsey McIntyre, PharmD, is a clinical pharmacist who specializes in drug information, literature analysis, and medical writing. She earned her Bachelor of Science degree in Genetics from the University of California, Davis. She then went on to complete her PharmD at Creighton University, followed by a clinical residency at the Children’s Hospital of Philadelphia (CHOP). Dr. McIntyre held the position of Drug Information and Policy Development Pharmacist at CHOP until her move to Washington state in 2017, after which she spent the next six years as a clinical editor for Natural Medicines, a clinical reference database focused on natural products and alternative therapies. She continues to create rigorous professional analysis and patient education materials for various publications while also practicing as a hospital pharmacist. Her professional interests include provider and patient education, as well as the application of evidence-based research to patient care.
Contributing faculty, Chelsey McIntyre, PharmD, has disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
John V. Jurica, MD, MPH
Mary Franks, MSN, APRN, FNP-C
Alice Yick Flanagan, PhD, MSW
Margaret Donohue, PhD
The division planners have disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
Sarah Campbell
The Director of Development and Academic Affairs has disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
The purpose of NetCE is to provide challenging curricula to assist healthcare professionals to raise their levels of expertise while fulfilling their continuing education requirements, thereby improving the quality of healthcare.
Our contributing faculty members have taken care to ensure that the information and recommendations are accurate and compatible with the standards generally accepted at the time of publication. The publisher disclaims any liability, loss or damage incurred as a consequence, directly or indirectly, of the use and application of any of the contents. Participants are cautioned about the potential risk of using limited knowledge when integrating new techniques into practice.
It is the policy of NetCE not to accept commercial support. Furthermore, commercial interests are prohibited from distributing or providing access to this activity to learners.
Supported browsers for Windows include Microsoft Internet Explorer 9.0 and up, Mozilla Firefox 3.0 and up, Opera 9.0 and up, and Google Chrome. Supported browsers for Macintosh include Safari, Mozilla Firefox 3.0 and up, Opera 9.0 and up, and Google Chrome. Other operating systems and browsers that include complete implementations of ECMAScript edition 3 and CSS 2.0 may work, but are not supported. Supported browsers must utilize the TLS encryption protocol v1.1 or v1.2 in order to connect to pages that require a secured HTTPS connection. TLS v1.0 is not supported.
The role of implicit biases on healthcare outcomes has become a concern, as there is some evidence that implicit biases contribute to health disparities, professionals' attitudes toward and interactions with patients, quality of care, diagnoses, and treatment decisions. This may produce differences in help-seeking, diagnoses, and ultimately treatments and interventions. Implicit biases may also unwittingly produce professional behaviors, attitudes, and interactions that reduce patients' trust and comfort with their provider, leading to earlier termination of visits and/or reduced adherence and follow-up. Disadvantaged groups are marginalized in the healthcare system and vulnerable on multiple levels; health professionals' implicit biases can further exacerbate these existing disadvantages.
Interventions or strategies designed to reduce implicit bias may be categorized as change-based or control-based. Change-based interventions focus on reducing or changing cognitive associations underlying implicit biases. These interventions might include challenging stereotypes. Conversely, control-based interventions involve reducing the effects of the implicit bias on the individual's behaviors. These strategies include increasing awareness of biased thoughts and responses. The two types of interventions are not mutually exclusive and may be used synergistically.
#98031: Getting to the Point: Acupuncture and Acupoint Therapies
Traditional Chinese medicine (TCM) began more than 3,000 years ago and has roots in shamanistic practices that resided with practitioners known as Wu [1,2]. At that time there was no scientific concept of disease or pharmacology in terms that can be related to our modern understanding of medicine. Wu shamans intertwined spirituality and healing in rituals that sought to cure disease or promote good health using special herbs and other substances and methods. Later, the formal principles of TCM were based first on Confucianism, which valued science and ethics over superstition and spirituality, and on Taoism, a philosophical and religious system of beliefs, attitudes, and practices that focuses on harmony and nature [3,4]. This ancient system of medicine encompasses a range of practices including acupoint therapies, meditation, martial arts, herbal medicine, feng shui, and massage [3].
These modalities and treatment techniques share a theoretical framework defined by the yin and yang relationship. In China, yin and yang are two forces that control the universe. Virtually all medical problems are considered to be due to imbalances in one of these forces. Chinese therapeutics intends to correct imbalances of these forces to cure disease [2,3].
Yin is the feminine side of nature and includes tranquility, darkness, cold, wetness, and depth. Yang is masculine and represents light, heat, activity, dryness, and height. Yin and yang are not the same as good and bad. Instead, they are considered complementary forces [2,3].
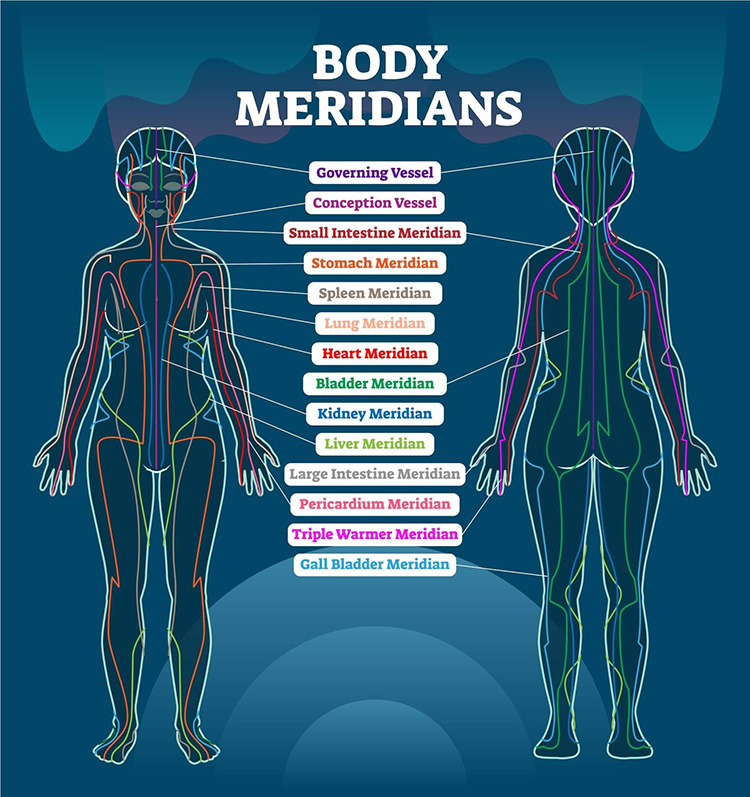
In TCM, it is thought that disease is caused by an imbalanced or blocked flow of energy, or qi. Additionally, there are 12 meridians that form a continuous pathway throughout the body; qi circulates through the body on these meridians (Figure 1).
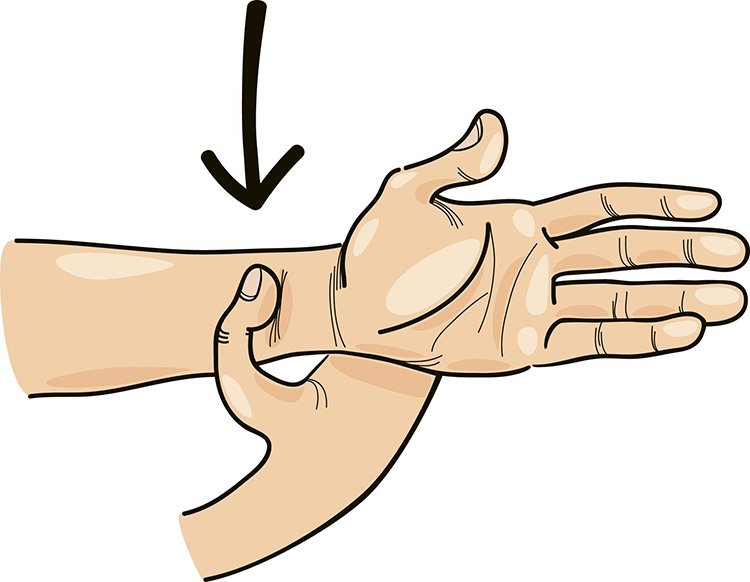
According to TCM, acupoints are specifically chosen sites of manipulation located along meridians thought to stimulate or balance specific organs, emotions, or sensory feelings. One example is the P6 acupoint, which is found on the inner forearm, two inches above the wrist joint between the two prominent tendons (Figure 2). This point is frequently used in TCM modalities for the prevention and relief of nausea and vomiting in multiple settings (e.g., chemotherapy-induced, postoperative, motion-related) [3].
There are more than 350 recognized acupoints on the human body, and each acupoint is associated with a list of conditions for which it may be used. Some practitioners may also choose to use certain acupoints for nontraditional indications [5,6].
In this practice, people are diagnosed through evaluation of the tongue and the radial pulse, and by a series of signs and symptoms unique to TCM. Although these diagnostic methods have a long history of traditional use, the findings and diagnoses achieved from these techniques do not directly correlate to Western medicine. Their use as accurate indicators of medical conditions or disease has not been validated in clinical research [3].
Pulse diagnosis and tongue diagnosis are techniques used in many traditional systems of medicine. In pulse diagnosis, practitioners assess a person's pulse for rate, strength, length, and width. The wrist is most commonly used for pulse diagnosis, and the practitioner palpates at three different pressures (superficial, middle, and deep). With tongue diagnosis, practitioners assess the tongue for color, elasticity, veining, and various other qualities. In some cases, a digital device may be used to aid in tongue diagnosis [3].
TCM modalities of acupuncture, moxibustion, acupressure, and transcutaneous electrical acustimulation (TEAS) are thought to stimulate energy flow, unblock energy, and rebalance energy, which results in healing. TCM is widely practiced in China and Taiwan, and adapted and modified forms are practiced in many Asian countries, including Cambodia, Japan, Korea, Singapore, and Vietnam. TCM has also experienced a surge in popularity in Western countries, where it is sometimes used for promoting wellness, preventing illness, and treating chronic conditions.
The practice of acupuncture originated in China more than 2,000 years ago as the primary treatment modality of TCM and involves the insertion of fine needles into specific points on the body along meridians. This acupoint therapy remains one of the most common components of TCM. So common, in fact, that many healthcare plans will cover this treatment. As of 2023, there were approximately 34,000 actively licensed acupuncturists and more than 56 accredited acupuncture and oriental medicine schools offering 147 programs in the United States, suggesting interest continues to grow [7].
Another practice of TCM, moxibustion, involves burning an herb, usually mugwort (Artemisia vulgaris), above the skin or on the acupoints to introduce heat into an acupoint for therapeutic effects. Moxibustion may be performed by burning a cone, stick, or loose herb a short distance away from the skin. Additionally, the burning herb may be placed on the head of an acupuncture needle to increase the temperature gradient of the needle. Theoretically, moxibustion opens the 12 meridians and removes cold, dampness, and stagnation, which improves consciousness and prevents the collapse of qi, particularly the yang qi[8].
Acupressure is another common treatment modality of TCM. Acupressure is similar to acupuncture; however, it involves the use of applied pressure in place of needles. Pressure is applied using hands, thumbs, fingers, or devices to specific places, or acupoints, on the body [6].
Lastly, acustimulation, another acupoint modality, involves stimulating specific acupoints on the body along meridians. TEAS involves applying a low-intensity electrical current to specific acupoints without puncturing the skin. While this modality is based on principles of TCM, it also incorporates aspects of modern practices by utilizing recently developed medical devices [9].
Although acupuncture, acupressure, and acustimulation are similar and may be used together in a single therapy session, they are individual and specific modalities and should not be confused with one another.
Additionally, TEAS differs from another therapeutic practice, transcutaneous electrical nerve stimulation (TENS), which does not utilize acupoints. It also differs from electroacupuncture, in which an electrical current is passed through embedded acupuncture needles [9].
Although a large number of clinical trials show some evidence for the use of acupoint therapies for certain conditions, their ability to show superiority to placebo controls has been contradictory and inconclusive, suggesting that benefits may be due, at least in part, to a placebo effect. This potential effect may also be due to the environment in which these therapies are conducted and the preconceived notions related to acupoint therapies.
The quality of available evidence is also important to note. Most research is limited by a lack of appropriate blinding or sham controls, unclear methodological quality (e.g., heterogeneity, publication bias), overall small sample sizes, and prior expectations of outcomes. Another limiting factor is geographical location. Most available research has been conducted in China; therefore, it is unclear if outcomes are generalizable to other regions or populations.
Sham acupoint procedures were developed to be used as a control intervention in clinical trials, similar to placebo pills used in pharmacological studies. Sham acupuncture treatments include inserting needles into non-acupoints, using a device that masks the presence or absence of a needle (such as the Park Sham Device), or poking acupoints with a toothpick rather than inserting a needle. Essentially, sham acupuncture is placebo acupuncture—it mimics the experience of acupuncture without implementing the methods thought to be responsible for its effects.
In order to mitigate some of the quality concerns commonly observed in acupoint research, investigators have developed a variety of sham acupoint procedures intended to be used as a control intervention in clinical trials. It is important to note that there are several different sham devices available, and the quality of sham design may vary between studies. Additionally, there are controversies surrounding the validity of this technique.
Acupuncture is a modality in which needles are inserted into more than 350 key points along meridians in the body. These points are referred to as acupoints, and stimulating acupoints through a needle is thought to stimulate the body to correct energy flow and balance [5].
Prior to treatment, traditional acupuncturists conduct a comprehensive medical history and examination similar to TCM practitioners. They may examine the tongue, the face, and the quality of the pulses. Both traditional and Western acupuncturists may palpate to identify points at which pressure causes tenderness or pain. Traditional acupuncturists may also add other modalities from TCM into the acupuncture therapy session [5].
Most states in the United Stated regulate the practice of acupuncture, for which different degrees and certifications are available. The National Certification Commission for Acupuncture and Oriental Medicine (NCCAOM) works with most states to validate the competency of acupuncture practitioners prior to licensure [5].
In this practice, needles are inserted into acupoints. An acupuncture session may involve the insertion of up to 20 very fine needles which are kept in place for different durations, usually about 10 to 30 minutes. The needles can be inserted to a depth of 5–40 mm and can be stimulated by winding by hand [5].
In this practice, acupuncture needles are stimulated by a weak electrical current.
In this practice, lasers are used to stimulate acupoints. A typical schedule of acupuncture administration is 6 to 12 sessions over three months [5].
In this practice, medical threads, such as catgut or polydioxanone (PDO) sutures, are inserted into subcutaneous tissue or muscle at specific points, thus providing long-term chemical stimulation in addition to the mechanical stimulation provided by traditional acupuncture. Typically, PDO threads take approximately four weeks to reach 50% tensile strength and six months to be completely absorbed [5].
Although there has been extensive research conducted on acupuncture, most data are inconclusive. Additionally, just as some research suggests evidence of benefit for certain indications, research for other indications suggests a lack of benefit.
Cancer-Related Fatigue
Low-quality studies suggest that acupuncture may modestly improve symptoms in patients with cancer-related fatigue. Guidelines from multiple oncology associations include acupuncture and electroacupuncture as a potential treatment option for reducing post-cancer fatigue [5].
Clinical research, mainly preliminary in design and low quality, shows that receiving acupuncture for a total of 6 to 10 sessions over two to ten weeks improves feelings of cancer-related mental and physical fatigue when compared with sham acupuncture or usual care alone [5].
The National Comprehensive Cancer Network (NCCN) guidelines for cancer-related fatigue list acupuncture as a potential nonpharmacologic treatment option for patients during and after treatment has been completed [8]. Additionally, the American Society of Clinical Oncology (ASCO) and the Society for Integrative Oncology recommend acupuncture for patients who have finished cancer treatment and for cancer survivors [5,11].
Cancer-Related Pain
Low-quality studies suggest that acupuncture may modestly improve symptoms in patients with cancer-related pain. Meta-analyses and preliminary clinical research, mainly low quality, show that acupuncture has a small-to-moderate effect on malignancy-related and surgery-induced pain in patients with cancer when compared with baseline or a control group. Furthermore, when used in combination with analgesics, a meta-analysis of three studies shows that electroacupuncture decreases analgesic use by a small amount [5].
The NCCN guidelines for adult cancer pain highlight acupuncture and electroacupuncture as a potential integrative treatment for vulnerable populations, such as frail or elderly individuals who may not be able to tolerate pharmacological treatments [12]. Society for Integrative Oncology/ASCO joint guidelines recommend acupuncture for pain management in patients experiencing aromatase inhibitor-related joint pain in breast cancer, general pain or musculoskeletal pain from cancer, and chemotherapy-induced peripheral neuropathy from cancer treatment [13]. Additionally, acupuncture (or acupressure) is recommended for patients undergoing cancer surgery or other cancer-related procedures (e.g., bone marrow biopsy).
Chemotherapy-Induced Nausea and Vomiting (CINV)
When used with antiemetics, some research shows that electroacupuncture, with or without manual acupuncture, modestly reduces nausea and vomiting associated with chemotherapy. Manual acupuncture alone also seems to be comparable to some antiemetics.
A clinical study in patients with advanced cancer shows that a combination of manual acupuncture and electroacupuncture with ondansetron during five days of chemotherapy reduces the severity of nausea and vomiting over a total period of 21 days when compared with sham acupuncture. However, it does not increase the number of patients that experience no nausea or vomiting [5].
Another clinical study shows that manual acupuncture is comparable to giving ondansetron 8 mg intravenously for preventing acute nausea and vomiting in the first 24 hours after chemotherapy with paclitaxel and carboplatin [5].
Clinical practice guidelines from the Society for Integrative Oncology (SIO) recommend that acupuncture or acupressure be considered as an adjunct to antiemetic medications for chemotherapy-induced nausea and vomiting (CINV) management [5].
Some experts theorize that acupuncture may result in the release of the endogenous opioids known as enkephalins and endorphins, which naturally reduce pain. However, because some research shows acupuncture to be no more effective than sham acupuncture, it is unclear if the effectiveness is due to physiologic stimulation [5].
Back Pain
Clinical research shows that acupuncture reduces pain when compared with either sham acupuncture or no treatment in patients with either chronic or acute low back pain. For chronic low back pain, most clinical research suggests that after three months, acupuncture is no more effective than sham acupuncture, although it does seem to be beneficial when compared with no treatment. Finally, there is some evidence that the analgesic effects of acupuncture may be delayed, with greatest benefit seen months after treatment discontinuation [5].
The analgesic effect of acupuncture seems to be influenced by several factors [5]:
Number of acupuncture sessions
A greater number of patients achieve relief of low back pain after 10 treatments compared to only five treatments.
Depth of needle insertion
Deep acupuncture appears to be more effective than superficial acupuncture.
Different acupuncture styles
Motion style acupuncture is a method combining acupuncture with Doin, a manual therapy used in Korean rehabilitation medicine. Research suggests that this treatment improves acute back pain to a greater degree than either traditional acupuncture or electroacupuncture [5].
Despite the uncertain and short-term benefits, guidelines published by the American College of Physicians recommend the use of nonpharmacologic therapy, such as acupuncture, prior to using pharmacologic therapy in patients with chronic low back pain [5].
Fibromyalgia
Most preliminary clinical research and meta-analyses of clinical research show that acupuncture improves pain and stiffness and quality of life when compared with no treatment, standard therapy, or sham acupuncture, although older research shows that acupuncture is no different than sham acupuncture for reducing pain [5].
This discrepancy in results might be due to the type of sham acupuncture used and the integrity of blinding procedures. Acupuncture is more effective at relieving pain when compared with the sham acupuncture method that involves placing a needle in the acupoint with a bandage, without piercing the skin. This benefit is not observed when skin is pierced in both sham and real acupuncture groups [5].
HIV/AIDS-Related Peripheral Neuropathy
Research shows that acupuncture does not improve HIV/AIDS-related peripheral neuropathy. For instance, clinical research shows that acupuncture may not be effective for reducing peripheral neuropathy associated with HIV when compared with sham acupuncture at control sites [5].
Osteoarthritis
Meta-analyses of preliminary clinical research show that electrical, laser, and manual acupuncture modestly reduce pain and modestly improve function in patients with hip or knee osteoarthritis when compared with no treatment or sham treatment, or when used as an adjunct to standard treatment. Most individual preliminary clinical trials show sustained reductions in pain for up to 12 weeks [5].
However, available research is generally of low quality and is challenged by an array of conflicting evidence. A meta-analysis of two higher quality studies and some preliminary clinical research did not find a difference between acupuncture and sham acupuncture for improving pain in hip or knee osteoarthritis. Acupuncture is conditionally recommended by The American College of Rheumatology (ACR) for any form of osteoarthritis [5].
It is important to mention that there are a number of pain-related conditions with insufficient evidence to support the use of acupuncture. These conditions include myofascial pain syndrome, shoulder pain, sciatica, pregnancy-related pain, and others. More evidence is needed to rate acupuncture for these uses [5].
Constipation
A meta-analysis of preliminary clinical research, as well as individual clinical trials, in patients with functional constipation show that receiving manual acupuncture or electroacupuncture for 2 to 10 weeks modestly increases bowel movements and improves stool formation and symptoms when compared with sham acupuncture. However, acupuncture was no more effective than various conventional medications [5].
Dyspepsia
Meta-analyses of preliminary clinical research show that manual and electroacupuncture are more effective than sham acupuncture for improving symptoms of dyspepsia and quality of life. Some individual clinical studies have shown that acupuncture combined with Western medicine (including prokinetic agents, acid suppressants, and antidepressants) improves symptoms more than Western medicine alone [5].
There are also a variety of gastrointestinal-related conditions for which there is very limited evidence to support the use of acupuncture. These conditions include gastroparesis, ulcerative colitis, irritable bowel syndrome, and postoperative ileus [5].
Postoperative Nausea and Vomiting (PONV)
Meta-analyses suggest that acupoint stimulation with acupuncture, acupressure, and electrical stimulation can reduce PONV by up to 50% and may be as effective as conventional antiemetics. Furthermore, other analyses show that acupuncture of the P6 acupoint is effective in reducing incidence of nausea, vomiting, and need for rescue antiemetics postoperatively when compared with no treatment. The effects of acupuncture on acute and delayed vomiting and nausea appear to vary [5].
A meta-analysis of six small clinical trials suggest that acupuncture reduces postoperative vomiting in children when compared with control acupuncture surgery. Additionally, one small study shows that receiving acupuncture on the P6 acupuncture point is as effective as sham acupuncture and dexamethasone [5].
Thus far, the evidence on the use of acupuncture for PONV is promising, and patients may consider it as an adjunctive treatment option. However, there is currently very limited evidence on use for pregnancy-induced and radiation-induced nausea and vomiting.
Asthma
Most research shows that acupuncture does not improve symptoms of asthma. While some preliminary clinical research suggests that acupuncture or laser acupuncture and probiotics may marginally improve asthma symptoms and pulmonary function, most clinical research supports that acupuncture has no effect on asthma or asthma parameters such as forced expiratory volume in one second and forced vital capacity [5].
Depression
When used with conventional antidepressants, most research shows that acupuncture modestly reduces symptoms of depression. However, it is unclear if acupuncture alone is more effective than conventional antidepressants.
Clinical evidence shows that using manual or electroacupuncture as an adjunct to antidepressants such as selective serotonin reuptake inhibitors modestly reduces depression severity when compared with antidepressants alone [5].
There is also some evidence that acupuncture may be more likely to alleviate symptoms of perimenopausal depression, post-stroke depression, or cancer-related depression when compared with antidepressants or hormone replacement therapy. However, because most of the available research has been conducted in China, it is unclear if these findings are generalizable to other geographic locations [5].
Insomnia
Clinical research shows that manual acupuncture modestly improves sleep quality and might reduce the need for medication when used as an adjunct to sleep hygiene instruction or conventional treatment, sham acupuncture, or a waitlist control group (i.e., a group that serves as an untreated comparator, but eventually goes on to receive treatment at a later date) [5].
Electroacupuncture does not seem to improve sleep efficiency, sleep onset, or insomnia severity when compared with conventional treatment or sham electroacupuncture [5].
Smoking Cessation
Clinical research shows that although acupuncture might have short-term benefits, it does not improve rates of long-term smoking cessation when compared with sham acupuncture [5].
Acupuncture, when used appropriately and performed with sterile needles, is generally well-tolerated and has been safely used in numerous clinical trials for up to 24 months. Some clinical research shows that acupuncture has been used in children without reports of significant adverse effects [5].
Most commonly, acupuncture is associated with dermatologic adverse effects, such as bruising, swelling, and pain. Acupuncture in the eyes can cause trauma to the eyes such as perforation and traumatic cataract. There have been case reports of epidural and subdural hematomas from improper acupuncture, resulting in paresthesia, hemiparesis, quadriparesis, and sensory deficit. There have been case reports of pneumocranium, pneumothorax, hemothorax, acute respiratory and circulatory failure, and death due to inappropriate acupuncture practices. Acupuncture needles that are not removed after treatment might embolize and cause damage to internal organs [5].
Moxibustion is another acupoint modality that is commonly utilized in TCM. Moxibustion involves burning moxa, a dried herbal preparation made of the aged, powdered mugwort herb, at prescribed acupoints on the body. These points are determined based on the patient's symptoms and diagnosis [8].
Moxa is considered to have a warming yang nature that is thought to prevent patients from experiencing a collapse of yang qi energy. There are various techniques used in moxibustion.
The ignited moxa cone does not contact the skin directly. Instead, it is separated from the skin by ingredients such as ginseng, salt, garlic, ginger, or aconite cake. In clinical research, indirect moxibustion has improved levels of cellular mediators involved in pain [8].
The ignited moxa cone is used directly to warm the skin surface at the acupuncture point. Direct moxibustion can be scarring, which involves burning moxa directly on the skin, or "warming," which involves burning moxa above the skin [8].
Moxa-cigars held by a moxibustion box are ignited over the treatment site. The fire head is held about an inch away from the skin and burned for about 30 minutes. To maintain the heat and reduce smoke in the air, the moxibustion treatment is covered with a thick towel [8].
This is an integration of acupuncture and moxibustion. A one-inch moxa stick is put on the handle of an acupuncture needle that has been inserted in the body, and the moxa stick is ignited. This method is purported to warm the meridians and promote the flow of qi and blood [8].
Electric moxibustion has been developed because there are safety concerns with traditional moxibustion, such as excessive heat or potentially toxic chemical components. Electric moxibustion has adjustable and constant heat stimulation that is applied either directly or indirectly to skin and has been shown to increase blood flow in healthy participants [8].
Involves wearing heated knee pads containing a jade stone for 20 minutes three times weekly for four weeks [8].
Back Pain
Most low-quality clinical research suggests that moxibustion, when used alone or in conjunction with other treatments, may modestly reduce back pain.
A meta-analysis of small, low quality clinical studies in people with chronic low back pain shows that moxibustion reduces pain when compared with acupuncture, massage, or taking ibuprofen 300 mg daily or celecoxib 200 mg daily. Furthermore, adding moxibustion to other treatments such as massage, acupuncture, core stability training, or the medicines celecoxib or meloxicam, further reduces back pain when compared with the active treatment alone [8].
Osteoarthritis
Meta-analyses of small clinical studies in patients with knee osteoarthritis show that moxibustion modestly reduces pain and improves function when compared with sham moxibustion or usual care. A subgroup analysis suggests that moxibustion improves osteoarthritis pain when compared with taking diclofenac, but not when compared with taking celecoxib. However, this finding is limited due to the high heterogeneity of the available research, as well as a high risk for publication bias [8].
Research has also evaluated other types of moxibustion for the treatment of knee osteoarthritis. One clinical trial shows that receiving jade moxibustion improves pain to a greater degree when compared with receiving traditional moxibustion. Another clinical study shows that receiving moxibustion in 12 sessions over six weeks via a specific electrical device (Cettum) improves pain similarly to traditional indirect moxibustion and to a greater extent than usual care [8].
In human research, moxibustion has been shown to reduce levels of certain inflammatory markers. Other preliminary data suggest that moxibustion may help to protect the gastric mucosa. Due to its perceived anti-inflammatory effects, there is interest in using this therapy for gastrointestinal-related conditions.
Moxibustion has been investigated in patients with diarrhea-predominant irritable bowel syndrome (IBS-D), constipation-predominant IBS (IBS-C), and inflammatory bowel diseases. Currently, there is not enough scientific evidence to support the use of moxibustion for Crohn disease and ulcerative colitis. Additionally, there is very limited evidence on use for constipation and gastritis.
IBS-D
Moxibustion with or without acupuncture appears to be more effective than sham moxibustion, sham acupuncture, or various pharmaceutical agents for improving abdominal pain, discomfort, gas, bloating, and stool consistency. There were also overall improvements in stool form and symptom severity [4].
Clinical research in patients with IBS-D shows that moxibustion three times weekly for six weeks produces adequate relief in about 77% to 82% of patients, compared with 37% to 42% of those given sham or placebo moxibustion. These data also suggest that beneficial effects lasted for up to an additional 18 weeks after treatment completion in up to 76% of patients [8].
Thus far, the evidence on the use of moxibustion for IBS-D is promising, and patients may consider it as an adjunctive treatment option.
IBS-C
The available research in patients with IBS-C is limited to a small clinical study showing no benefit with the use of warming moxibustion six times weekly for four weeks when compared with baseline or electroacupuncture [8]. As such, available research suggests that moxibustion may not be effective in patients with IBS-C.
Crohn Disease
Moxibustion administration has only been evaluated in combination with acupuncture; its effect when used alone is unclear. Clinical research in patients with Crohn disease shows that combining herb-partitioned moxibustion with acupuncture three times weekly for 12 weeks induces remission in 74% of patients, compared with only 36% of patients given sham moxibustion and superficial acupuncture [8].
Ulcerative Colitis
A meta-analysis of low-quality clinical research shows that moxibustion with or without acupuncture improves response rate by 24% when compared to control treatment. However, these results are limited by the small number, size, and low quality of the included studies [8].
Cancer
Moxibustion administration does not seem to be beneficial for cancer treatment. A meta-analysis of five clinical studies shows that moxibustion does not improve treatment response in patients with various cancer types when compared with standard care. There is limited evidence on use of moxibustion for CINV and cancer-related fatigue [8].
Dysmenorrhea
Low-to-moderate quality clinical research in patients with dysmenorrhea shows that moxibustion with or without acupuncture reduces pain, usually when compared with no treatment or usual care. Additional clinical research shows that moxibustion reduces pain intensity similarly to ibuprofen 300 mg twice daily for three days, starting the day before menstruation and repeated for three cycles. Furthermore, at three months after treatment discontinuation, pain intensity remains 13% lower in the patients that received moxibustion [8].
Insomnia
It is unclear if moxibustion is beneficial for insomnia. Although some research has been conducted on the use moxibustion for insomnia, there is not enough reliable evidence to confirm a benefit for these indications [8].
Moxibustion is likely safe when administered appropriately by a qualified practitioner and has been used in clinical research without reports of serious adverse events.
Most commonly, moxibustion is associated with blisters, burns, dizziness, fainting, fatigue, gastrointestinal upset, headache, hypersomnia, itching, pain, rash, redness, and respiratory discomfort. Serious cases of adverse effects caused by moxibustion are generally related to inappropriate administration, such as not removing the moxa from the skin at the appropriate time or accidentally dropping ash onto the skin [8].
Acupressure involves applying pressure using hands, thumbs, fingers, or devices to acupoints. Acupressure can be self-administered or applied by a trained practitioner. Passive acupressure devices are also available that apply pressure continuously at a specific location. For example, wrist bands can apply pressure to the P6 acupoint, which is utilized for the treatment or prevention of nausea and vomiting. Most acupressure points are located near nervous tissue or structures. Duration and frequency of acupressure treatment is individualized to the patient and the condition being treated [6].
Although there is a large body of research evaluating acupressure for various purposes, most evidence is low quality and inconclusive.
Most acupressure points are located near nervous tissue or structures. Researchers suggest that applying pressure at these points may block transmission of pain signals through certain neural gates [6].
Back Pain
Acupressure, administered either alone or as an adjuvant treatment, seems to reduce chronic low back pain. Clinical research in patients with lower back pain shows that acupressure, administered alone or with acupuncture, or acupressure massage with aromatic essential oil in combination with usual care, reduces pain and disability and improves walking ability when compared with physical therapy, usual care, or acupuncture alone [6].
Preliminary clinical research shows that using an acupressure backrest during sedentary work for one month reduces pain and disability by at least 30% when compared with no intervention. Other preliminary clinical research shows that using auricular acupressure for three minutes three times daily for five days each week for four weeks reduces pain by about 40% when compared with performing the same procedure on incorrect acupoints [6].
Auricular acupressure involves the taping of magnetic beads or plant seeds to the ear. In TCM, it is thought to relieve tension and improve circulation [6].
Osteoarthritis
Most research shows that manual acupressure does not improve pain or function in patients with knee osteoarthritis. Additionally, it is unclear if auricular acupressure is beneficial for osteoarthritis.
Clinical research in patients with osteoarthritis of the knee shows that self-administered acupressure alone for up to 16 weeks does not reduce knee pain intensity when compared with receiving sham acupressure, education on knee health, exercise, or no intervention [6].
A small clinical study shows that auricular acupressure four times daily for four weeks is associated with reductions in pain, stiffness, and function on days 3 and 7, but not days 14, 21, or 28, when compared with sham acupressure [6].
It is important to mention that there are a number of other pain-related conditions with insufficient evidence to support the use of acupressure. These conditions include neck and shoulder pain, postoperative pain, and neuropathic pain [6].
Cancer-Related Fatigue
Acupressure seems to improve fatigue in patients with cancer. A meta-analysis of mostly small clinical studies in patients with cancer-related fatigue shows that various forms of acupressure, either self-administered or administered by a professional, reduces fatigue by a large amount when compared with usual care, sham acupressure, or acupuncture [6].
Thus far, the evidence on the use of acupressure for cancer-related fatigue is promising, and patients may consider acupressure as an adjunctive treatment option. However, there is very limited evidence on use for breast cancer, cancer-related pain, and chemotherapy-related fatigue [6].
Chemotherapy-Induced Nausea and Vomiting (CINV)
It is unclear if acupressure is beneficial in patients with CINV. Data are conflicting.
Some research, but not all, suggests that acupressure modestly reduces chemotherapy-induced acute and delayed nausea, but not acute or delayed vomiting. Research using acupressure wristbands for CINV is also mixed; some research shows that using a specific passive acupressure wristband product (Sea-Band) reduces nausea and vomiting when compared with usual care alone, but it does not appear to be more effective than sham acupressure [6].
The reasons for these mixed findings may be related to the type of cancer, the chemotherapy regimen used, or the severity of CINV. Larger, higher quality studies are needed to determine which patients, if any, may benefit the most from treatment.
Dysmenorrhea
Acupressure seems to reduce pain in adults and adolescents with primary dysmenorrhea. Preliminary clinical research in adolescents with primary dysmenorrhea shows that beginning acupressure shortly after menstruation onset reduces the severity of dysmenorrhea for up to two hours after treatment and improves pain and anxiety. Self-administration of acupressure also seems to help reduce pain in dysmenorrhea [3].
Insomnia
Some small clinical studies suggest that manual and auricular acupressure improves sleep in patients with insomnia or sleep disturbances due to various underlying conditions.
Improvement in sleep was reported in small clinical studies, particularly in patients with hypertension or cancer, individuals who receive routine hemodialysis, and patients who are hospitalized or residing in long term care. Larger, higher quality studies are needed to determine which patients are more likely to benefit from treatment [6].
Motion Sickness
It is unclear if acupressure is beneficial in patients with motion sickness. Some clinical research shows that acupressure does not reduce motion sickness in elderly patients, females, or male college students. However, other research in experimentally induced motion sickness shows that acupressure at the P6 point reduces nausea when compared with baseline but has mixed findings when compared with sham acupressure [6].
There are a number of other conditions with insufficient evidence to support the use of acupressure. Some examples include, but are not limited to, PONV, smoking cessation, and irritable bowel syndrome (IBS) [6].
Acupressure in adults and children appears well tolerated when applied appropriately and has been safely used in numerous clinical trials. Most commonly, acupressure is associated with bruising, dizziness, headache, inflammation, and skin irritation [6].
TEAS involves applying low-intensity electrical current to specific acupoints without puncturing the skin. TEAS can be given using electric units with a transcutaneous electrical nerve stimulation (TENS) unit or a Han's acupoint nerve stimulator (HANS) dual-channel unit. The electrodes are attached to specific acupoints on the body to which a small electric current is administered. Common currents include 2–100 Hz in constant or pulsed mode [9].
A specific acustimulation device (ReliefBand) has been used with apparent safety in clinical research with no reports of adverse effects. This device is commercially available and cleared by the U.S. Food and Drug Administration (FDA) for certain types of nausea, retching, and vomiting [9]. Note that FDA clearance and FDA approval are not interchangeable terms. "FDA cleared" typically refers to medical devices, which differs from the rigorous testing required for "FDA approval," which is generally applied to pharmaceutical drugs.
Common acupoints used for acustimulation are the P6 Neiguan point on the wrist, which is used for nausea and vomiting, and the ST36 Zusanli point below the knee, which is used for gastrointestinal discomfort, stress, and fatigue. These and other acupoints have been stimulated alone or in combination in clinical research [9].
Sessions normally last for 30 to 60 minutes and are conducted two to seven days per week for 2 to 12 weeks, or as multiple sessions daily. Occasionally, acustimulation is used in surgical patients, and may be administered prior to, during, and/or daily for up to three days after surgery [9].
Acustimulation does not seem to be beneficial for CINV. Several clinical trials including patients with breast and liver cancer receiving highly emetogenic chemotherapy such as cisplatin or doxorubicin shows that acustimulation, administered by wearing a specific acustimulation device (ReliefBand) or given via electrodes does not improve CINV when compared with not wearing the device, wearing the device incorrectly, wearing acupressure bands, or sham acustimulation [9].
Additionally, there is insufficient evidence to support the use of TEAS in patients with fatigue or constipation related to chemotherapy [9].
Postoperative Cognitive Dysfunction
Acustimulation seems to be beneficial for preventing postoperative cognitive dysfunction. A meta-analysis of generally good quality clinical research shows that acustimulation, alone or in combination with other therapies, reduces the incidence of postoperative cognitive dysfunction in the first week after surgery by approximately 60% when compared with control groups given sham intervention, no intervention, or other treatments. Although there were also improvements seven days after surgery, these benefits were not observed on day five [9].
Additional preliminary clinical research in elderly patients undergoing laparoscopic cancer surgery shows that acustimulation from 30 minutes before anesthesia induction to the end of surgery modestly reduces the cumulative duration of cognitive decline on postoperative days two and three when compared with no acustimulation. However, there was no effect on the incidence of cognitive decline [9].
Postoperative Ileus
Acustimulation seems to be beneficial for preventing postoperative ileus. A meta-analysis and individual clinical research show that acustimulation modestly improves the time to first flatus or first defecation, the number of spontaneous bowel movements, symptoms such as appetite, belching, and abdominal distension, and the overall incidence of postoperative ileus or gastrointestinal dysfunction when compared with sham acustimulation or routine treatment alone [9].
Acustimulation has been given during or after the operation until postoperative day three for cesarean section, gastric surgery, and colorectal surgery [9].
Postoperative Nausea and Vomiting (PONV)
Acustimulation seems to be effective for preventing PONV; however, it is unclear whether acustimulation is effective for treating PONV or whether it is more effective than antiemetics alone for preventing PONV.
Most clinical research from meta-analyses and individual trials shows that acustimulation reduces the risk of PONV by up to 46% for at least 2 hours, and in some cases for up to 48 hours, after surgery. In addition, a meta-analysis of four studies shows that acustimulation at the P6 acupoint reduces the need for antiemetic rescue [9].
Many studies used acustimulation of the P6 point starting before anesthesia and continuing for up to 72 hours after surgery using a specific acustimulation band (ReliefBand) or HANS electrodes. This device has shown benefit for PONV after gynecological laparoscopy, laparoscopic cholecystectomy, and plastic surgery and appears to be most effective for preventing PONV when used perioperatively and postoperatively as opposed to only preoperative use [9].
Other clinical research in children 4 to 12 years of age undergoing tonsillectomy shows that acustimulation of 20 Hz for five minutes before the induction of anesthesia and five minutes after surgery is as effective as ondansetron 0.15 mg/kg and more effective than no treatment for reducing the incidence of postoperative retching and vomiting on the day of surgery and the day after discharge, but not immediately after surgery or on postoperative day one [9].
Postoperative Pain
Acustimulation seems to be effective for reducing postoperative pain for certain surgeries. Clinical research shows that acustimulation modestly reduces postoperative pain and/or the need for postoperative analgesics when compared with sham acustimulation or routine treatment alone. Types of surgery have included caesarian section, inguinal hernia repair, thoracoscopic surgery, spinal cord surgery, total hip arthroplasty, radical mastectomy, ureteroscopic lithotripsy, gastrectomy, and others. In some cases, acustimulation is initiated prior to, and possibly during, surgery, as well as intermittently after surgery. In others it has only been used postoperatively for up to three days [9].
However, not all research agrees. When used in combination with the antiemetics dexamethasone and tropisetron in female patients undergoing laparoscopic sleeve gastrectomy, acustimulation does not reduce postoperative pain over 48 hours or the need for opioid medication [9].
There is very limited evidence on use for acustimulation in patients with acute or chronic pain. Additionally, it is unclear if acustimulation is beneficial in patients with neck pain or if it improves pain during labor [9].
TEAS is generally well tolerated when used appropriately, short-term. Acustimulation via other methods has also been used with apparent safety in clinical research for up to 12 weeks [9].
Until more is known about the safety of acupuncture, moxibustion, acupressure, or TEAS during in vitro fertilization (IVF), recommend against the use of these modalities [5,6,8,9].
Acupuncture
Some clinical research shows that acupuncture has been used during pregnancy and labor without reports of significant adverse effects when used appropriately at most acupoints and performed with sterile needles. There is insufficient reliable information available about the use of electroacupuncture or laser acupuncture during pregnancy; avoid using. There is some concern that acupuncture at the SP6 acupoint on the inner ankle can increase the risk of early contractions and miscarriage [5].
Acupressure
This therapy has been safely used during pregnancy in clinical trials without significant adverse effects [6].
Transcutaneous Electrical Acustimulation (TEAS)
There is currently insufficient reliable information available; however, there is no reason to expect safety concerns when used appropriately [9].
Moxibustion
While this therapy has been used with apparent safety during pregnancy in most clinical studies, some clinical evidence suggests that moxibustion may be associated with premature birth, premature membrane rupture, increased rate of contractions, abdominal pain due to contractions, placental bleeding, reduced or increased fetal movement, and reduced fetal heart rate [8].
There is insufficient reliable information available about the use of moxibustion during lactation; however, it is unlikely that maternal use of moxibustion would pose a significant safety risk to breastfeeding infants [8].
Theoretically, moxibustion may exacerbate asthma symptoms. Clinical reports of respiratory discomfort and asthma exacerbation due to the smoke associated with moxibustion suggest that moxibustion may not be safe for use in patients with asthma. However, some research has suggested a possible beneficial effect of moxibustion in patients with asthma. Until more is known, use with caution [8].
Although there are no absolute contraindications, it is imperative that acupoint practitioners are fully informed on a patient's health history to ensure safety during treatment. Examples of conditions to watch out for include altered mental status, hemophilia, and needle phobia. Patients should inform their acupoint practitioners regarding any implanted devices, such as pacemakers. Additionally, dermatologic conditions such as cellulitis, burns, or ulcerations should be evaluated prior to treatment [5,6,8,9].
Because these acupoint modalities share similar characteristics and may be used together in a therapy session, patients may have questions regarding specific therapies and their efficacy for specific indications.
Although multiple acupoint therapies have been evaluated for back pain, the study structures and comparators used in this research has varied widely.
Acupuncture
Most research shows that acupuncture seems to reduce back pain more than no treatment. However, it is unclear if acupuncture is more effective than sham acupuncture. Receiving more than five treatments with deep acupuncture seems to offer the most long-term benefit [5].
Moxibustion
Low-quality clinical research shows that moxibustion reduces back pain when compared with acupuncture, massage, or taking ibuprofen or celecoxib. Furthermore, adding moxibustion to other treatments such as massage, acupuncture, core stability training, or the medicines celecoxib or meloxicam, further reduces back pain when compared with the active treatment alone [8].
Acupressure
Clinical research in patients with lower back pain shows that acupressure, used alone or with acupuncture, or acupressure massage with aromatic essential oil in combination with usual care reduces pain and disability and improves walking ability when compared with physical therapy, usual care, or acupuncture alone [6].
Acupuncture, acupressure, and moxibustion have a growing body of evidence suggesting at least modest benefit for back pain. TEAS has not yet been adequately evaluated for this purpose [5,6,8,9].
Although multiple acupoint therapies have been evaluated for insomnia, research has varied widely. Take note of the differences in study structures and patient populations.
Acupuncture and acupressure have a growing body of evidence suggesting at least modest benefit for insomnia. There is currently insufficient evidence to rate the effectiveness of moxibustion for this condition; larger, higher quality studies are needed. TEAS has not yet been adequately evaluated for this purpose.
Acupuncture
Clinical research shows that manual acupuncture modestly improves sleep quality and might reduce the need for medication when used as an adjunct to sleep hygiene instruction or conventional treatment, sham acupuncture, or waitlist control [5].
Acupressure
Most small clinical studies suggest that manual and auricular acupressure modestly improves sleep in patients with insomnia or sleep disturbances due to various underlying conditions including patients with hypertension or cancer, those who are hospitalized or residing in long term care, or those receiving hemodialysis [6].
Moxibustion
Although some research has been conducted on the use of moxibustion for insomnia, there is not enough reliable evidence to confirm a benefit for these indications [8].
Although multiple acupoint therapies have been evaluated for osteoarthritis, the affected joints, as well as the comparators used in clinical studies, have varied widely.
Acupuncture has a growing body of evidence suggesting at least modest benefit for patients with knee or hip osteoarthritis. Some research suggests moxibustion is beneficial for knee osteoarthritis, but it is unclear how it compares to the use of other therapies.
Most research shows that manual acupressure does not improve pain or function in patients with knee osteoarthritis. TEAS has not yet been adequately evaluated for this purpose.
Acupuncture
Meta-analyses of preliminary clinical research show that electrical, laser, and manual acupuncture modestly reduce pain and modestly improves function in patients with hip or knee osteoarthritis when compared with no treatment and sham treatment and when used as an adjunct to standard treatment. Furthermore, most individual preliminary clinical trials show that acupuncture is more effective than control treatments, such as advice or sham acupuncture, for reducing pain in knee and hip osteoarthritis for up to 12 weeks. Acupuncture is conditionally recommended by the ACR for any form of osteoarthritis [5].
Moxibustion
Meta-analyses of small clinical studies in patients with knee osteoarthritis show that moxibustion modestly reduces pain and improves function when compared with sham moxibustion or usual care. A subgroup analysis suggests that moxibustion improves osteoarthritis pain when compared with taking diclofenac, but not when compared with taking celecoxib; however, these findings are uncertain [8].
Acupressure
Most research in patients with osteoarthritis of the knee shows that self-administered acupressure alone for up to 16 weeks does not reduce knee pain intensity when compared with receiving sham acupressure, education on knee health, exercise, or no intervention [6].
Although multiple acupoint therapies have been evaluated for PONV, the study structures and comparators used in this research has varied widely. Acupuncture and TEAS have a growing body of evidence suggesting at least modest benefit at preventing PONV. Currently, there is insufficient evidence to support the use of acupressure in this setting. Moxibustion has not yet been adequately evaluated for this purpose.
Acupuncture
Some meta-analyses suggest that acupoint stimulation with acupuncture, acupressure, and electrical stimulation can reduce postoperative nausea and vomiting by up to 50% and may be as effective as conventional antiemetics. Furthermore, other analyses show that acupuncture of the P6 acupoint is effective in reducing incidence of nausea, vomiting, and need for rescue antiemetics postoperatively when compared with no treatment [5]. However, a 2023 meta-analysis and several other studies found only a reduction in postoperative nausea but not vomiting, and yet others found that within the first six hours following surgery acute vomiting was reduced but acute nausea was not. These results are largely from small-scale, low-quality studies.
TEAS
Acustimulation seems to be effective for preventing PONV; however, it is unclear whether acustimulation is effective for treating PONV or whether it is more effective than antiemetics alone for preventing PONV [9].
For patients who are not proficient in English, it is important that information regarding the benefits and risks associated with acupoint therapies be provided in their native language, if possible. When there is an obvious disconnect in the communication process between the practitioner and patient due to the patient's lack of proficiency in the English language, an interpreter is required. Interpreters can be a valuable resource to help bridge the communication and cultural gap between patients and practitioners. Interpreters are more than passive agents who translate and transmit information back and forth from party to party. When they are enlisted and treated as part of the interdisciplinary clinical team, they serve as cultural brokers who ultimately enhance the clinical encounter.
The popular practice of acupuncture has existed for centuries, with records dating back thousands of years. Acupuncture and related acupoint modalities are widely used on a global scale and continue to grow in popularity as patients seek alternative treatments for various acute and chronic medical conditions. Similarities between these modalities may make it difficult to decipher the effectiveness of individual treatments for certain conditions.
Additionally, quality of evidence remains a concern. The evidence supporting the use of acupoint therapies remains limited to low-quality research. Larger, higher quality studies are needed to determine which patients, if any, are most likely to benefit, and how these treatments compare to the use of other therapies.
Further, no treatment is without safety concerns, including adverse effects, condition interactions, and special considerations. It is imperative that clinicians provide accurate information regarding various acupoint therapies and evidence-based recommendations to help patients make informed decisions about their health.
1. National Center for Complementary and Integrative Health. Traditional Chinese Medicine: What You Need to Know. Available at https://www.nccih.nih.gov/health/traditional-chinese-medicine-what-you-need-to-know. Last accessed October 22, 2025.
2. National Library of Medicine. Traditional Chinese Medicine. Available at https://www.nlm.nih.gov/hmd/topics/chinese-traditional/index.html. Last accessed October 22, 2025.
3. TRC Healthcare Natural Medicines Database. Traditional Chinese Medicine (TCM). Available at https://naturalmedicines.therapeuticresearch.com/Data/ProMonographs/Traditional-Chinese-Medicine-TCM. Last accessed October 24, 2025.
4. Ferreira M. Confucianism and Traditional Chinese Medicine. Available at https://www.traditionalbodywork.com/confucianism-and-traditional-chinese-medicine-tcm. Last accessed October 24, 2025.
5. TRC Healthcare Natural Medicines Database. Acupuncture. Available at https://naturalmedicines.therapeuticresearch.com/Data/ProMonographs/Acupuncture. Last accessed October 24, 2025.
6. TRC Healthcare Natural Medicines Database. Acupressure. Available at https://naturalmedicines.therapeuticresearch.com/Data/ProMonographs/Acupressure. Last accessed October 24, 2025.
7. Fan AY, He DG, Sangraula A, Faggert Alemi S, Matecki A. Distribution of licensed acupuncturists and educational institutions in the United States at the start of 2023, during the late stage of the COVID-19 pandemic. J Integr Med. 2024;22(4):379-384.
8. TRC Healthcare Natural Medicines Database. Moxibustion. Available at https://naturalmedicines.therapeuticresearch.com/Data/ProMonographs/Moxibustion. Last accessed October 24, 2025.
9. TRC Healthcare Natural Medicines Database. Transcutaneous Electrical Acustimulation. Available at https://naturalmedicines.therapeuticresearch.com/Data/ProMonographs/Transcutaneous-Electrical-Acustimulation. Last accessed October 24, 2025.
10. National Comprehensive Cancer Network. Cancer-Related Fatigue (Version 1.2026). Available at https://www.nccn.org/professionals/physician_gls/pdf/fatigue.pdf. Last accessed October 22, 2025.
11. Mustian K, Lacchetti C, Zick S, Bower JE. Management of fatigue in adult survivors of cancer: American Society of Clinical Oncology - Society for Integrative Oncology (ASCO-SIO) guideline update clinical insights. JCO Oncol Pract. 2024;20(12):1575-1579.
12. National Comprehensive Cancer Network. Adult Cancer Pain (Version 2.2025). Available at https://www.nccn.org/professionals/physician_gls/pdf/pain.pdf. Last accessed October 22, 2025.
Mention of commercial products does not indicate endorsement.